Plasma big endothelin-1 is an effective predictor for ventricular arrythmias and end-stage events in primary prevention implantable cardioverterdefibrillator indication patients
Xiao-Yao LI, Shuang ZHAO, Xiao-Han FAN, Ke-Ping CHEN, Wei HUA, Zhi-Min LIU, Xiao-Di XUE,Bin ZHOU, Shu ZHANG
Arrhythmia Center, State Key Laboratory of Cardiovascular Disease, Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
Abstract Objective To investigate whether plasma big endothelin-1 (ET-1) predicts ventricular arrythmias (VAs) and end-stage events in primary prevention implantable cardioverter-defibrillator (ICD) indication patigents. Methods In total, 207 patients fulfilling the inclusion criteria from Fuwai Hospital between January 2013 and December 2015 were retrospectively analyzed. The cohort was divided into three groups according to baseline plasma big ET-1 tertiles: tertile 1 (< 0.38 pmol/L, n = 68), tertile 2 (0.38–0.7 pmol/L, n = 69), and tertile 3 (>0.7 pmol/L, n = 70). The primary endpoints were VAs. The secondary endpoints were end-stage events comprising all-cause mortality and heart transplantation. Results During a mean follow-up period of 25.6 ± 13.9 months, 38 (18.4%) VAs and 78 (37.7%) end-stage events occurred. Big ET-1 was positively correlated with NYHA class (r = 0.165, P = 0.018), serum creatinine concentration (Scr; r = 0.147, P =0.034), high-sensitivity C-reactive protein (hs-CRP; r = 0.217, P = 0.002), Lg NT-pro BNP (r = 0.463, P < 0.001), left ventricular end diastolic diameter (LVEDD; r = 0.234, P = 0.039) and negatively correlated with left ventricular ejection fraction (LVEF; r = −0.181, P =0.032). Kaplan-Meier analysis showed that elevated big ET-1 was associated with increased risk of VAs and end-stage events (P < 0.05). In multivariate Cox regression models, big ET-1 was an independent risk factor for VAs (hazard ratio (HR) = 3.477, 95% confidence interval(CI): 1.352–8.940, P = 0.010, tertile 2 vs. tertile 1; HR = 4.112, 95% CI: 1.604–10.540, P = 0.003, tertile 3 vs. tertile 1) and end-stage events(HR = 2.804, 95% CI: 1.354–5.806, P = 0.005, tertile 2 vs. tertile 1; HR = 4.652, 95% CI: 2.288–9.459, P < 0.001, tertile 3 vs. tertile 1).Conclusions In primary prevention ICD indication patients, plasma big ET-1 levels can predict VAs and end-stage events and may facilitate ICD-implantation risk stratification.
J Geriatr Cardiol 2020; 17: 427-433. doi:10.11909/j.issn.1671-5411.2020.07.003
Keywords: Big endothelin-1; End-stage events; Implantable cardioverter-defibrillator implantation; Primary prevention; Ventricular arrythmias
1 Introduction
Sudden cardiac death (SCD) is a serious public health problem worldwide, accounting for approximately 50% of all cardiovascular deaths.[1]An implantable cardioverter-defibrillator (ICD) can effectively terminate malignant tachyarrhythmia, prevent SCD and reduce all-cause mortality.[2–4]However, identification of primary prevention patients at high risk of SCD remains challenging.
