Evaluation of the neutrophil-lymphocyte ratio, platelet-lymphocyte ratio and monocyte lymphocyte ratio for diagnosis of testicular torsion
Cihan Bedel, Mustafa Korkut
Department of Emergency Medicine, Antalya Training and Research Hospital, Health Science University, Antalya, Turkey
ABSTRACT Objective: To explore the value of complete blood count (CBC),including neutrophil-lymphocyte ratio (NLR), platelet-lymphocyte ratio (PLR), and monocyte lymphocyte ratio (MLR) in diagnosis of testicular torsion (TT) and differential diagnosis from epididymo-orchitis.Methods: The study was conducted at the Antalya Training and Research Hospital Emergency Department in Turkey with acute scrotal pain patients from January 1st, 2016 to January 1st, 2018.The patients were categorized into 3 groups: the TT group who underwent an operation for TT (n=70), the epididymo-orchitis group who received epididymo-orchitis treatment (n=120), and the healthy control group (n=100). NLR, PLR, and MLR of the three groups were analysed and compared. The optimum cut-off values of NLR, MLR, and PLR were analyzed.Results: Mean NLR and MLR values were significantly higher in the epididymo-orchitis group and the TT group compared to the control group (P<0.001). Receiver operating characteristic analysis revealed a sensitivity of 77.1% and a specificity of 80% for NLR(77.1) and a sensitivity of 68.2% and a specificity of 78% for PLR(124.80). Moreover, when MLR was used to differentiate the two treatment groups, the optimal cut-off value had a sensitivity of 67.1% and a specificity of 75% (AUC: 0.677-0.826, P<0.001).Conclusions: NLR, PLR, and MLR might be associated with the diagnosis of TT. These parameters provide a useful and economical method to help diagnose TT in the emergency department.
KEYWORDS: Testicular torsion; Epididymo-orchitis; Monocyte lymphocyte ratio; Emergency department
1. Introduction
Testicular torsion (TT) is one of the most common causes of acute scrotum pain requiring urgent treatment. It leads to impaired blood flow in the testis and testicular ischemia as a result of the spermatic cord rotating around its longitudinal axis[1]. TT typically presents with testicular sensitivity, pain, and associated symptoms such as nausea and vomiting. The incidence of TT in men under 25 years is approximately 1:4 000[1,2]. If it is treated within 6 h after pain occurs, there is a good chance (90%-100%) to save the affected testicle. If treated within 6 h-12 h, depending on the degree of the torsion, 20%-50% testicles will be saved, while treated within 12 h-24 h, only 0%-10% testicles will be saved. Actually, TT can occur at any age but usually occurs in young males, with a bimodal incidence in the pediatric population: during the first year of life,and between the ages of 13 and 16 years[3,4].
Epididymo-orchitis has similar symptoms to TT, and differential diagnosis is needful. Evaluation of acute scrotal pathologies should include a detailed medical history and physical examination of the genital area. However, obtaining a medical history and physical examination may sometimes not be sufficient for a definitive diagnosis[5,6]. The most frequently used imaging modality for differential diagnosis is scrotal Doppler ultrasonography (USG)[7].However, USG is time-consuming or unavailable in emergency situations so that clinical decision-making is difficult in these cases.Therefore, faster and available methods for the diagnosis of TT are needed.
Recently, as inflammatory hematological parameters, neutrophillymphocyte ratio (NLR), platelet-lymphocyte ratio (PLR), and monocyte lymphocyte ratio (MLR) have become popular research topics, only a few studies have been conducted on the use of NLR and PLR for the diagnosis of TT[2,7-9]. Likewise, to the best of our knowledge, rare studies have been conducted on the use of MLR for the diagnosis of TT.
In the present study, we aimed to show the efficiency of NLR, PLR,and MLR for the diagnosis of TT and to determine whether these values can help distinguish between TT and epididymo-orchitis.
2. Materials and methods
2.1. Ethical consideration
Ethics committee approval and institutional approval (Protocol code: 2019/109-Decision number: 2019-04-11) were received from the Clinical Research Ethics Committee of Antalya Training and Research Hospital.
