Modified subintimal plaque modification improving future recanalization of chronic total occlusion percutaneous coronary intervention
Ruo-Fei JIA, Long LI, Yong ZHU, Cheng-Zhi YANG, Shuai MENG, Yang RUAN, Xiao-Jing CAO,Hong-Yu HU, Wei CHEN, Jing NAN, Xiao-Wei XIONG, Jing-Jin LI, Jia-Yu WANG, Ze-Ning JIN,,#
1Department of Cardiology and Macrovascular Disease, Beijing Tiantan Hospital, Capital Medical University, Beijing, China 2Department of Cardiology, Beijing Anzhen Hospital, Capital Medical University, Beijing, China
Abstract Background Subintimal plaque modification (SPM) is often performed to restore antegrade flow and facilitate subsequent lesion recanalization. This study aimed to compare the safety and efficacy of modified SPM with traditional SPM. Methods A total of 1454 consecutive patients who failed a chronic total occlusion percutaneous coronary intervention (CTO PCI) attempt and underwent SPM from January 2015 to December 2019 at our hospital were reviewed retrospectively. Fifty-four patients who underwent SPM finally were included in this study. We analyzed the outcomes of all the patients, and the primary endpoint was recanalization rate, which was defined as Thrombolysis in Myocardial Infarction (TIMI) grades 2-3 flow on angiography 30 to 90 days post-procedure. Results The baseline characteristics were similar between the two groups. In the follow-up, the recanalization rate was noticeably higher in the modified SPM group compared with the traditional SPM group (90.9% vs. 62.5%, P < 0.05). The proposed strategy in the modified group was more aggressive, including a larger balloon size (1.83 ± 0.30 vs. 2.48 ± 0.26 mm, P < 0.05) and longer subintimal angioplasty (0.59 ± 0.16 vs. 0.92 ± 0.12 mm, P < 0.05).Also, the common use of a Stingray balloon and guide catheter extension resulted in improvement of patients in the modified SMP group(12.5% vs. 100%, P < 0.05). Conclusion Modified SPM, which is associated with a high likelihood of successful recanalization, is an effective and safe CTO PCI bail out strategy.
J Geriatr Cardiol 2020; 17: 393-399. doi:10.11909/j.issn.1671-5411.2020.07.009
Keywords: Chronic total occlusion; Recanalization; Subintimal plaque modification
1 Introduction
Chronic total occlusions (CTOs) are common in patients with coronary artery disease (CAD) and often lead to refractory angina and impaired quality of life.[1–5]Successful revascularization with contemporary percutaneous coronary intervention (PCI) could relieve symptoms and improve clinical outcomes. However, these procedures remain challenging with a 10%–15% failure rate at experienced centers, whereas contemporary CTO PCI techniques have continuously improved.[6,7]Moreover, cutting-edge techniques, such as retrograde wire, subintimal tracking and re-entry (STAR),[8–10]and control antegrade and retrograde subintimal tracking(CART) may result in serious complications in some complex cases, especially in patients with a previous history of coronary artery bypass grafting (CABG).[11–14]
When CTO PCI fails or potential risk exceeds the anticipated benefits, subintimal plaque modification (SPM) may be employed as a supportive treatment strategy. SPM is typically used to describe the “investment procedure”, in which when the distal knuckle fails to re-enter the true lumen distally, balloon angioplasty is performed in the subintimal space to partly restore antegrade flow or increase the success rate of CTO PCI with no stents implanted. Recent evidence shows that patients undergoing SPM can noticeably benefit from restoring antegrade flow, which relieves symptoms, improves quality of life, and increases the success rate of CTO PCI.[15–18]
The Stingray balloon (Boston Scientific Corporation,Marlborough, MA, USA) has been used widely on CTO PCI in our center since 2017. Upon this novel equipment and the continuous development of the techniques and algorithms of CTO PCI, we designed a modified SPM different from traditional SPM in multiple aspects, such as whether it is used with or without a Stingray balloon, changes to the ratios of balloon size and target vessel size, and the range of SPM. Therefore, we proposed to compare the safety and efficacy between the modified and traditional SPM.
