Food insecurity and other possible factors contributing to low birth weight: A case control study in Addis Ababa, Ethiopia
Degemu Sahlu, Negussie Deyessa, Naod Firdu, Sahle Asfaw
1Department of Preventive Medicine, School of Public Health, Addis Ababa University, Addis Ababa, Ethiopia
2Menelik II College of Health and Medical Science, Kotebe Metropolitan University, Addis Ababa, Ethiopia
ABSTRACT
KEYWORDS: Household food insecurity; Mothers; Low birth weight; Neonates
1.Introduction
The health of the mother during pregnancy is very important to give birth to healthy baby.Birth weight is a strong predictor of infant development and existence.Child born with low birth weight starts life with challenges and has lower survival rate[1].
The World Health Organization defines low birth weight as having a birth weight of below 2 500 g[2].Low birth weight and premature birth are the important predictors of perinatal existence,child diseases and death.These may also determine the chance of developing illness in later life.Low birth weight affects all ages of human being and low delivery weight neonate may develop into stunted young and adult person and finally, undernourished mother of reproductive age.The mother with this situation brings low birth weight child[3].Complex and multiple factors are contributing to the existence of intrauterine growth retardation.Among which,the maternal environment is the major predictor of birth weight[3].Most of low birth weight in underdeveloped nations is as a result of intrauterine growth retardation.And occurrence of low delivery weight can be minimized through early identification of susceptible pregnant mothers.
In 2012, the World Health Assembly planned to reduce low birth weight by 30% that is from approximately 20 million to about 14 million in 2025.This in turn accounts almost 2.3% decrement per year between 2012 and 2025[4].
Child death rate had been decreased significantly in Ethiopia.On September 13, 2013 the Federal Ministry of Health of Ethiopia and United Nations International Children's Emergency Fund publicized that Ethiopia successfully achieved millennium development goal 4 three year ahead of timeline, 2015[5].However, the report and evidences elsewhere clearly showed that the contribution of neonatal mortality to infant mortality in the country is still far behind in reducing neonatal mortality rate.Approximately 42% of the under-5 mortality in Ethiopia is attributable to neonatal deaths and 80% of neonatal deaths are attributable to low birth weight[6].
Nutritious food is very important for healthy pregnancy.It has an influence on premature birth and low birth weight.A number of health outcomes have been affected by inadequate access to food.For instance, it is related with self-reported health status among adult and children and depression and anxiety in mothers[7-9].The impact of food insecurity on reproductive outcome is not wellestablished.The relationship between household food insecurity and low birth weight were inconsistent and not well studied particularly in Ethiopia.Therefore, this stud aimed to determine the relationship between low birth weight and household food insecurity in Addis Ababa, Ethiopia.
2.Methods and materials
2.1.Study design, period and area
Institution based unmatched case control study design was applied among mother-new born pairs in Addis Ababa, Ethiopia.The study was conducted at four governmental hospitals namely, Black Lion,Zewditu, Gandhi and St.Paulos Hospitals in Addis Ababa from February 1, 2017 to May 15, 2017.Addis Ababa is the capital city of Ethiopia with total population size of 3 435 030.The proportion of female in the city were 52.7% and out of total females, 1 161 441(64%) were in reproductive age group[10].Food insecurity was a problem in Addis Ababa Ethiopia which accounted 58.16% of households as of the 2012 study[11].
2.2.Study participants
All mothers who gave term newborns with their neonates in the period February 1-May 15, 2017 at four governmental hospitals in Addis Ababa were considered to be included in the study.Mothers who gave term neonates weighing below 2 500 g during February1-May 15, 2017 served as the case group.Mothers gave term neonates weighing ≥2 500 g during the same time period served as the control group.Mothers whose baby had congenital anomalies, stillbirth,from multiple birth and above and mothers whose gestational ages unknown by interview or from card were excluded from the study.
