Remote monitoring of implantable cardioverters defibrillators: a comparison of acceptance between octogenarians and younger patients
Iva Safarikova, Alan Bulava, Premysl Hajek
1Faculty of Health and Social Sciences,the University of South Bohemiain Ceske Budejovice,Ceske Budejovice, Czech Republic
2Cardiac Center,Department of Cardiology, Ceske Budejovice Hospital,Ceske Budejovice,Czech Republic
3Faculty of Medicine and Dentistry of Palacky University Olomouc, Olomouc, Czech Republic
Abstract Background Remote monitoring (RM) is increasingly employed for all types of cardiac implantable devices (CIED). However, there are only limited data on the acceptance of RM by the elderly. The aim of our study was to ascertain how octogenarians assess RM technologies compared to younger, presumably technically more literate patients, and what concerns or technical problems the system presents to both groups of patients. Methods The trial was designed as a descriptive, register-based single-center study. The study population consisted of all consecutive patients ≥ 80 years of age (group A, n = 94) and all consecutive patients aged ≤ 40 years (group B, n = 71), who had undergone implantation of an implantable cardioverter-defibrillator (ICD) between the years of 2009 and 2018 and were using a Home Monitoring™ (HM, Biotronik, Berlin, Germany) system. All patients fulfilling entry criteria were approached with a request to participate in the survey. Results A total of 85 (90.4%) and 65 (91.5%) valid surveys were obtained for groups A and B, respectively. Ninety-two percent of patients in both groups (P = 0.903) were satisfied with the limited number of planned ambulatory follow-ups (i.e., once a year). All patients in both groups (100%) reported that they were satisfied with the HM system, and 97% and 94% of patients in Groups A and B, respectively, ranked it highly beneficial (P = 0.68). A significant proportion of patients in both groups were completely unaware of any health-related benefits associated with the use of the HM system (42% in Group A vs. 49% in Group B, P = 0.4). Among the most frequently reported personal benefits of HM were a sense of safety and security and savings on travel expenses and time. 5% and 9% of patients in Groups A and B, respectively, reported that usage of HM caused them some degree of psychological stress (P = 0.27). Nearly all patients in both groups reported receiving information on HM from their doctor after ICD implantation. None of Group A reported receiving information from a nurse either before or after ICD implantation, while 14% of Group B patients reported receiving information from a nurse after,but not before ICD implantation. Seven and 51% (P < 0.0001) of patients in Group A and B, respectively, sought additional information about HM post-discharge. Conclusions The HM system received good marks and was much appreciated, even in patients over 80 years of age. The level of acceptance and potential psychological stress resulting from RM technology appears to be about the same in older patients as in younger patients. The majority of octogenarians either did not fully understand the clinical benefits of the system or mistakenly thought that the HM system was a substitute for emergency 24-h surveillance. These results highlight the need for better patient education relative to RM technology, with one option being to delegate more of this educational process to specially trained nurses.
J Geriatr Cardiol 2020; 17: 417-426. doi:10.11909/j.issn.1671-5411.2020.07.008
Keywords: Education; Implantable electronic devices; Remote monitoring; The elderly
1 Introduction
The clinical benefit of cardiac implantable electronic devices (CIED) is well documented and is, therefore, the main reason for their use in patients of all ages.[1]Because the indication criteria for CIED implantation are getting broader,the number of patients with cardiac implants continues to rise, and since the average life expectancy is simultaneously increasing, the number of patients over 80 years of age, for whom such a procedure is often indicated, is also steadily increasing.[2]
It is recommended that all patients wearing CIEDs undergo regular check-ups of system functionality as well as an assessment of their clinical condition.[3,4]Although modern technologies for remote monitoring (RM) are now widely available, they are underused, especially by patients who might truly benefit, such as the elderly or people with physical disabilities.[5]RM is underused, especially in octogenarians, due to general skepticism regarding the ability of the elderly to effectively use modern technologies. This is made worse by the fact that there is limited data on the acceptance and operational skills required for RM technologies in the elderly population.
The aim of our study was to ascertain how patients ≥ 80 years of age, compared with younger, potentially more technically literate patients ≤ 40 years of age, with implantable cardioverter-defibrillators (ICD), are using one of the commercially available RM systems [i.e., Home Monitoring®(HM), Berlin, Germany]. Additionally, we wanted to know what concerns or perhaps technical problems the system presents for both groups so as to properly identify the specific problems that need to be addressed through educational intervention. The second major goal was to determine what and/or who was the main source of information regarding the use of the HM system at our institution.
2 Methods
2.1 Setting
The study was performed in one of the largest cardiac centers utilizing RM in the Czech Republic. At present,there are more than 3000 patients being followed remotely in our database. Regarding CIEDs, as a part of standard care at our institution, all mentally competent patients receive an HM system and are offered an opportunity to continue with remote follow-up of their ICD using this technology with only one in-office visit per year, unless there is a specific need for an earlier check-up.
2.2 Study design and participants
The study population consisted of 94 patients ≥ 80 years of age (group A) and 71 patients ≤ 40 years of age (group B), who were identified from our Home Monitoring Database and who had undergone implantation of an ICD within the last ten years. All patients were monitored using the Home Monitoring®system (HM) starting immediately after device implantation, and regular follow-ups were conducted once a year unless extra visits were initiated either by the patient or by the physician based on remotely retrieved data indicating the need for medical intervention. All patients in the study were required to have at least one year of experience with the HM system before being enrolled.