2 Methods
2.1 Study populations
This retrospective study following patients who underwent SPM from January 2015 to December 2019 in the Department of Cardiology at Beijing Tiantan Hospital (Beijing, China) after a CTO PCI procedure included 54 cases out of a total of 1454 reviewed. Inclusion criteria were as follows: (1) SPM procedures were undertaken by experienced cardiologists to avoid failure of CTO PCIs or exceeding the potential risks from anticipated benefits after evaluating the radiation dose, contrast volume, operative time, and risks of other therapeutic approaches; and (2) 30 to 90 days after SPM, a repeat coronary angiography/intervention was performed. Exclusion criteria were as follows:(1) patients aged < 18 or > 80 years old; (2) presence of acute or chronic inflammatory diseases; or (3) no dual antiplatelet therapy for contraindications.
The present study was approved by the Ethics Committee of Beijing Tiantan Hospital, Capital Medical University (Beijing, China), and performed according to the Declaration of Helsinki. Additionally, all eligible patients signed a written informed consent form.
2.2 Definition of endpoints
The primary endpoint was recanalization, defined as Thrombolysis in Myocardial Infarction (TIMI) grades 2-3 flow on angiography after 30 to 90 days follow-up.
Coronary lesions with TIMI grade 0 that lasted for three months or more were defined as CTO.[19]When CTO PCI fails, the role of SPM is extremely significant. The modified SPM should meet the following criteria, otherwise it is defined as traditional SPM: (1) a Stingray balloon was used for antegrade dissection and re-entry (ADR), regardless of whether the guidewire entered the distal true lumen; (2)balloon angioplasty was undertaken during the SPM, and a balloon-to-vessel ratio of 0.75: 1 or 1: 1 was recommended;and (3) the length of subintimal angioplasty should be closer to or longer than the length of the occluded lesions (at least≥ 50%); and (4) once shifted to ADR strategy, all patients had a guide catheter extension to block antegrade flow and minimize the subintimal hematoma. According to the above-mentioned criteria, the present study included 32 patients with traditional SPM and 22 patients with modified SPM.
2.3 Data collection
Patients’ demographic and clinical characteristics, such as age, sex, risk factors for CAD, medical history, the Canadian Cardiovascular Society (CCS) grade, and coronary angiography findings, were collected using a standard case report form. In addition, significant data about SPM, Stingray balloon, balloon-to-vessel ratio, and the length of subintimal angioplasty were collected. The length of subintimal angioplasty was defined as SPM length divided by occluded lesion length and categorized into 25%, 50%, 75% and 100% groups. Intravascular ultrasound (IVUS) was employed to indicate whether the guidewire was in the distal true lumen, and the Japan-chronic total occlusion (J-CTO)score was calculated using Morino,et al.’s method.[20]All the information about coronary angiography and procedures was evaluated by two experienced cardiologists. Postoperative complications were recorded (i.e., death, coronary artery perforation, stroke, acute stent thrombosis,[21]emergency surgery, and bleeding at access site).[22]
2.4 Statistical analysis
Continuous data were presented as mean ± SD or median(interquartile ranges) and analyzed by the Student’st-test or the Mann–WhitneyUtest. Categorical variables were summarized as number (percentages) and compared using the chi-square test. For continuous variables, normally distributed data were evaluated using the Kolmogorov-Smirnov test. All statistical analyses were undertaken with SPSS 20.0 software (IBM, Armonk, NY, USA), andP< 0.05 was considered statistically significant.
3 Results
From January 2015 to December 2019, 1,454 CTO PCIs were performed in our hospital, of which 226 (15.5%) patients had a prior unsuccessful attempt. Among them, 73(32.3%) patients underwent SPM. Nineteen patients did not accept angiography within 90 days. Eventually, a total of 54 eligible patients were included in the final analysis, of which 22 patients underwent modified SPM (modified SPM group) and 32 patients received traditional SPM (traditional SPM group). Figure 1 shows the flowchart of the study.
The patients’ baseline and clinical characteristics are presented in Table 1. There were no significant differences between the two groups in history of smoking (68.8%vs.59.1%,P= 0.57), hypertension (78.1%vs.72.7%,P= 0.75),type 2 diabetes mellitus (40.6%vs.59.1%,P= 0.268),chronic kidney disease (25.0%vs.18.2%,P= 0.742), or atrial fibrillation (15.6%vs.9.1%,P= 0.687). Additionally,the two groups were well matched for median age, medical history, CCS grade, and baseline left ventricular ejection fraction (LVEF).