2.3.Study variables
The dependent variable in this study was birth weight less than 2 500 g.The independent variables assessed in this study included socio-economic factors like maternal age, education level,occupation, residence, current married status, household wealth and family size; obstetric factors including history of low birth weight, parity, history of abortion, birth interval and age at first birth; sanitation and hygiene factor; behavioral factors like smoking and alcohol consumption; genetic factors including mother height and infant sex; nutritional factor especially food insecurity, weight gain during pregnancy and maternal mid-upper arm circumference(MUAC); toxic exposure during pregnancy including malaria,hypertension, urinary tract infection and anemia.Maternal MUAC was a potential indicator of maternal nutritional status.It indicated the protein reserves of a body, and a thinner arm reflected wasted lean mass, i.e.malnutrition[12].MUAC was measured by MUAC tape and re-categorized as <23 cm (poor nutritional status) and ≥23 cm(nutritional status was not poor).
2.4.Measurement tool
The data was collected by using structured questionnaire which was adapted from standard literature[13].The neonate weight was measured by using standard beam balance in the delivery room immediately after delivery or within the first hour by trained midwifery.The measurements were rounded to nearest 100 g.Maternal MUAC was also taken by using non stretchable MUAC tape to estimate the nutritional status.It was taken when the mother became stable after delivery.
2.5.Data quality control
The questionnaire was prepared in English and translated into Amharic to increase understanding of the respondents and translated back to English to keep consistency of the question.The sample of questionnaire was pre-tested on mother out of the study area.The pre-test was done to insure clarity, wording, and logical sequence and skip pattern of the questionnaire.Essential amendment was taken.Training was given to the data collector and supervisor on objective of the study, technique and procedure that they followed during interview and anthropometry measurement.Close supervision was done by supervisor and principal investigator.
2.6.Sample size
The total sample size was calculated by using statistical program of Epi Info version 7.Sample size determination for proportion in two populations was used.One major exposure variable that was household food insecurity was taken into consideration during sample size calculation.The following assumptions were taken to come up with the final sample size; 95% confidence level, power of 80% and case to control ratio of 1:3.The proportion of food insecurity among mothers who delivered more than 2 500 g neonates was 58.16%[14]with detection of 15% difference in food insecurity among cases.Based on the above assumptions, with additional 10% for non-response rate, total sample size required to detect the existing difference was 480 (120 cases and 360 controls).