According to current guidelines, left ventricular ejection fraction (LVEF) ≤ 35% is still recommended as the main criterion for implantation of an ICD for primary prevention of SCD.[1,5]However, recent studies have demonstrated that the application of LVEF alone lacks of both sensitivity and specificity for prediction of SCD.[6–8]Cardiac magnetic resonance imaging and electrical examination have also been explored for prediction of SCD,[9,10]but due to complexity of the operation, no factor has been widely used in clinical practice. The DANISH study revealed that the benefit of an ICD may be limited in patients with non-SCD risk and an evaluation in addition to LVEF might be needed before ICD implantation. In the era of optimal treatment of heart failure (HF) with drugs and devices, improving the efficiency and cost-effectiveness of ICD implantation for primary prevention of SCD is of great importance.[11]
The endothelial system is an important factor that regulates cardiovascular functions and contributes to neurohormonal activation, hemodynamic deterioration, and cardiovascular remodeling, and endothelin-1 (ET-1) has the strongest effect on this system. Big ET-1 is the precursor of ET-1 and has a longer half-life, which makes it a more suitable marker for the endothelial system. Previous studies have confirmed that big ET-1 is related to the pathophysiological progression of HF.[12,13]However, whether big ET-1 is related to SCD or ventricular arrythmias (VAs) is still unclear.The purpose of the present study was to investigate whether plasma big ET-1 could be a predictive factor for VAs and end-stage events in patients with indications for primary prevention ICD implantation.
2 Methods
2.1 Population selection
The present study retrospectively analysed the data of patients with symptomatic HF and left ventricular systolic dysfunction (LVEF ≤ 35%) at Fuwai Hospital (National Center of Cardiovascular Diseases, Beijing, China) between January 2013 and December 2015. Additional inclusion criteria were as follows: (1) age greater than 18 years; (2)available baseline big ET-1 results; and (3) indication for primary prevention ICD implantation. The exclusion criteria were as follows: (1) indication for the secondary prevention of SCD; (2) severe valvular disease was the main cause of HF; (3) a scheduled heart transplant within one year; and (4)participation in another clinical therapeutic trial that required the consent of the patient at the same time. In total, 218 patients qualified according to the inclusion criteria. However,eight candidates were excluded due to indications for the secondary prevention of SCD, and three patients were lost during follow-up. The ethics committee of the Fuwai Hospital approved the present study (No. 2012–427), and all patients signed informed consent forms before enrollment.
2.2 Data collection
The baseline data for all admitted patients in this study were obtained from their inpatient medical records during hospitalization. Demographic and clinical characteristics,including age, sex, body mass index (BMI), New York Heart Association (NYHA) class, etiology (ischemic cardiomyopathy or nonischemic cardiomyopathy), comorbidities (hypertension, diabetes, atrial fibrillation, and stroke),baseline laboratory data [routine blood examinations, biochemistry, and N-terminal pro brain natriuretic peptide(NT-pro BNP)], and medications (renin-angiotensin system blockers, β-blockers, spironolactone, loop diuretics, amiodarone, and digoxin) were reviewed and analyzed by two separate physicians who were blinded to the other results.Biochemistry assessments included alanine aminotransferase (ALT), high-sensitivity C-reactive protein (hs- CRP),and serum creatinine concentration (Scr). Echocardiography parameters, LVEF and left ventricular end-diastolic diameter (LVEDD) were evaluated by two physicians with experience in echocardiography. The LVEF was calculated using the modified Simpson’s biplane rule.
2.3 Big ET-1 and patient groups
Venous blood samples were collected from all patients after 12 h of fasting on the next morning of admission. All blood samples were tested in the medical examination center of Fuwai Hospital according to the standard procedure.The plasma big ET-1 level was measured with a highly sensitive and specific commercial sandwich enzyme immunoassay (BI-20082H, Biomedica, Wien, Austria). The normal range was less than 0.25 pmol/L, and the detection sensitivity was 0.02 pmol/L. Then, the patients were divided into three tertiles according to the baseline level of plasma big ET-1: tertile 1 (< 0.38 pmol/L,n= 68), tertile 2 (0.38–0.7 pmol/L,n= 69), and tertile 3 (> 0.7 pmol/L,n= 70).
2.4 Follow-up and endpoints
All patients were followed up regularly through outpatient or telephone calls at 3, 6, 12, 24 and 36 months. The primary endpoint events were VAs including SCD, appropriate ICD therapy and documented sustained ventricular tachycardia or nonfatal ventricular fibrillation. SCD was defined as sudden and unpredictable death following cardiovascular symptoms within 1 h. ICD appropriate therapy refers to appropriate anti-tachycardia pacing (ATP) and shock for sustained ventricular tachycardia.[14]The secondary endpoint events were a composite of end-stage events consisting of all-cause mortality and heart transplantation.