Study patients were recruited by phone and asked to complete a phone questionnaire. Informed consent was given orally at the time of the interview, and data processing was done anonymously. Both the survey structure, as well as the individual questions, were designed to match the aim of the study and increase reliability. This approach was dictated by the lack of validated questionnaires that specifically address the quality of life and acceptance of RM technologies in the literature. Patients who agreed to take the survey were interviewed using prepared questions, with possible answers read to them during the initial oral interview, or with regard to open-ended questions, their responses were transcribed verbatim. The average interview lasted 17.8 ±7.2 (12–28) and 15.1 ± 5.1 (11–22) min in groups A and B,respectively. A total of 85 (90.4%) and 65 (91.5%) valid surveys were obtained in groups A and B, respectively. The rest of the patients either did not give informed consent to enter the study, or their mental or physical state had deteriorated to such an extent that they were unable to complete the interview.
2.3 Study goals
Our primary goal was to ascertain how octogenarians with an ICD perceive remote follow-up of their device compared with younger, potentially more technically literate patients ≤ 40 years of age. Specifically, we looked at the acceptance of HM, benefits, concerns, and problems related to the use of the system and especially the perceived personal benefits. The second goal was to determine what and/or who was the main source of information on the HM system and try to identify specific problem areas regarding RM technologies, in the younger population and in octogenarians with an ICD that could be addressed through improved education.
2.4 Statistical analysis
Standard descriptive statistics were used to describe the clinical characteristics and outcomes of the individual surveys within the two patient groups. Categorical parameters were expressed using absolute and relative frequencies;continuous parameters were presented using the mean ± SD and/or the median. The nonparametric Mann-WhitneyUtest was used to assess the statistical significance of the differences of continuous parameters between the two patient groups. Categorical parameters were assessed using Fisher’s exact test. AP-value of < 0.05 was considered statistically significant. Calculations were performed using the SPSS Statistics program for Windows, version 24.0.0.0 (IBM Corp., Armonk, N.Y., USA).
3 Results
3.1 Baseline characteristics
The basic descriptive characteristics of the cohort are given in Table 1. Group A (octogenarians) had a substantially higher occurrence of arterial hypertension, diabetes,hyperlipoproteinemia, atrial fibrillation, and ischemic heart disease. The prevalence of dilated cardiomyopathy was comparable; men were more prevalent in Group B (patients≤ 40 years of age). These patients also preferred the mobile version of the CardioMessenger.
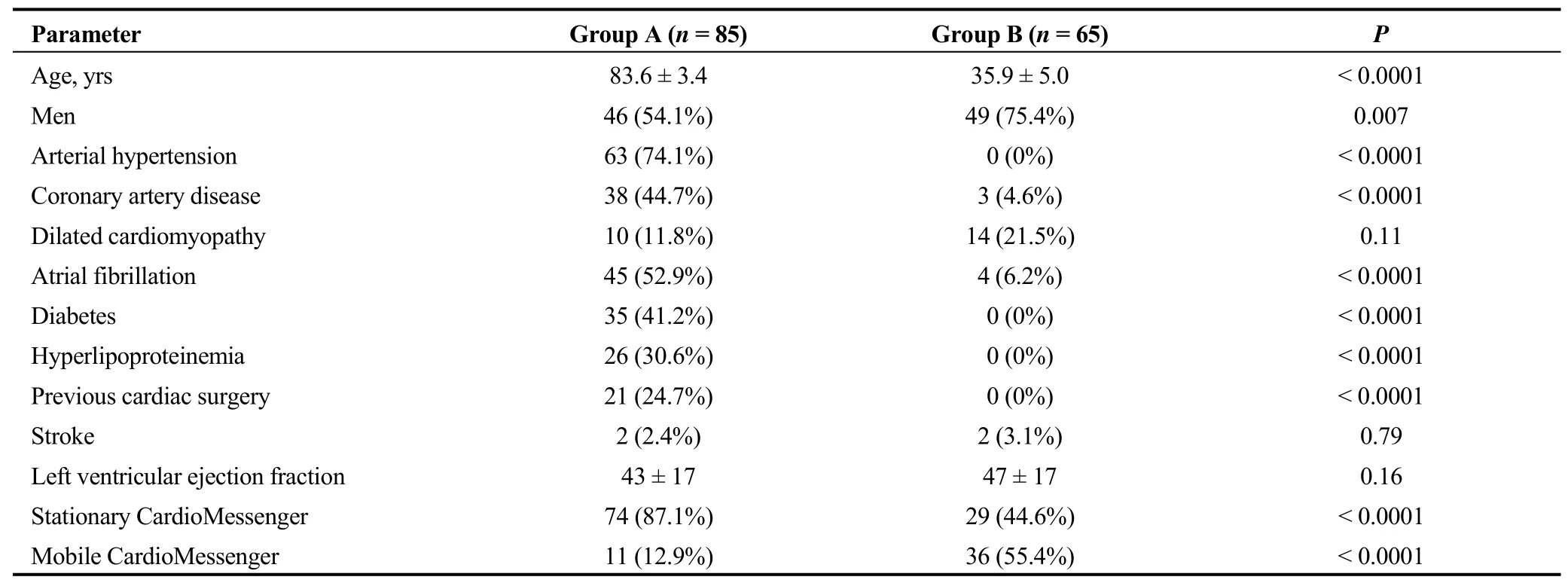
Table 1. A comparison of the basic clinical data from patients ≥ 80 years of age (Group A) vs. patients ≤ 40 years of age (Group B)with an implantable cardioverter-defibrillator, who were followed using a Home Monitoring® system (HM, Biotronik, Germany)and agreed to participate in the study and completed the interview.