Figure 1. Study flowchart. *Modified SPM technique was designed in Oct, 2018. Therefore, almost all patients received the procedure in 2019. CTO: chronic total occlusion; PCI: percutaneous coronary intervention; SPM: subintimal plaque modification.

Table 1. Baseline clinical characteristics of study population.
Lesion characteristics at baseline were well matched between the two groups in terms of percentage of previously undergoing CTO target vessels (18.8%vs.18.2%,P= 0.99),guidewire in distal true lumen (21.9%vs.27.3%,P= 0.75),and calcification present (71.9%vs.59.1%,P= 0.67) (Table 2).Additionally, the lesion- and reference vessel-related parameters were similar between the groups, including length of the lesion (47.53 ± 17.34vs.40.36 ± 20.80 mm,P= 0.18),proximal reference vessel diameter (2.77 ± 0.36vs.2.66 ±0.27 mm,P= 0.22), and distal reference vessel diameter(2.05 ± 0.49vs.2.09 ± 0.36 mm,P= 0.59). Furthermore,there were no significant differences between the two groups in CTO target vessels, J-CTO scores, or complications.
Most importantly, as presented in Table 3, compared with the traditional SPM group, the larger balloon size was used in the modified SPM group (1.83 ± 0.30vs.2.48 ±0.26 mm,P< 0.05). Similarly, the length of subintimal angioplasty in the modified SPM group was significantly longer than that in the traditional SPM group (0.59 ± 0.16vs.0.92 ± 0.12 mm,P< 0.05). This revealed that the modified SPM strategy was more aggressive. In the traditional SPM group, the guide catheter extension and Stingray balloon were scarcely utilized. As the ADR strategy has been modified, all the cases received Stingray balloon and guide