2.5 Statistical analysis
Continuous variables are presented as the mean ± SD,and nominal data are presented as numbers and percentages.Baseline characteristics were compared among the groups using one-way analysis of variance for continuous variables and chi-square tests for categorical variables. Kaplan-Meier curves were generated to compare the endpoints between groups. The Log-rank test was used to evaluate significant differences. Cox proportional hazard models were used to evaluate differences in endpoint events between groups. All variables with a statistically significant effect were introduced into a multivariate Cox proportional hazards model(forced-entry method). Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated to show the effects of variables. SPSS 23.0 (IBM Corp., Armonk, New York) and GraphPad Prism 7.0 (GraphPad Software, La Jolla, California) were used to perform all statistical analyses. AP-value< 0.05 was considered significant in all conditions.
3 Results
3.1 Baseline characteristics and groups
Data from 207 patients, composed of 111 patients with ischemic cardiomyopathy (53.6%) and 96 patients with nonischemic cardiomyopathy (46.4%), were ultimately analyzed.Males were predominant in the study population (79.7%),and the mean age was 56.38 ± 14.00 years old.
The baseline characteristics of patients are shown in Table 1. Participants in tertile 2 and tertile 3 had worse NYHA classes, lower LVEF, more manifestations of atrial fibrillation, and more use of amiodarone and digoxin. Patients with an elevated big ET-1 level also had higher levels of Scr,hs-CRP, Lg NT-pro BNP, and LVEDD. Moreover, the tertile 3 group had a lower rate of renin-angiotensin system blocker use.