2.2. Participants
Our study was designed as a retrospective cohort study. Patients were included in the study once they met the following criteria:(1) ≥12 years; (2) Visited the emergency department (ED) due to acute scrotal pain between January 1, 2016, and January 1,2018; (3) Diagnosed as epididymo-orchitis or TT; (4) Supported by physical examination, imaging, and laboratory tests. The exclusion criteria included: (1) Patients with testicular trauma (n=3);(2) Previous testicular surgery (n=2); (3) Chronic liver disease(n=2); (4) Previous testicular exploration with normal results(n=2); (5) Those with missing data (n=1). A total of 10 patients were excluded from the study. Consequently, 190 patients were selected for this study. Meanwhile, another 100 patients were randomly assigned to the healthy control group (Figure 1).
Patients were screened using the electronic database of the hospital retrospectively. All patients underwent scrotal USG in the ED by a radiologist. The patients were examined by a urologist or pediatric surgeon, and those who were diagnosed as TT with surgery. The patients were categorized into 3 groups: the TT group with surgery(n=70); the epididymo-orchitis group with epididymo-orchitis treatment (n=120); and the healthy control group (n=100).
2.3. Complete blood count parameters
Complete blood count (CBC) including NLR, PLR, and MLR,white blood cell (WBC), and neutrophil values was performed and recorded in all patients when they first visited the ED. For blood analysis, 3 mL of venous blood samples were collected in Tripotassium K3 ethylenediaminetetraacetate vacuum tubes. Blood samples were analyzed within 1 h from the patient’s admission using an automated blood cell counter (Coulter®LH 780 Hematologic Analyzer, Beckman Coulter Inc. Brea, USA). Normal values were accepted as (150-450)×103mm3for platelets, (4-10.5)×103mm3for WBC, (1.82-7.42)×103mm3for neutrophils and (0.85-3)×103mm3for lymphocytes.

Figure 1. The study flowchart.
2.4. Statistical analysis
Data were analyzed using SPSS 18.0. Continuous variables were described as standard deviation ± mean values and non-parametric data as median and interquartile interval. TheChi-square test was used to compare proportions in different groups. Analysis of variance(ANOVA) tests or Mann-WhitneyU-test was used to compare the two independent groups according to distribution. The optimum cutoff values of NLR, MLR, and PLR were analyzed by ROC analysis.
3. Results
The mean age of the patients in TT and epididymo-orchitis groups was (23.5±13.4) years and (34.7±22.4) years, respectively. Patients with TT were significantly younger than those with epididymoorchitis (P=0.022). Of the patients with TT, 70% underwent detorsion and 30% underwent orchiectomy. Table 1 shows the comparison of parameters among the three groups.
Mean WBC and neutrophil values were significantly higher in the epididymo-orchitis group compared to the TT and the control groups (P=0.001). The mean PLR in the control group was lower than that of both the TT and the epididymo-orchitis group (P<0.001). Finally, the mean NLR and MLR values were significantly higher in the epididymo-orchitis group compared to the TT and the control group (P<0.001 andP<0.001, respectively).
ROC analysis showed that the sensitivities of WBC, neutrophil,NLR, and PLR were 65.7%, 74.3%, 77.1%, and 68.2%,respectively and specificities were 73%, 68%, 80%, and 78%,respectively. The optimal cut-off value of MLR had a sensitivity of 67.1% and a specificity of 75%. Result of the ROC analysis are shown in Table 2 and Figure 2.