3.2 Types of ICDs
Patient groups also differed in terms of the implanted device (Figure 1). Biventricular devices (CRT-Ds) were by far the most common in the younger group B (P< 0.001). Single-chamber ICDs were the least common implanted devices in both groups.

Figure 1. The structure of implanted devices in octogenarians (Group A) and patients of ≤ 40 years of age (Group B). CRT-D:biventricular devices; 1D ICD: single-chamber devices; 2D ICD: dual-chamber devices.
3.3 Acceptance and rating of the HM system
A similar (P= 0.903) majority of patients in both Group A (92%) and Group B (92%) were satisfied with the small number of planned ambulatory follow-ups (i.e., once a year).Although most patients found the number of ambulatory follow-ups extremely convenient, 11% of patients in Group A and 12% (P= 0.81) of patients in Group B said they would welcome more frequent visits to the arrhythmology ambulatory unit. The rest would prefer either the current or even longer intervals between ambulatory visits.
Satisfaction with the HM system was 100% in both groups (P= 1.0). All these patients were delighted with the HM system, and looking back, they reported that they were glad this modern technology had been offered to them.
The patients were instructed to rank the HM system on a scale of 1 to 5 (1 = highly beneficial, 2 = beneficial, 3 =somewhat beneficial, 4 = almost unbeneficial, 5 = completely unbeneficial). Patients in Group A found HM highly beneficial (mark 1) and beneficial (mark 2) in 97% and 3%of cases, respectively. Patients in Group B showed similar results (P= 0.68): 94% and 6% of patients considered theHM system highly beneficial or beneficial, respectively.None of the patients in either group ranked the HM technology less than 2.
From their personal perspective, the HM system generally gave patients a feeling of safety and security (Figure 2).During the interview, many patients noted that the green ON indicator light (or the “OK” text on the mobile unit)represented positive feedback for them, and they regularly checked to see whether it was still green (or “OK”). Group B patients also appreciated the time and money saved on travel and the time saved not waiting at the clinic (48% of patients in Group Bvs. 33% in Group A). Both groups similarly reported that HM provided a sense of calm, comfort, and well-being (15% of all patients), nonetheless, a significant number of patients (21% in Group A and 20% in Group B) could not describe any personal benefits provided by the HM system.
3.4 Clinical benefits, concerns, and technical problems related to the use of the HM system
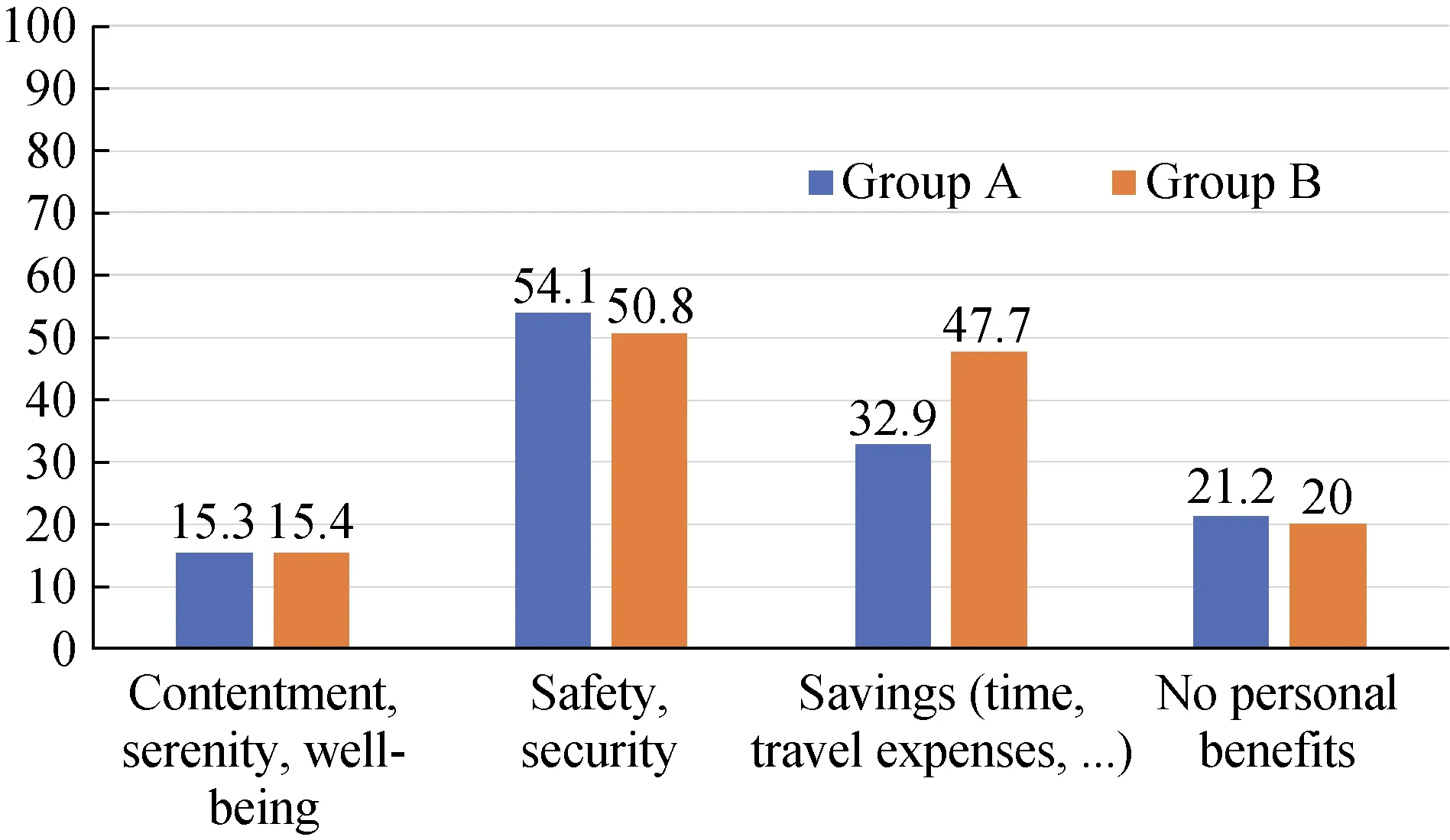
Figure 2. Patient views on the personal benefits of the HM system. Numbers are percentages of patients in the respective group. Group A: octogenarians, Group B: patients ≤ 40 years of age. HM: home monitoring.