catheter extensions in the modified SPM group (12.5%vs.100%,P< 0.01). In both groups, a few cases used IVUS to reveal whether the guidewire was in the distal true lumen;this information was the basis to select balloon size and dilation pressure (< 25%).
In the follow-up, the primary endpoint showed that the recanalization rate was markedly higher in the modified SPM group compared with the traditional SPM group(90.9%vs.62.5%,P< 0.05). Final successful revascularization (81.3%vs.95.5%,P= 0.73) and duration of follow-up after SPM were not significantly different between the two groups (56.38 ± 19.32vs.51.36 ± 19.69 days,P= 0.18). A representative case in the modified SPM group is described in Figure 2.
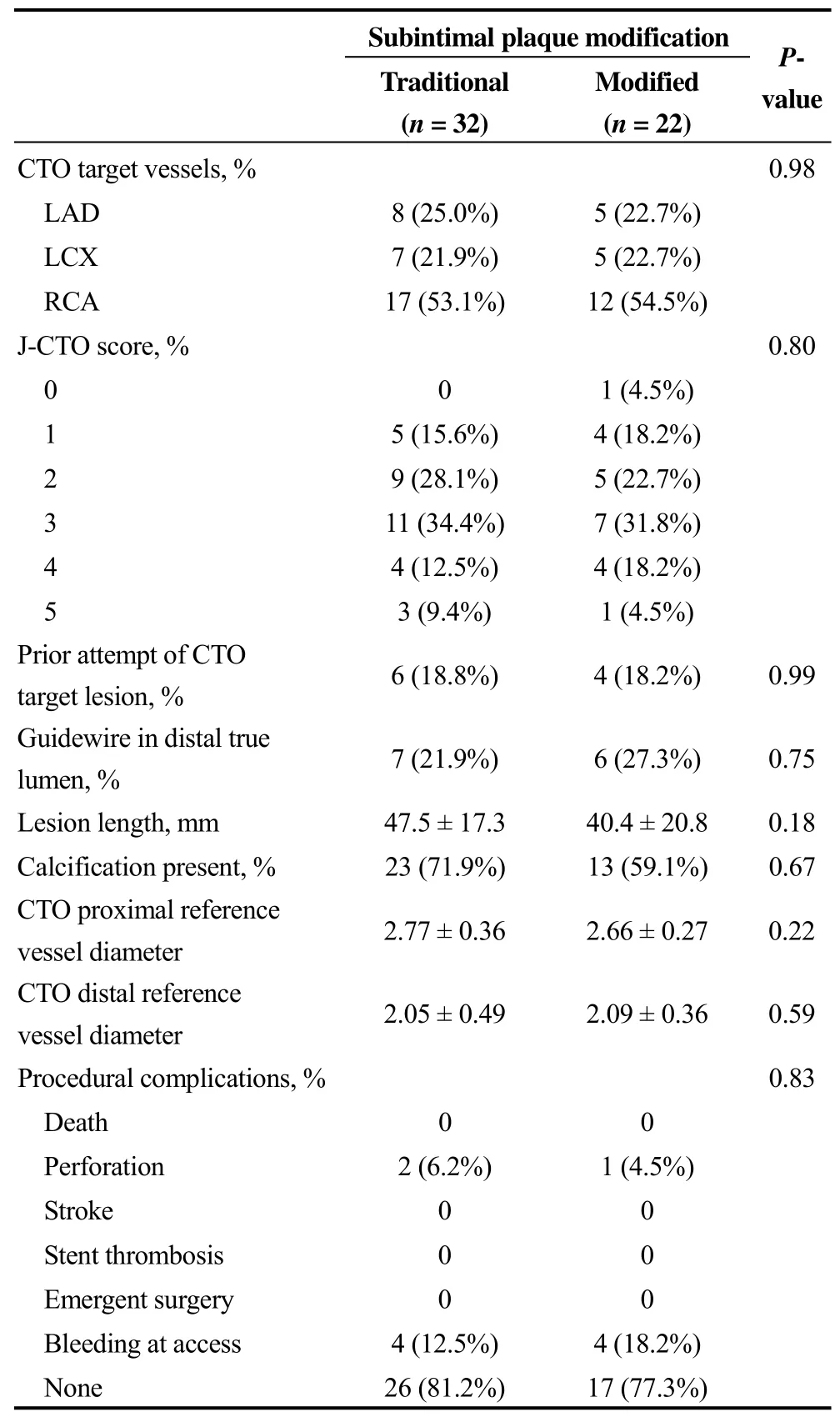
Table 2. Baseline lesion and procedural characteristics of study population.
4 Discussion
In this study, we presented a new concept for the modified SPM technique which included four criteria: (1) a Stingray balloon was used for antegrade dissection and re-entry (ADR), regardless of whether the guidewire entered the distal true lumen; (2) balloon angioplasty was undertaken during the SPM, and a balloon-to-vessel ratio of 0.75:1 or 1: 1 was recommended; (3) the length of subintimal angioplasty should be closer to or longer than the length of the occluded lesions (at least ≥ 50%); (4) once shifted to ADR strategy, all patients had a guide catheter extension to block antegrade flow and minimize the subintimal hema-toma. Also, the follow-up time for subsequent intervention after SPM should be 30 to 90 days.
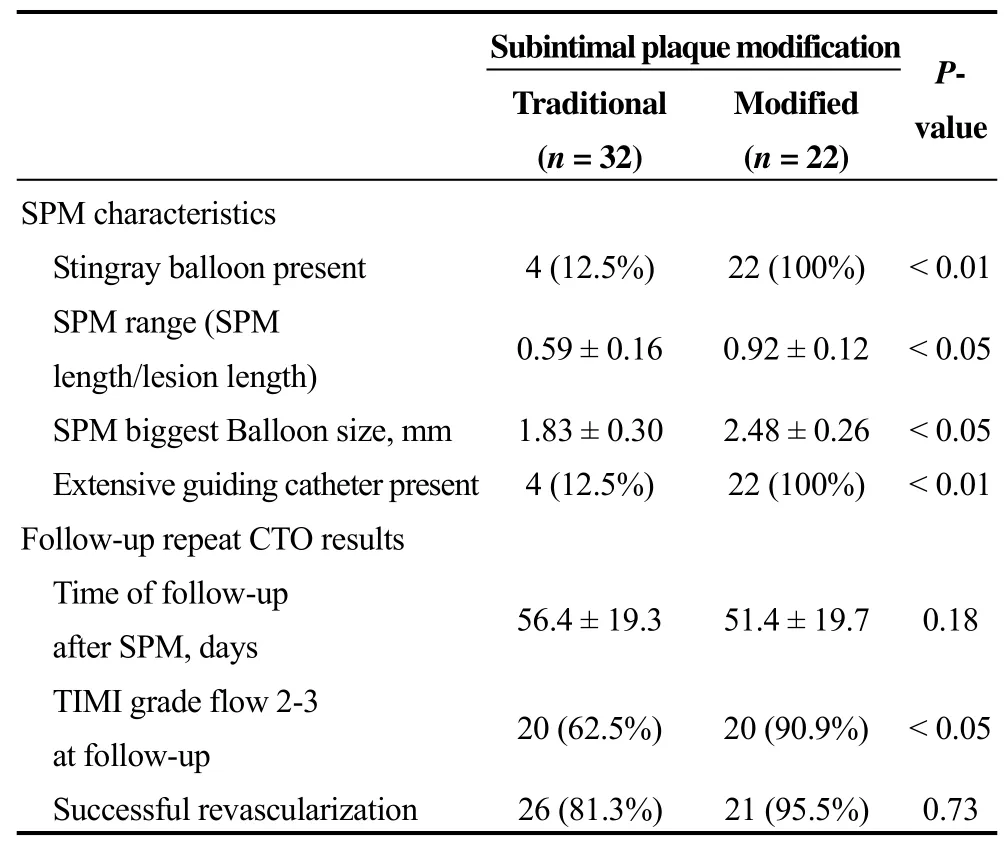
Table 3. SPM characteristics and outcome of study population.