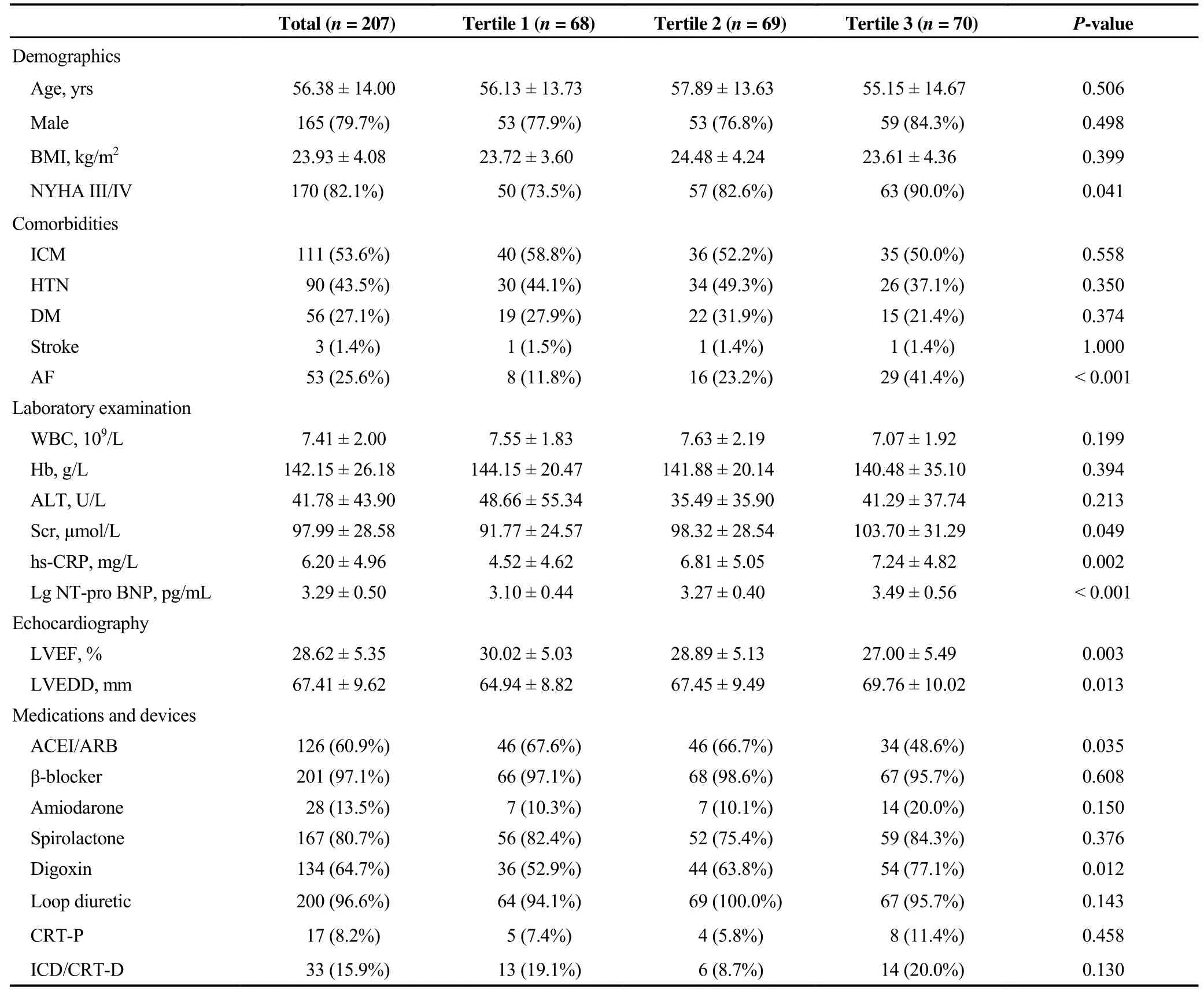
Table 1. Baseline characteristics according to big ET-1 tertiles.

Table 2. Correlation analysis between big ET-1 and baseline variables.
3.2 Relationship between big ET-1 and baseline variables
In the correlation analysis, big ET-1 was positively correlated with NYHA class (r= 0.165,P= 0.018), Scr (r=0.147,P= 0.034), hs-CRP (r= 0.217,P= 0.002), Lg NTpro BNP (r= 0.463,P< 0.001), and LVEDD (r= 0.234,P= 0.039) and negatively correlated with LVEF (r= −0.181,P= 0.032) (Table 2).
3.3 Clinical outcomes and Kaplan-Meier survival analysis
The average follow-up period was 25.6 ± 13.9 months,VAs occurred in 38 primary prevention patients (18.4%), of whom 30 suffered SCD, six received an appropriate ICD therapy and two survived documented sustained ventricular tachycardia or nonfatal ventricular fibrillation. Patients in tertile 2 and tertile 3 had higher rates of VAs than those in tertile 1 (8.8%vs.23.2%vs.22.9%, tertile 1–3,P= 0.026).
Seventy-eight (37.7%) end-stage events occurred including seven heart transplantations. The risk of end-stage events increased according to big ET-1 level (14.7%vs.40.6%vs.57.1%, tertiles 1–3,P< 0.001). As shown in Figure 1, in the Kaplan-Meier survival analysis, big ET-1 was associated with increased risk of VAs and end-stage events (P<0.05).