Alarmingly, a significant proportion of patients in both groups was completely unaware of any health-related benefits associated with the use of the HM system (42% in Group Avs. 49% in Group B,P= 0.402, Figure 3). On the other hand, more patients in Group A compared to Group B(55%vs. 14%,P< 0.0001) thought that HM was designed to serve as an emergency system that monitored their clinical condition 24 hours a day, 365 days a year, with the potential for an immediate response by medical personnel(emergency 24-hour surveillance). Only two patients (representing 2%) out of the whole cohort of octogenarians correctly answered that the HM system serves to prevent their clinical condition from suddenly worsening. Generally, patients in Group B were more likely to state at least one true clinical benefit of HM technology as it related directly to their health status (P< 0.01): i.e., a prompt response to deteriorating clinical conditions or technical failure of the device (23% of patients), prevention of sudden worsening of clinical conditions (20% of patients), decreased psychological burden (3% of patients), or the ability to archive all significantly relevant events (5% of patients).
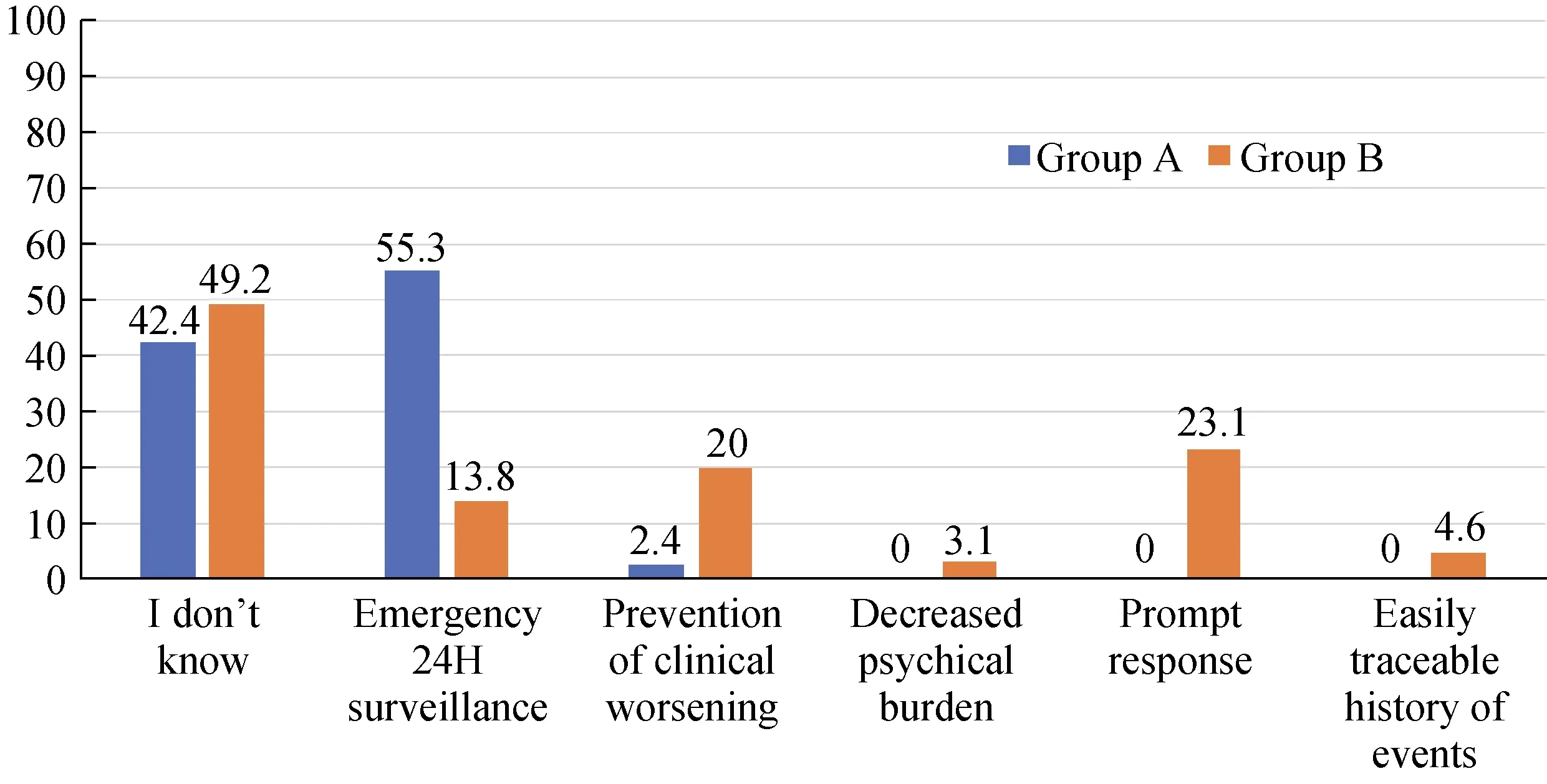
Figure 3. Patient views on the benefits of HM, in terms of its effect on health. Numbers are percentages of patients in the respective group. Group A: octogenarians; Group B: patients ≤ 40 years of age. HM: home monitoring.