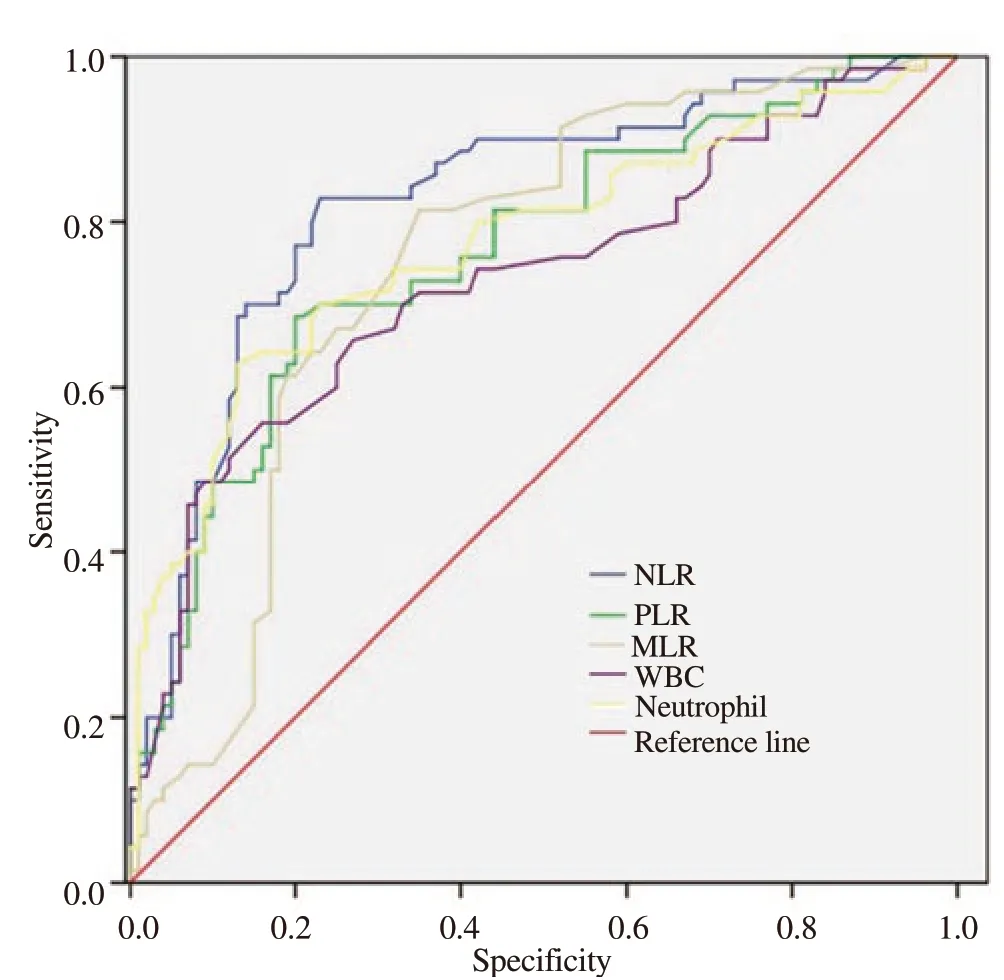
Figure 2. Receiver operating characteristic of parameters in the torsion group. NLR: Neutrophil-lymphocyte ratio; PLR: Platelet-lymphocyte ratio;MLR: Monocyte lymphocyte ratio; WBC: white blood cell.

Table 1. Comparison of parameters of the three groups.
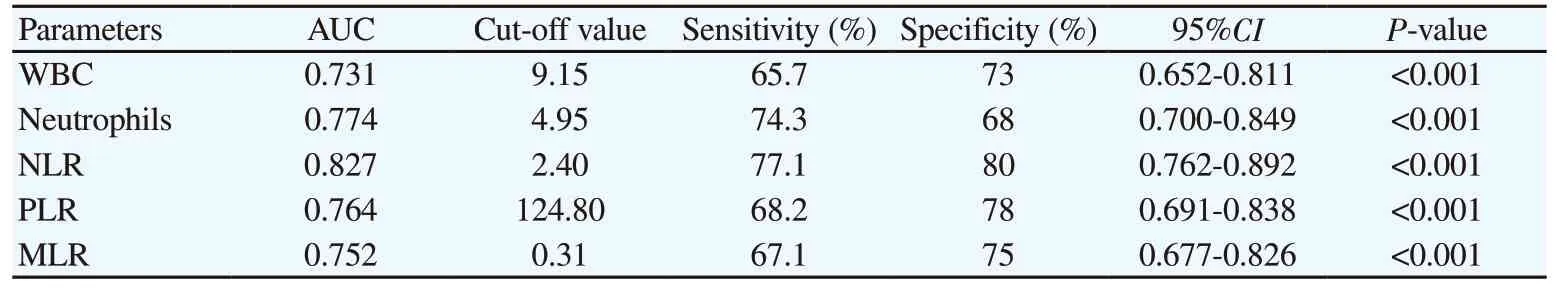
Table 2. Diagnostic accuracy of parameters for predicting the presence of testicular torsion.