2.7.Sampling technique and procedure
There were 11 public hospitals in Addis Ababa.From these public hospitals four hospitals were selected by simple random (lottery)technique.To allocate the total sample size to each hospital, total number of women who gave birth in the selected hospitals in the last two months was considered before the actual data collection period.Allocation of the sample size to each health facility was made by using proportion to population size of the facilities (Figure 1).In each selected health facility, selection of cases was done as a case found, and the next three eligible children were the controls.From planned 480 mother-neonate pairs, only 468 participants were involved in the study accounting 97.50% response rate.
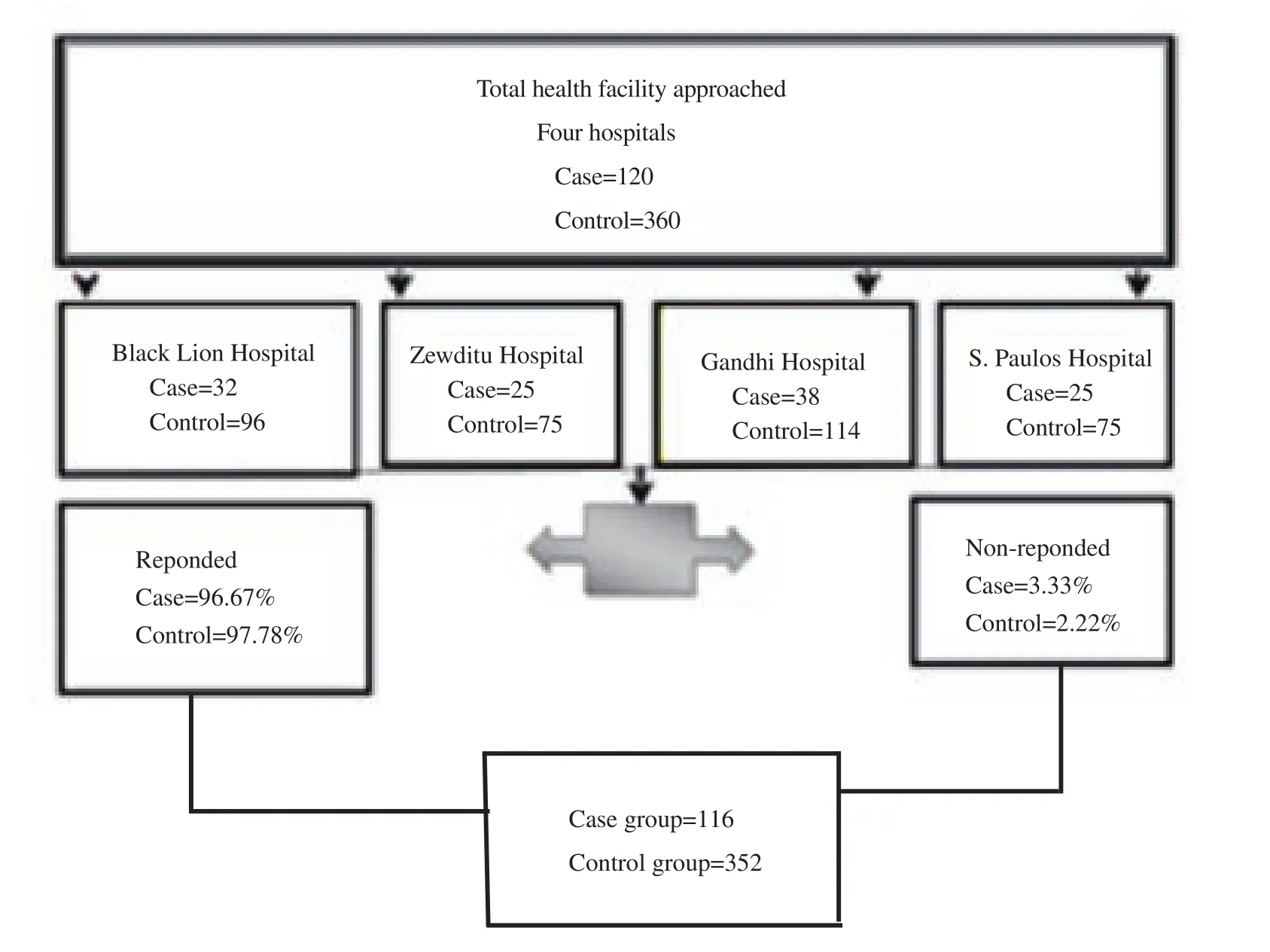
Figure 1.Summary of study population among selected hospitals in Addis Ababa, Ethiopia.
2.8.Food insecurity assessment
According to the United States Agency for International Development (USAID), food security was defined as a state in which all people at all times had both physical and economic access to sufficient food to meet their dietary needs for a productive and healthy life[13].The USAID in 1992 also acknowledged food insecurity as one of the three most important underlying causes of malnutrition[13].Because of its complexity, multidimensional concept, measuring food insecurity become a challenge for both researchers and practitioners too.To solve this challenge, USAID Food and Nutrition Technical Assistance project prepared Household Food Insecurity Access Scale, which provided a means for food security programs to easily measure the impact of their programs on the access component of household food insecurity[13].The method was based on the idea that the experience of food insecurity (access)caused predictable reactions and responses that can be captured and quantified through a survey and summarized in a scale[13].It used nine generic questions that represented apparently universal domains of the household food insecurity experience and could be used to assign households and populations along a continuum of severity, from food secure to severely food insecure.Of course,understanding and measuring the impact of programming on the utilization component of food insecurity was equally important, but was better accomplished by using other measurement tools, such as anthropometric indicators[13].
2.9.Data management and analysis
The collected data was entered by using Epi-Data version 3.1 (The EpiData Association, Odense Denmark) and exported to Stata 14 software (Stata Corp, USA) for cleaning, recording, categorizing and analyzing.All variables were changed to categorical and polytomic type.