The vast majority of the patients were not afraid of and had no concerns about using the HM system for the very first time, with no significant difference between patients in Group A and B (95%vs. 97%,P= 0.614).
Technical problems related to the CardioMessenger unit occurred in only 5% and 8% of patients in groups A and B,respectively (P= 0.445). However, none of the problems were clinically dangerous, let alone life-threatening. The interviews revealed that most of the problems in Group A were user-related, e.g., forgot to plug the unit into a power source, forgot to take the patient unit with them when traveling (which prevented data transfer and prevented the doctor from having access to their data), etc. One patient in Group A and two patients in Group B also reported that they had a hard time finding a suitable location in their home with a strong enough GSM signal for the patient unit. One patient reported that during a summer storm, lightning damaged his CardioMessenger, which had to be subsequently replaced. There were unexpected technical problems with the CardioMessenger in a total of four patients(3%), which mandated the replacement of the unit (one in Group A and three in Group B); after the units were replaced, the HM system operated uneventfully.
3.5 Psychological problems
Five percent of patients in Group A and 9% of patients in Group B reported that the HM system caused them some degree of psychological stress (P= 0.27). The most common concerns in Group A were loss of connection, fear of forgetting to bring the mobile CardioMessenger when out of the house, and loss of power to the unit. Three of the octogenarians (4%) also reported that they did not fully trust HM (e.g., they expressed concerns about the reliability of data transfer), in part because they did not completely understand its function. Additionally, they also reported that they were never sure whether remote monitoring was properly working because they had no meaningful feedback aside from the green indicator light on the HM unit.
On the other hand, the most common concerns of Group B patients were the appearance of an unknown number on his/her mobile phone, anxiety regarding “being tracked,”and fear related to security checks at airports, and as with Group A patients, they expressed concerns about forgetting to carry the mobile CardioMessenger with them when they left their home and loss of power to the unit.
3.6 Patient education and sources of patient information
Ninety-five percent and 97% of patients in Group A and B, respectively (P= 0.87), reported that they received information or education on HM technology before the implantation procedure from the materials that contained the written informed consent (Figure 4). Only 25% and 22% of patients in Group A and B, respectively (P= 0.84), were specifically educated or informed about the availability of HM technology by their doctor. None of the patients in either group sought supplemental information on ICD implantation and/or RM technologies from family, friends,books, newspapers, or the Internet. A minority of patients(3%–5%) in both groups reported that they had not received any information at all; however, all patients signed the written informed consent at the time of implantation, which contained information on RM.
Almost all patients in both groups received information on HM technology after the implantation procedure and prior to discharge from the hospital, with the vast majority of this information coming from the attending doctors. In the octogenarian group, nurses were not involved in postimplantation HM education, while Group B patients reported that nurses were involved about 14% of the time (Figure 5).
Only 7% and 51% (P< 0.0001) of patients in Group A and B, respectively, sought additional information about HM post-discharge (Figure 6). A minority of patients in Group A searched for information on the Internet (3%), from the referring cardiologists (2%), or their family members (1%).The majority of patients in Group B cited the Internet as their main source of additional information about the HM system (48%), while HM information obtained from the referring cardiologist (6%), friends (3%), and family(2%) was more than Group A patients, it was still relatively insignificant. Six percent of Group B patients searched for specific information about HM in magazines or books.
The main reason octogenarians gave for seeking more information post-discharge was that they felt the in-hospital education was too brief and lacked sufficient information(both 5%). Only one patient (1%) reported that the in-hospital information was unintelligible. The unintelligibility of information, the lack of sufficient information, and the brief time during in-hospital education were reported by 6%, 23%,and 34% of patients in Group B, respectively.
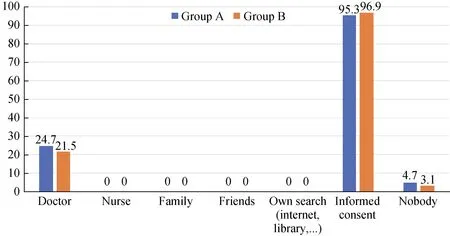
Figure 4. Sources of patient information before device implantation (several options were available for selection during the interview, e.g., doctors, nurses, family, etc). Numbers are percentages of patients in the respective group. Group A: octogenarians, Group B:patients ≤ 40 years of age.