This retrospective study showed that the modified SPM technique could increase the percentage of cases with TIMI grades 2–3 flow in subsequent intervention compared with the traditional SPM technique. In the follow-up, angiography uncovered that the recanalization rate was significantly higher in the modified SPM group compared with the traditional SPM group (90.9%vs.62.5%,P< 0.05). The modified SPM strategy was more aggressive, which resulted in a larger balloon size (1.83 ± 0.30vs.2.48 ± 0.26 mm,P<0.05) and longer length of subintimal angioplasty (0.59 ±0.16vs.0.92 ± 0.12 mm,P< 0.05). Additionally, in Table 3,the common use of the Stingray balloon and guide catheter extension resulted in improvement of patients in the modified SMP group (12.5%vs.100%,P< 0.01).
We hypothesized possible reasons for the positive effects of the modified SPM technique: (1) although the Stingray-based ADR cannot always re-wire from the subintimal space to the true lumen, the wire located in the subintimal space should be closer to the true lumen compared to cases without a Stingray balloon; (2) the more aggressive balloon size and length of subintimal angioplasty can destroy the recanalization of the occluded lesion during healing; (3) the wide application of the guide catheter extension can effectively control the subintimal hematoma, and this strategy increases the rate of recanalization; and (4) the adaptive subsequent intervention time is highly important. All the differences between the two techniques and possible potential principles are illustrated in Figure 3.

Figure 2. Recanalization after contemporary SPM technique: 30 day follow-up. (A): Angiogram shows a long CTO lesion of the mid right coronary with blunt proximal cap (arrow), the J-CTO score was 2; (B): the antegrade wire escalation strategy used Fielder XT-A and Pilot200; (C): after entering the subintimal space, antegrade dissection re-entry was performed with Gaia third based on the Stingray balloon(arrow) and extensive guiding catheter (arrow); (D): after demonstrating that the wire was in the subintimal space, the modified SPM technique was performed with a 2.5 mm balloon and aggressive angioplasty length (between two arrows); (E): 30 days later, a repeat angiogram demonstrated recanalization with TIMI 2 grade flow; and (F): after the true lumen was entered with the Fielder XT wire, balloon angioplasty and implanted stents, the final angiogram was made. CTO: chronic total occlusions; SPM: subintimal plaque modification; TIMI: thrombolysis in myocardial infarction.

Figure 3. Illustration for contemporary SPM technique. (A): The traditional SPM technique. The guidewire crosses into the subintimal space and angioplasty with a small balloon is performed. The SPM length range was limited. (B): The contemporary SPM technique. ADR was based on the Stingray balloon and extensive guiding catheter. This SPM technique was more aggressive, with a larger balloon size and longer SPM length range. ADR: antegrade dissection and re-entry; SPM: subintimal plaque modification.