Household food insecurity was assessed by using household food access scale.Nine questions with dictums (yes/no) response options and nine questions with quantitative response options were used to assess the household food security.The respondent were asked about question (Q) related to anxiety and uncertainty about the household food supply (Q1), insufficient quality (includes variety and preferences of the type of food) (Q2, Q3 and Q4).Insufficient food intake and its physical consequences in the past four weeks with their frequency (Q5, Q6, Q7, Q8 and Q9).The response of the household in this case mothers was re-categorized as secured(household experiences none of the food insecurity access conditions or just experiences worry once or twice in the past four weeks) and insecure (household experiences one of the food insecurity access conditions, but not just experiences worry once or twice in the past four weeks).Categorization was done by the help of Stata 14 software.
Wealth status of the participants was created with the help of principal component analysis using asset variable, household characteristic, water source and latrine type.Descriptive analysis was done to determine the socio-demographic characteristic of women.The Chi-square (χ2) was computed to show whether the difference was significant or due to chance.Bivariate analysis was done to see the association between independent and outcome variables.Those variables with 95% confidence interval (CI) and P-value <0.05 during the bivariate analysis were included in the multiple logistic regression analysis to assess the relative effect of confounding variables.After multivariate analysis had done, adjusted odds ratio(OR) was used to measure the strength of association between the dependent variable and the independent variable, while 95% CI was used to assess whether the association was significant.
2.10.Ethics approval and consent to participate
The study was approved by Research and Ethics Committee of Addis Ababa University School of Public Health (approval No.aau054217).Before data collection, a formal letter from Addis Ababa University, School of Public Health Ethical Clearance Committee was submitted to the relevant and concerned bodies of the hospitals.Permission was obtained from head of selected hospitals.Verbal consent was obtained from study participants after clear explanation about the purpose, benefit and risk of the study and also their right on decision of whether or not participating in the study.Confidentiality was maintained by omitting their names and personal identification.
3.Results
3.1.Description of socio-demographic characteristic mother in case and control group
About 40% of mothers were within age group 25-29 years old, and 75% of these age group mothers were in the control group.The mean age of the respondents was (26.7±5.2) years old.Almost half of mothers in the control group and more than half of mothers in the case group were orthodox in religion.Nearly half of mothers both in the case and control groups were housewives.Concerning to educational level of the mothers, nearly 43% (75.5% controls and 24.5% cases) of them were in the primary educational level and 14%(29.0% cases and 71.0% controls) had no formal education.Thirty one percent (17.0% from the cases and 83.0% from the controls) of respondents were in the fourth wealth quintile group (Table 1).
3.2.Food security status of mothers
Depending on Household Food Insecurity Access Scale, which was developed by USAIDS, this analytical study comes up with thefollowing finding.Of total respondents of this study, about 86.11%(403/468) of them were food secured, and from these 91.48%(322/352) in the control group and 69.83% (81/116) in the case group.Mild food insecurity in the case group [12.93% (15/116)]was higher than the control group [5.11% (18/352)].Moderate food insecurity in the case and control groups was found to be 14.65%(17/116) and 3.13% (11/352), respectively.Severe food insecurity was 2.59% (3/116) and 0.28% (1/352) in the case group and the control group, respectively (Figure 2).

Table 1.Socio-demographic profile of mothers among selected hospitals in Addis Ababa, Ethiopia from February 1, 2017 to May 15, 2017.

Table 2.Obstetric, antenatal care related, toxic exposure during pregnancy profile of mothers and its association with low birth weight among selected hospitals in Addis Ababa, Ethiopia from February 1, 2017 to May 15, 2017.
3.3.Obstetric characteristic and antenatal care follow up result of the study participants
From total 468 mothers who had participated in the study, about 52% were primigravida, out of these mothers 29.2% in the case group and 70.8% in the control group.About 95% of mother gave the first birth at age 18 years and above.MUAC was used to assess nutritional status of mother and majority of mothers (57.0%) in case group had MUAC less than 23 (Table 2).