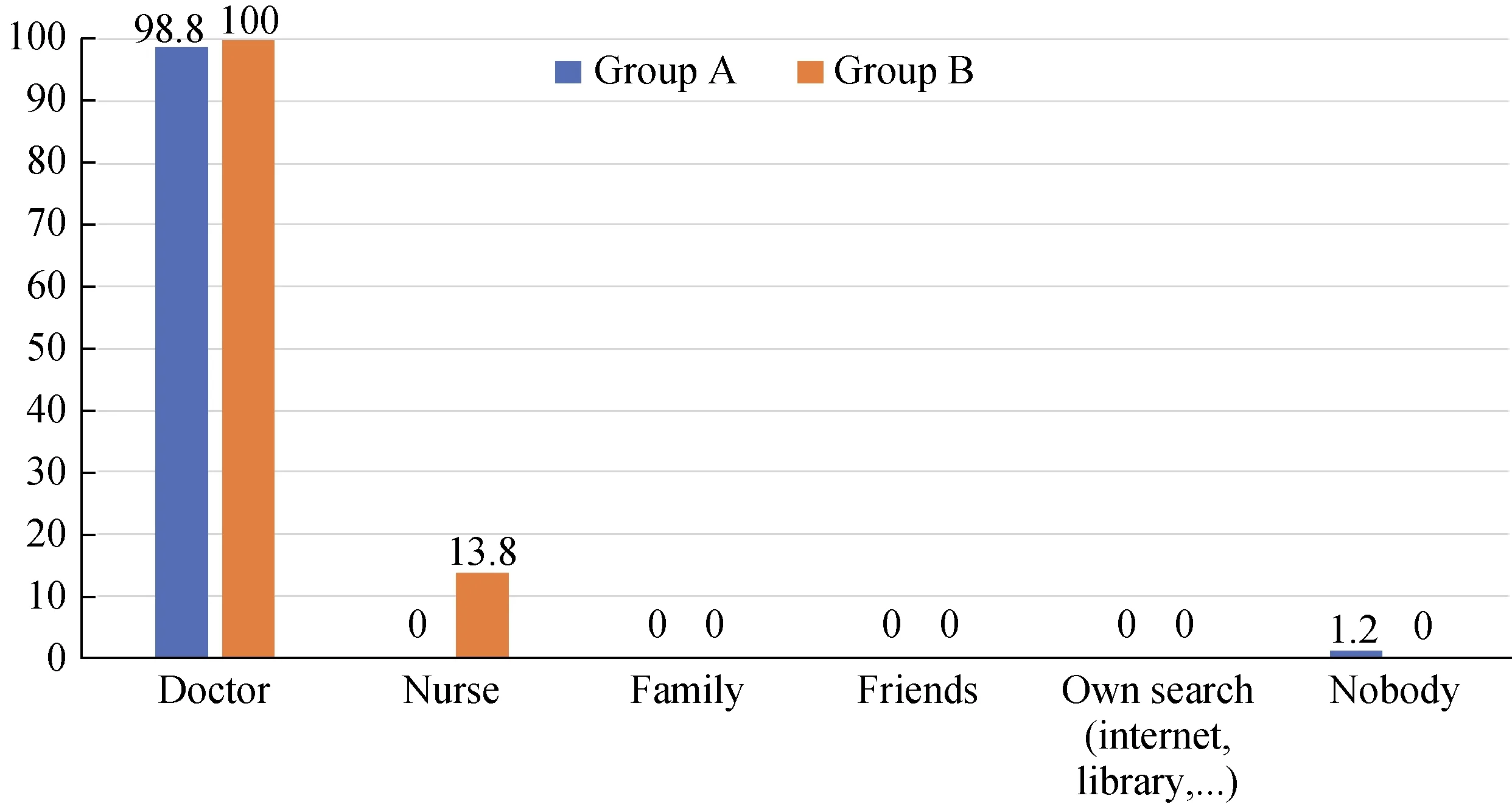
Figure 5. Sources of patient information after device implantation but before discharge from the hospital (several options were available for selection during the interview, e.g., doctors, nurses, family, etc). Numbers are percentages of patients in the respective group.Group A: octogenarians; Group B: patients ≤ 40 years of age.
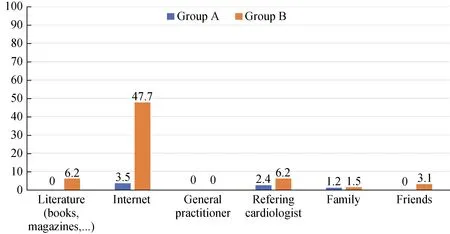
Figure 6. Sources of patient education after discharge from the hospital (several options were available for selection during the interview, e.g., the internet, literature, referring doctor, etc). Numbers are percentages of patients in the respective group. Group A: octogenarians; Group B: patients ≤ 40 years of age.
4 Discussion
The main outcomes of our study can be summarized as follows: (1) patients ≥ 80 years of age very much appreciate the opportunity to use HM systems and this particular telemedical technology for follow-up of their ICDs was generally very well accepted and highly ranked; their assessment of the personal advantages of the HM system did not differ significantly from the young patients using the same type of remote monitoring; (2) although all patients were satisfied with their HM system, almost half of the patients in both groups lacked a full understanding of its clinical benefits;and (3) doctors, not nurses were the main source of information and patient education on the use of HM, which may explain why many patients felt that there was not enough time devoted to or enough information provided on HM operation and benefits. These were also the most cited reasons for a post-discharge search for additional information on HM in the ≤ 40 years group. While only a minority of octogenarians perform such an additional search, the reasons were the same. Regarding this 3rdpoint, the main source of information used to better understand HM systems was the Internet, which carries an inherent risk that the information might be incomplete, inaccurate, or possibly out-of-date.