4. Discussion
Acute scrotum disease is the most common urological emergency in the ED. This situation requires urgent diagnosis and treatment since testicular loss might be inevitable due to the delayed intervention[10,11]. Currently, the diagnosis method of the acute scrotum disease are not specific. Blood routine test are usually carried out[12,13]. Previous studies have reported that the erythrocyte sedimentation rate and acute phase reactants such as C-reactive protein would increase in TT patients[12]. In this study,we evaluated the predictive roles of WBC, neutrophil, NLR, PLR,and MLR in the diagnosis of TT. These parameters are of utmost importance because they are quick to perform and easy to access.
WBC count is routinely used to determine inflammation in clinical practice. Studies have shown an increase in WBC count in patients with TT[2,10]. Also, other studies have shown that hematological parameters such as NLR and PLR can be used in the diagnosis of acute and chronic inflammation[14,15]. They are used as practical inflammatory markers in the diagnosis and prognosis of many diseases especially during perioperative cancer surgery[16-22]. A recent study reported that the PLR and NLR values of patients with TT were significantly higher compared to the control group[9]. A study conducted in 2017 reported that NLR values in patients with TT were significantly higher compared to the control group, but PLR values in patients with torsion did not differ from those in the control group[2]. Previous studies have shown that D-dimer levels would start to increase a few minutes after the onset of ischemia,and D-dimer was found to be higher in patients with TT than acute epididymitis, and it was reported to be a diagnostic marker[23]. In our study, mean WBC, NLR, and PLR were significantly higher in the TT group compared with the control group (P<0.005).Also, NLR levels were higher in patients with epididymo-orchitis compared to patients with torsion. According to our findings, WBC count and NLR were useful parameters in the differential diagnosis of epididymo-orchitis and TT. However, PLR values were higher in patients with epididymo-orchitis compared to patients with torsion,but this difference was not statistically significant.
As is known, the role of monocytes in the immune system is cytokine expression, antigen presentation, or phagocytosis. It has recently been reported that abnormally activated monocytes can play a role in the pathogenesis of inflammation[24]. Like monocytes, the function of MLR has also been studied as an immunological marker and as an indicator of inflammation in many diseases[25]. Although previous studies have investigated the use of MLR in the diagnosis and prognosis of cancer patients and the diagnosis and treatment of diabetic retinopathy, Guillain Barre syndrome, and coronary artery disease, to the best of our knowledge, rare studies have studied the role of MLR in patients with TT[25-28]. In our study, mean MLR values were significantly higher in TT patients compared to the control group (P<0.005).The cut-off value of 0.31 for MLR had a sensitivity of 67.1% and specificity 75% when used for torsion. According to our findings,MLR is a simple and easily accessible parameter that can be used in the diagnosis of TT.
The present study had some limitations. Firstly, our study was performed retrospectively in a single center and included a relatively small number of patients. Secondly, physical examination, surgical treatment, and USG that was required for the diagnosis were performed by different physicians and radiologists.Thirdly, since the baseline NLR, PLR, and MLR values before the diagnosis of TT were not available in most patients, it was impossible to compare the baseline and subsequent parameters. The failure to compare these parameters with acute phase reactants such as C-reactive protein and sedimentation rate was also a significant limitation. Another important limitation is that the age distribution between the patient groups is not homogeneous and may have an effect on the results. In addition, USG can be used to check the testicular viability after TT treatment, but the retrospective nature of the present study did not permit this procedure.
Conflict of interest statement
The authors report no conflict of interest.
Authors’ contributions
C.B. and M.K.: Corresponding author, study designer, and writing the manuscript; C.B. and M.K.: Data collector, interpreter, and writing the introduction; C.B. and M.K.: Data analysis, writing the results.
 Journal of Acute Disease2020年5期
Journal of Acute Disease2020年5期
- Journal of Acute Disease的其它文章
- Using point-of-care ultrasound in ocular emergencies: A mini review
- Coronavirus disease 2019 (COVID-19), MERS and SARS: Similarity and difference
- An epidemiological report on the burden and trend of injuries in the Philippines from 2011 to 2018
- Epidemiological profile and management of acute pyelonephritis in the emergency department of a tertiary hospital: A retrospective observational study
- Effect of proximal femur nail anti-rotation on unstable intertrochanteric fractures: A prospective observational study
- Antibacterial activity of plant extracts in different solvents against pathogenic bacteria: An in vitro experiment