The “SPM and investment” technique was derived from the STAR technique. The STAR technique has been described as a strategy to use in case of failure of cross coronary occlusion with approved conventional approaches.This technique entails creating a dissection plane in the coronary artery with distal re-entry. Colombo,et al.[8]proposed an approach similar to the one utilized in treating some peripheral artery occlusions and created a subintimal dissection with distal reentry. In STAR, a subadventitial cleavage plane is created by advancing a knuckled polymer-jacketed guidewire to allow a blunt dissection between the anatomical planes of the vessel, with the aim to achieve re-entry into the distal true lumen. It was demonstrated that the STAR technique produced an acceptable procedural success in patients with selected CTOs in whom attempts to reanalyze the vessel with conventional wires or dedicated CTO devices had failed. Thereafter, Wilson,et al.[23]reported that procedural failure in the setting of CTO PCI may have different causes. In case of successful negotiation of the proximal cap, with failed re-entry of the subintimal passage of the guidewire, angiography should be repeated in 4–6 weeks to assess vessel reconstitution. Prior to case abandonment, actions to consolidate any lesion modification in the current procedure may facilitate future success.[23]Hirai et al. determined the impact of SPM on early health status following unsuccessful CTO PCI. They studied 138 patients who underwent unsuccessful CTO PCI in a 12-center CTO PCI registry. Safety was assessed by comparing in-hospital outcomes of patients undergoing unsuccessful CTO PCI with and without SPM. The association between SPM and health status was quantified using the Seattle Angina Questionnaire Summary Score (SAQSS). They indicated that SPM was independently associated with better patient-reported health status at 30 days.[17]Hirai,et al.[17]demonstrated that the STAR technique was not appropriate for routine use during CTO PCI due to side branch loss and long stent length, leading to high restenosis and re-occlusion rates. They also suggested that the STAR technique may become an important element of the expanded hybrid algorithm. Four parameters are constantly being evaluated during the procedure: radiation dose, contrast volume, procedure time and the risk of the remaining treatment options, to determine if it is necessary to stop the procedure.[16]Goleski,et al.[15]assessed CTO cases with STAR and deferred stenting (DSS). In their research, STAR was performed in 45 cases and DSS in 32 cases, and the median inter-procedure time was 2.4 months. Technical success was achieved in 28(88%) patients. They emphasized that DSS was particularly attractive in the right coronary artery and in the left circumflex artery branches, rather than the left anterior descending artery, where diagonal branches might be at risk. Xenogiannis,et al.[24]investigated the frequency of SPM and outcomes of subsequent PCIs in a large, contemporary multicenter CTO PCI registry. They found that SPM as a bailout strategy in CTO PCI was associated with a high likelihood of successful revascularization during repeat CTO PCI attempts, with acceptable risks.[24]
The present study and the literature indicate that SPM is a safe and effective bailout strategy. Moreover, this is the first research that defined four criteria for modified SPM and compared the cases who met these criteria with traditional SPM cases. However, further studies are required to confirm our findings, and develop new criteria for the modified SPM technique.
The current study has several limitations. First, it was an observational retrospective study that involved a limited number of patients conducted in a single center, without long-term follow-up. Second, the criteria were designed in 2018. Therefore, all the traditional SPM patients were studied from 2015 to 2018, whereas modified SPM patients were assessed from 2018 to 2019. Third, not all patients received IVUS to confirm the location of the guidewire in the distal vessel. Hence, prospective and randomized studies are warranted to evaluate the modified SPM technique in the future.
In conclusion, SPM is a safe and effective bailout strategy in CTO PCI. Compared with the traditional SPM technique, a Stingray balloon-based modified SPM technique with guide catheter extension and aggressive balloon size and length of subintimal angioplasty can increase the recanalization rate significantly by 30–90 days post-procedure.
Acknowledgements
The authors thank Zhiyun Data Technology Co. LTD for data abstraction and analysis.
 Journal of Geriatric Cardiology2020年7期
Journal of Geriatric Cardiology2020年7期
- Journal of Geriatric Cardiology的其它文章
- The prognostic role of high-sensitivity C-reactive protein in patients with acute myocardial infarction
- Associations of soybean products intake with blood pressure changes and hypertension incidence: the China-PAR project
- Left atrial diameter and atrial fibrillation, but not elevated NT-proBNP,predict the development of pulmonary hypertension in patients with HFpEF
- Quality of life, physical performance and nutritional status in older patients hospitalized in a cardiology department
- Remote monitoring of implantable cardioverters defibrillators: a comparison of acceptance between octogenarians and younger patients
- Plasma big endothelin-1 is an effective predictor for ventricular arrythmias and end-stage events in primary prevention implantable cardioverterdefibrillator indication patients