3.4.Potential confounder control
To assess the independent effect of food insecurity on low birth weight, potential confounder should be controlled.Identification of these confounders was analyzed by using multiple regressions.For this, all variables with 95% CI and P-value <0.05 during the bivariate analysis were included in the multiple logistic regression analysis(Table 3).
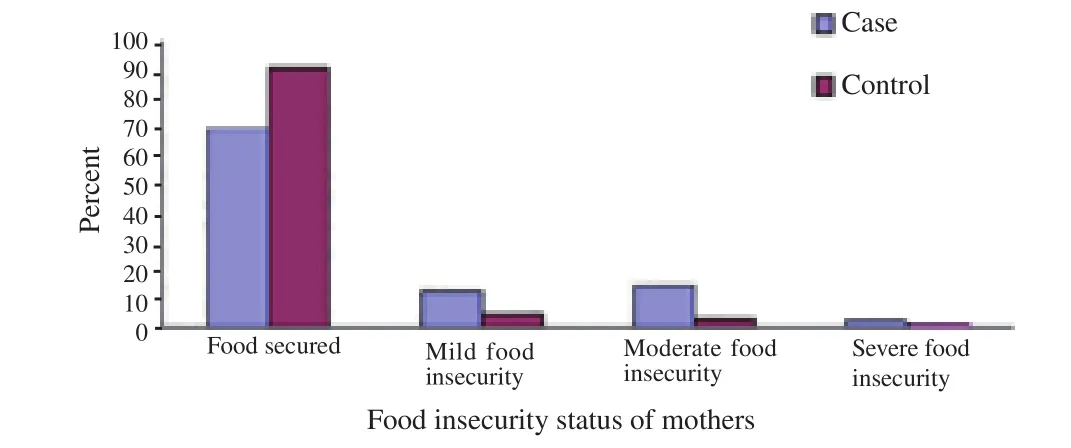
Figure 2.Food insecurity status among selected hospitals, Addis Ababa,Ethiopia.
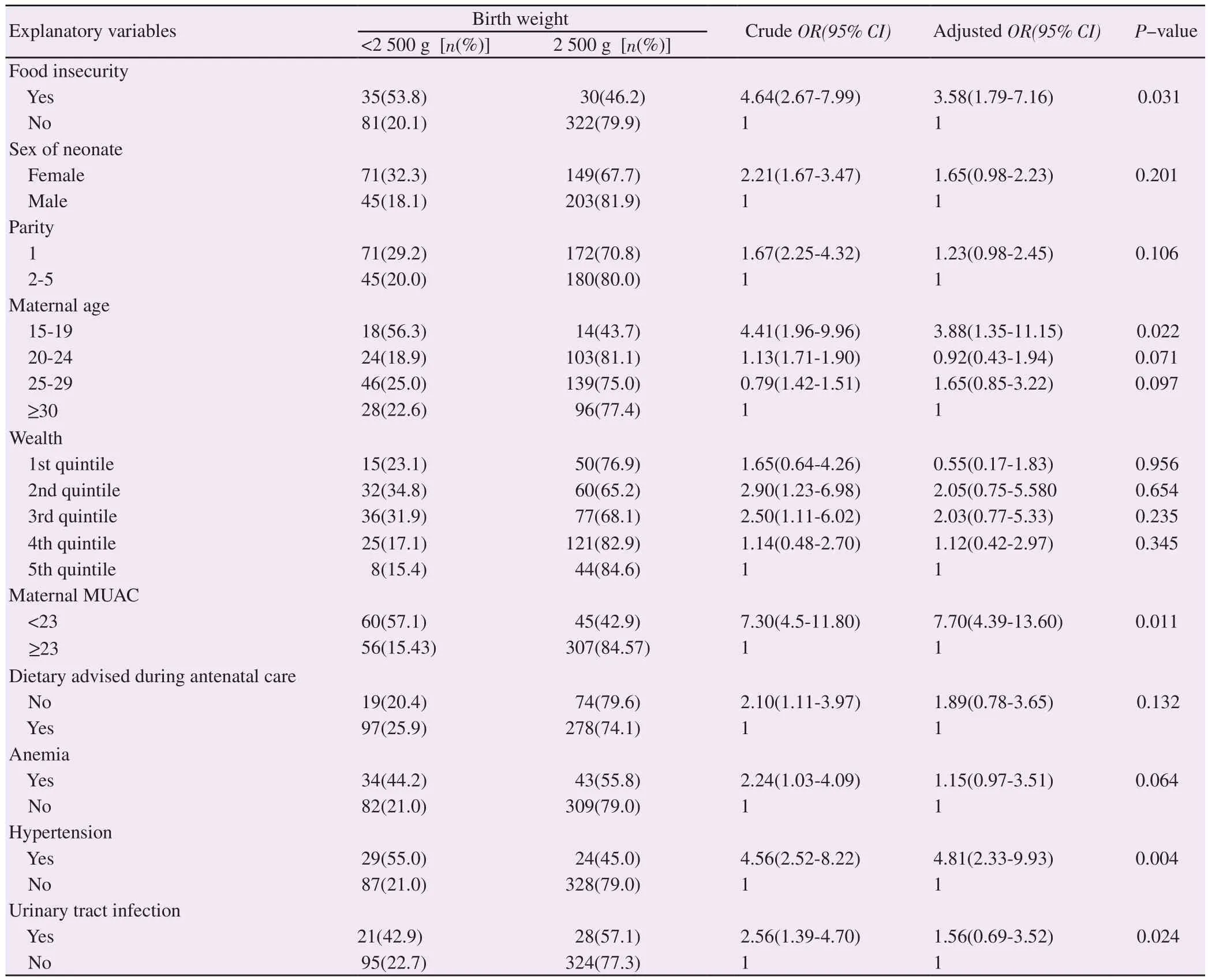
Table 3.Multivariate logistic regression result by covariates of low birth weight among mothers in selected hospitals, Addis Ababa, Ethiopia from February 1, 2017 to May 15, 2017.
3.5.Independent factors associated with low birth weight
Ten variables had association with both the outcome variable (low birth weight) and the major independent variable (food insecurity).These factors were taken to multivariate logistic regression models from binary logistic regression model because one variable(occupation of mothers) was dropped from model due to multicollinearity.After dropping this variable, the variance inflation factors of the remaining variables was from 1.09-2.57 and tolerance test below one.Both of these values were within normal range.Based on aforementioned criteria, those variables included for multiple analysis were socioeconomic related variable (maternal age, sex of neonate, wealth and food insecurity), obstetric and antenatal care related (parity, dietary advised during antenatal care and MUAC) and medical problem during pregnancy (hypertension,anemia and urinary tract infection).Multivariate logistic regression result revealed that factors independently associated with low birth weight were food insecurity, age, hypertension, and MUAC (Table 3).
4.Discussion
The main aim of this study was to assess the association between household food insecurity and low birth weight by using unmatched case control study among term neonate.On the basis of this study,household food insecurity was independently associated with low birth weight.The effect of food insecurity at household level was prominent both at bivariate crude OR 4.64 CI (2.67-7.99) and multivariate adjusted OR 3.6 CI (1.79 -7.16) level of analysis.
The odds of low birth weight among mothers at food insecurity condition were about four times higher than mothers in food security condition.This may be due to the mothers at the time of their pregnancy do not get adequate nutrients which are essential for the growth and development of fetus especially during the second and third trimester.Food insecurity may also pose a stress on pregnant mothers which in turn affect the health of fetus.The cohort study done in United States indicated that food insecurity was significantly associated with a low-birth-weight after adjustment for maternal age which was in line with our study[15].A similar case control study done in Tehran supports the present finding.It indicated that the risk of low-birth-weight babies born to mothers with food insecurity was 10.46 higher against mothers were food security situation(P<0.001)[16].But a cross sectional study done in New York City showed that there was no significant association between household food insecurity and low birth weight.The discrepancy of the results may be due to the difference in design and period of studies.