4.1 Clinical benefits of the HM system
The European Society of Cardiology (ESC) stated in their 2016 guidelines for heart failure that a high portion of deaths among patients with heart failure, especially those with milder symptoms, occur suddenly and unexpectedly.[6]ICDs provide both effective prevention of bradycardia and correction of potentially lethal ventricular arrhythmias. These same guidelines for heart failure management also state that patients should be included in multidisciplinary care programs designed to reduce the risk of rehospitalization and all-cause mortality. It is emphasized, in the context of telemedical care (class of recommendation IIb, level of evidence B), that automatic, daily multiparameter ICD monitoring using an HM system should now be actively recommended to patients with chronic heart failure and, therefore,should become the standard of care for these patients.
The impact of RM of ICDs has been investigated in many studies. These studies have consistently shown benefits such as improved clinical conditions, decreased morbidity and number of hospitalizations, decreased number of inadequate ICD discharges, significantly decreased number of ambulatory visits, earlier detection of adverse technical events, and better allocation of health care resources,etc.[7-11]With respect to mortality, the TRUECOIN[12]study evaluated data from 2405 patients who were monitored in the TRUST[13], ECOST[14], and IN-TIME[15]trials and specifically showed that the HM system reduces all-cause mortality, by 38%, in patients with an ICD, at one year.
The results of our study indicate that patients ≥ 80 years of age, as well as those ≤ 40 years of age, were both unlikely to have adequate information about all the clinical benefits offered by their HM system. Octogenarians typically and mistakenly thought that HM was used for emergency 24-h monitoring of their clinical condition (emergency surveillance) and were often completely unaware of how HM positively affects their health. Patients aged ≤ 40 years, however, seemed to have a better understanding. Almost half of these patients in our study were able to name at least one real clinical benefit derived from remote monitoring of their ICD. This topic should definitely be one of the focal points for HM-related information and education offered to all ICD implantation candidates, regardless of age.This one item has the potential to increase overall appreciation and acceptance of RM technologies.
The French study EUDCAT[16](patients aged 63.9 ± 12.8)found that the degree to which RM systems were understood was directly linked to the degree of acceptance.EDUCAT was also the first observational study to show that the overall degree to which patients understood HM was closely related to the patient’s age. Additionally, the study confirmed the importance of comprehensive education and training during the introduction of HM into the patient’s daily life. However, so far, there have been almost no studies looking specifically at patients ≥ 80 years of age, with the goals of finding and addressing potential concerns and problems linked to this age group. The steadily increasing population of those ≥ 80 years of age is often overlooked,but changing demographics and the ever-increasing average age of patients should compel us to give consideration to their needs since they stand to greatly benefit from new medical technologies, and as in this study, advancements in remote monitoring.[17,18]
4.2 Personal benefits of the HM system
One of the reasons for implementing HM is to enable patients to live full and high quality lives with fewer limitations, among which, for example, is the need for frequent ambulatory follow-up visits.[19]Both the octogenarians and the younger patients that we studied, appreciated the added sense of safety and security (approximately half of each group) HM brought them. Many patients also reported that they found “the green light” on the HM unit comforting, in that the indicator light gave them a sense of safety. They believed that if the light was on, everything was OK. However, some of the patients in both groups emphasized that there was inadequate feedback regarding data transfer—hence, this is a call to the industry, patients would feel better about HM if there was a clear indication that data transfer was successful, for example, (1) the date and time when the last data transfer occurred, (2) the overall success rate of data transfer, and (3) an indication that their data had been checked by a dedicated specialist.
Not surprisingly, a higher proportion of patients ≤ 40 years compared to octogenarians (48%vs. 33%) also appreciated the time and money savings, which would be otherwise spent traveling to ambulatory follow-ups. We cannot completely explain why approximately one-fifth of patients in both patient groups were unable to find any personal benefits of HM systems. It could be linked with a lack of adequate information and education on HM systems, but we cannot exclude personal skepticism towards remote monitoring technology. We were surprised that skepticism relative to RM was found in almost the same proportion in both patient groups since we would have expected a higher proportion in the elderly group of patients. In the event of limited health care resources, it might be necessary to fully educate all patients on HM first, and then offer HM to those expressing more “confidence” in the technology. This would increase both patient awareness and positive assessments of the care provided by the hospital and/or ambulatory units. In our hospital, the currently prevailing approach is to hand-out HM technology to all-comers without properly considering the patients´ needs and preferences.
4.3 Patient education and sources of information
Our findings show that although patients were educated by a doctor before discharge and also received an HM informational brochure, some patients still subsequently looked for additional information. Understandably, the proportion of patients over 80 years old who reported looking for additional information was significantly lower than the ≤40 years. old group (7%vs. 51%). The main drivers for the additional information searches were insufficient training time during the patient education process and insufficient information (or the unintelligibility of the information,which was reported in 5 cases total). In almost all patients,information on the HM system came from doctors, which could explain the above-stated problems. These health care professionals have limited time for patient education, which must be fit into all their other duties. With almost 100% of patients receiving some in-hospital HM education after their implantation procedure, but before discharge, we had hoped that the general level of understanding and knowledge of the clinical benefits the HM system, above and beyond those associated with the ICD itself, would have been better.