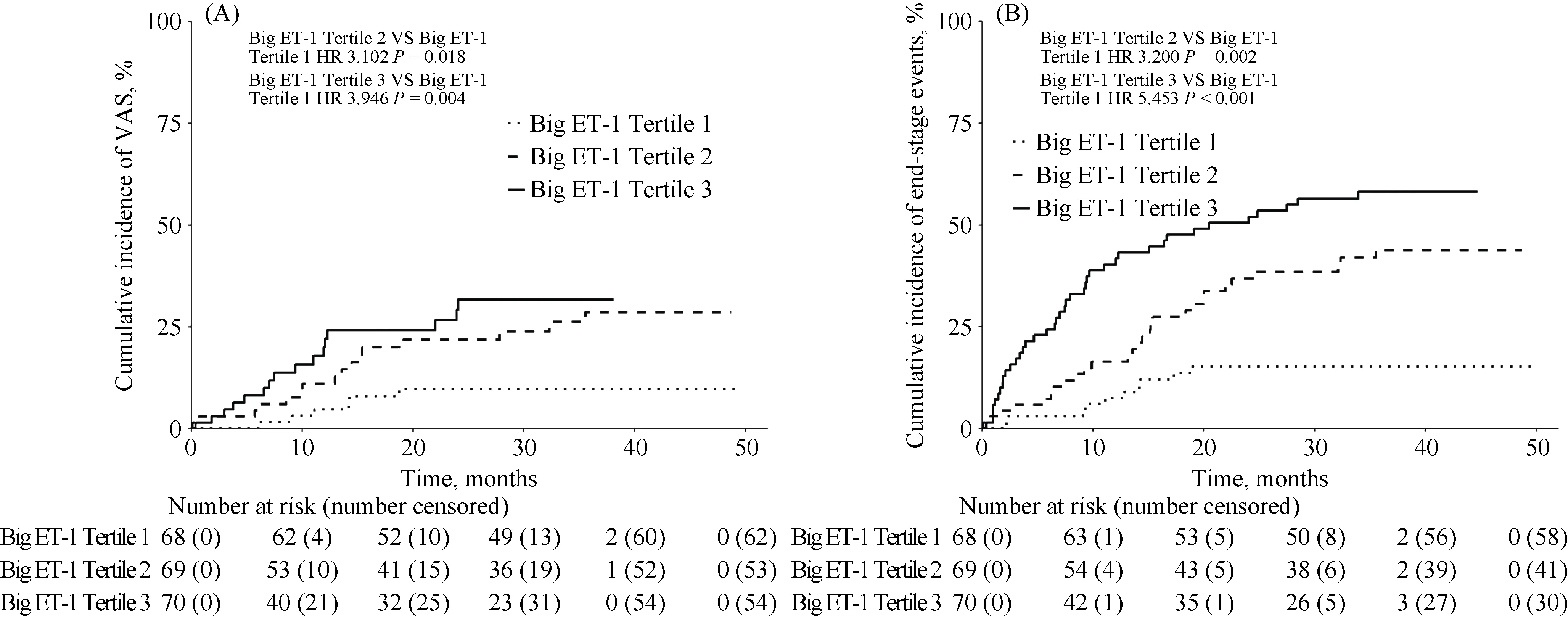
Figure 1 Kaplan-Meier estimates of the cumulative incidence of VAs (A) and end-stage events (B) in the three groups. VAs: ventricular arrhythmias
3.4 Plasma big ET-1 as a predictor for VAs and endstage events
In the univariate Cox regression models, in tertile 2 and tertile 3, big ET-1 along with ICD implantation, Scr, spironolactone and amiodarone were significantly related to VAs(P< 0.05). The multivariate Cox regression modeling results showed that a high plasma big ET-1 level was an independent risk factor for VAs (HR = 3.477, 95% CI:1.352–8.940,P= 0.010, tertile 2vs.tertile 1; HR = 4.112,95% CI: 1.604–10.540,P= 0.003, tertile 3vs.tertile 1) (Table 3).
Additionally, in tertile 2 and tertile 3, big ET-1 as well as BMI, atrial fibrillation (AF), ALT, Lg NT-pro BNP, LVEF,LVEDD and angiotensin-converting enzyme inhibitor (ACEI)/angiotensin receptor blocker (ARB) use were positively associated with end-stage events (P< 0.05). Multivariate Cox regression modeling results showed that a high plasma big ET-1 level was an independent risk factor for end-stage events (HR = 2.804, 95% CI: 1.354–5.806,P= 0.005, tertile 2vs.tertile 1; HR = 4.652, 95% CI: 2.288–9.459,P< 0.001,tertile 3vs.tertile 1) (Table 4).

Table 3. Predictors of VAs risk, uni- and multivariate Cox proportional hazards models.

Table 4. Predictors of end-stage events risk, uni- and multi-variate Cox proportional hazards models.