Maternal MUAC was other independent variable which was strongly associated with low birth weight as proxy indicator of nutritional status of mother.The multivariate analysis finding indicated that mothers who had MUAC < 23 cm was about 8 times more likely to give low birth weight baby as compared to their counterparts with corresponding CI (4.39-13.60).Other studies also reported a similar finding[8,9].MUAC was found to be a good anthropometric indicator to identify acutely malnourished pregnant woman and predict adverse birth outcome[17].
Hypertension was the medical problem that showed a significant association with low birth weight with adjusted OR of 4.8 with CI (2.33- 9.93).The odd of low birth weight among mothers with history of hypertension were about five times higher as compared with mothers who had not history of hypertension during their pregnancy.Other study also support that hypertension was an independent determinant of low birth weight[18].Hypertension during pregnancy leads to a decrement of blood flow through spiral artery which may result in a reduction of passage of nutrient and oxygen to placenta thereby bring about small size infants.The other medical problem such as urinary tract infection and anemia was not significantly associated with low birth weight in this study.
The current study also showed that mother within the age group 15-19 years was about 4 times more likely to give birth with low weight adjusted OR 3.88 CI (1.35-11.15) against mother in age 30 years and above.Different studies supported the result.They indicated that birth weight was generally less favorable among adolescent and women over 35 years old[19,20].Within the age range of 15-19 years,the mothers overall body do not well matured and consequently it may have effect on birth outcome.Intervention aim at delaying pregnancy in young adolescent might be more effective than other modifiable risk factors of low birth weight.Socio-economic variables included in this study were not independently associated with low birth weight.This might be due to mothers included in the study have almost similar living standard.Majority of mothers were housewife,married and lived in similar setting.Other study also support that socio-economic variables (residence, marital status, occupation of mother, educational level and family size of the household) were not significantly associated with low birth weight[21,22].
Using clear selection criteria for both cases and controls decreases selection bias during sample size selection.And also almost the entire question included in this study was close ended.This may decrease information bias.The ratio of case to control may increase the strength of the study as increasing sample size makes the result more precise.Conducting pretest and using standardized and validated questionnaire added value on the strength of this study.On the other hand, this study did not include some potential risk factor of low birth weight.Even if standardized and validated measurement tool was used to measure food security condition of the mothers,misclassification bias may be occurred.This is because the data gathered was based on the response of the participants.
We have shown that household food insecurity was independently associated with low birth weight among term neonates in governmental hospitals in Addis Ababa.This prevents many women from meeting guideline for healthy eating during pregnancy.This finding suggests pregnant mother having food insecurity as a primary focus of intervention in order to prevent low birth weight.In addition, maternal MUAC, hypertension and age were other factors that were significantly associated with low birth weight in this study.So, mothers should be screened for food insecurity during pregnancy.Early initiation of antenatal care and early screening for co-morbidity during pregnancy, early treatment and referral linkage should be assured.Efforts must be continued to provide adequate funding for those in need.Empowering and training health providers should be initiated to give effective nutritional education for mothers during pregnancy.
Conflict of interest statement
The authors declare that there is no conflict of interest.
 Asian Pacific Journal of Reproduction2020年4期
Asian Pacific Journal of Reproduction2020年4期
- Asian Pacific Journal of Reproduction的其它文章
- Prospects of diagnostic and prognostic biomarkers of pyometra in canine
- Hemodynamic changes in arterial flow velocities throughout the first six months of pregnancy in buffalo heifers by Doppler ultrasonography
- Seasonal changes in sperm parameters, testicular histology and circulating levels of reproductive hormones in the male African straw-colored fruit bat (Eidolon helvum)
- Genistein improves the vaginal epithelium thickness in a rat model of vaginal atrophy through modulation of hormone and heat shock protein 70 levels
- Process of becoming a mother in women receiving donated egg: Based on the grounded theory
- Effects of nitric oxide on reproductive organs and related physiological processes