The solution to this disparity brings us to the role of the nurse-educator—nurses can instruct patients on the use and care of the HM systems and educate the patient’s family,both before device implantation and after discharge from the hospital. Nurses can work with each patient individually and take the time needed to fully educate them on HM. This type of nursing position (i.e., heart failure nurse or clinical specialist nurse) is commonplace in clinical and nursing practice in Western European countries. Unfortunately, no system for education and implementation of nurse competencies has been created that would lead to the creation of the nurse-specialist position in the Czech Republic. It can be assumed, especially in patients ≥ 80 years of age, that additional time is needed for proper patient education if we want them to fully understand the function and benefits of telemedicine. Based on the results of our study, we created a nurse-led educational program aimed at the most common issues associated with HM of ICDs and the impact of this technology on the patient’s life and clinically relevant events. This education is based on nurse-led instruction of all patients using remote monitoring, a brochure summarizing the main advantages of the HM system, and a short video available on YouTube (https://www.youtube.com/watch?v=QwBcZ_Ne144&feature=youtu.be - in the Czech language).
4.4 The relationship between the “degree of understanding” and patient concerns
In our study, 5% of octogenarians and 3% of patients aged ≤ 40 years expressed some degree of fear about using HM for the first time (no significant difference). Although this percentage is small, preferably, it should be zero. This effort is underlined by the fact that in our study of patients with an ICD 5% of octogenarians and 9% of patients ≤ 40 years suffered from psychological problems (mainly anxiety)while using RM. This could have easily been the result of insufficient education. The previously mentioned EDUCAT study noted that approximately 50% of patients with an ICD experienced depression or anxiety caused by their chronic disease as well as the knowledge that they were at risk of life-threatening arrhythmias or sudden cardiac death.[16,20]Another source of panic disorders and/or anxiety in the majority of these patients was the knowledge that there was a continuous risk of an unexpected electrical discharge, either appropriate or inappropriate.[21,22]
Better feedback regarding successful data transfer or monitoring by health care professionals was already mentioned. This related to several patients in our study who were anxious about whether their HM system was working or not, even though the green light on the HM unit was ON(or the “OK” message was displayed). Our patients with an ICD also reported a sense of foreboding, “i.e., that something bad would happen” relative to a potential failure of the patient HM unit or their ICD. While RM has become the preferred standard of ICD follow-up, its effect on the mental state of patients and the ability of patient education to redress some of these concerns, especially in patients older than 80 years of age, is not well known.[23]We believe that establishing patient trust in the RM system is the first step towards full acceptance of this modern technology. Again,there is enormous potential for nurses in this area. Nurses can educate patients in any age group; additionally, they can also be more proactive with patients and provide post-discharge care as needed. Nurses can also facilitate regular contact with patients and, if needed, provide more information about RM technology, or answers questions that might stem from the daily use of HM. In this sense, it could also benefit those patients who expressed a desire for more contact with a health professional as a social event.
4.5 Study limitations
To our knowledge, this is the first study comparing the acceptance of RM of ICD in elderly patients with patients ≤40 years of age. The study highlights the necessity for a thorough RM educational program for all patient groups.Since such a program falls outside what physicians can normally do, there is huge potential for this to be performed by specially educated nurses. The weak point of the trial was that it explored only patients already actively using the HM system, which included only patients considered competent to use HM [based on their pre-implantation screening(preselection bias)]. However, these are exactly the patients who would be most likely to use RM systems in daily clinical practice. Not all HM patients we contacted were willing to participate in our study; however, we strongly believe that the more than 90% of patients from each group that were included constitute a robust body of evidence capable of offsetting any bias we might have towards our conclusions.
4.6 Conclusions
The HM system used in our study received high marks and was much appreciated, even by patients over 80 years of age. The level of acceptance and potential psychological stress resulting from the RM technology appears to be about the same regardless of age group, despite the younger group being presumably more technically literate. These findings strongly support using the RM technologies in all competent population groups, regardless of age. However, we found that the majority of octogenarians either did not understand the clinical benefits of HM or mistakenly considered the HM system to also function as an emergency 24-hour surveillance system. These results show a need for improved education and more information regarding remote monitoring of ICD patients, especially in octogenarians, and not only during the initial learning phase, which usually occurs mainly during hospitalization but also during follow-up care.This is the area where we see a clear opportunity for nurse-specialists educated in telemedicine to provide supplemental information, while also making sure that each patient fully understands the information they were given.
Acknowledgments
The authors would like to thank Tom Secrest for proofreading the manuscript. The authors would also like to thank the Grant Agency of the University of South Bohemia in Ceske Budejovice (project registration No.: GAJU 079/2019/S) and the Foundation Cardiac Center Ceske Budejovice for their financial support covering article processing and publication charges. The authors report no conflicts of interest. The authors alone are responsible for the writing and content of this article.
 Journal of Geriatric Cardiology2020年7期
Journal of Geriatric Cardiology2020年7期
- Journal of Geriatric Cardiology的其它文章
- The prognostic role of high-sensitivity C-reactive protein in patients with acute myocardial infarction
- Associations of soybean products intake with blood pressure changes and hypertension incidence: the China-PAR project
- Modified subintimal plaque modification improving future recanalization of chronic total occlusion percutaneous coronary intervention
- Left atrial diameter and atrial fibrillation, but not elevated NT-proBNP,predict the development of pulmonary hypertension in patients with HFpEF
- Quality of life, physical performance and nutritional status in older patients hospitalized in a cardiology department
- Plasma big endothelin-1 is an effective predictor for ventricular arrythmias and end-stage events in primary prevention implantable cardioverterdefibrillator indication patients