4 Discussion
The results of the present study demonstrated that plasma big ET-1, as a simple and practicable blood marker, is significantly and independently related to SCD risk in the primary prevention ICD indication population and thus may aid in selecting appropriate patients, especially for primary prevention ICD implantation.
Plasma big ET-1 has been studied as a predictor and prognostic marker in coronary artery disease, myocardial infarction, and HF.[15,16]Moreover, big ET-1 can predict the responsiveness and prognosis of patients undergoing cardiac resynchronization therapy.[17]However, the relationship between big ET-1 and VAs has been less investigated. Shah,et al.[18]found that the level of big ET-1 was significantly increased during ventricular fibrillation in pigs with acute myocardial infarction. Szûcs and colleagues demonstrated that the big ET-1 level was significantly increased in eleven patients with persistent ventricular tachycardia or ventricular fibrillation.[19]However, the above studies did not explore the predictive value of big ET-1 for VAs in patients at a high risk for SCD in clinical settings. The patients included in our study were at high risk for SCD, with decreased LVEF and indications for primary prevention ICD implantation.
In our study, the risk of VAs in patients with primary prevention ICD indications was compared according to tertiles of the baseline level of plasma big ET-1. The results showed that the risk of SCD was increased in patients with high plasma big ET-1 levels. Compared to tertile 2, the risk for patients in tertile 3 was higher, but it did not reach statistical significance, which may be related to the high mortality rate of tertile 3 and the small number of patients included in this study. Furthermore, the predictive value of plasma big ET-1 for the combined endpoint of heart transplantation and all-cause mortality was also excellent. A higher level of plasma big ET-1 resulted in a higher risk of end-stage events.
Big ET-1 is mainly secreted by the vascular endothelium.It exerts its bioactivity, including vasoconstriction, myocardial fibrosis and inflammation, in the development of cardiovascular diseases via two G protein-coupled receptors.[20]The effective prognostic value of big ET-1 in predicting VAs seems to be explained by its potential physiological mechanism. First, an increase in big ET-1 can activate the sympathetic nervous system and renin-angiotensin aldosterone system, promote the proliferation of cardiomyocytes and increase the extracellular matrix, which may lead to the formation of the pathological substrate of arrhythmia.[21]In addition, big ET-1 can act with ion channels. Liu,et al.[22]found that an exogenous increase in big ET-1 levels accelerated the depolarization of cardiomyocytes, prolonged the duration of the action potential, and thus increased heart rate variability (HRV). Moreover, big ET-1 can promote ventricular remodeling. Liu,et al.[23]found that myocardial fibrosis and ventricular remodeling were mediated by the TGF-β1-endothelin-1 signaling pathway in patients with HF.
4.1 Limitations
The sample size of the study was rather small. Additionally, the changes in plasma big ET-1 levels were not monitored dynamically during the follow-up period. Therefore,further large, prospective randomized controlled trials are needed to confirm the accuracy of the conclusions.
4.2 Conclusions
In primary prevention ICD indication patients, plasma big ET-1 levels are predictive of VAs and end-stage events and thus may aid in ICD implantation risk stratification.
Acknowledgments
This study was supported by Natural Science Foundation of China (81470466). All authors had no conflicts of interest to disclose.
 Journal of Geriatric Cardiology2020年7期
Journal of Geriatric Cardiology2020年7期
- Journal of Geriatric Cardiology的其它文章
- Measuring frailty in patients with severe aortic stenosis: a comparison of the edmonton frail scale with modified fried frailty assessment in patients undergoing transcatheter aortic valve replacement
- Atherosclerosis, its risk factors, and cognitive impairment in older adults
- Remote monitoring of implantable cardioverters defibrillators: a comparison of acceptance between octogenarians and younger patients
- Quality of life, physical performance and nutritional status in older patients hospitalized in a cardiology department
- Left atrial diameter and atrial fibrillation, but not elevated NT-proBNP,predict the development of pulmonary hypertension in patients with HFpEF
- Modified subintimal plaque modification improving future recanalization of chronic total occlusion percutaneous coronary intervention
