Potential of the ellagic acid-derived gut microbiota metabolite - Urolithin A in gastrointestinal protection
Małgorzata Kujawska, Jadwiga Jodynis-Liebert
Abstract
Key words: Urolithin A; Colonic metabolite; Gut microbiota; Colorectal cancer;Inflammatory bowel diseases; Hepatocellular carcinoma; Pancreatic ductal adenocarcinoma; Barrett’s esophagus; Ellagitannins
INTRODUCTION
The human gastrointestinal tract (GI) is colonized by a large number of microbes,which is ten times higher than the total number of human cells[1]. The intestinal microbiota, being an integral part of the host system, has emerged as a key modulator of health and disease risk. Indeed, microbes that reside in the human gut form a cometabolism structure with the host to participate in various metabolic processes,including biotransformation of food substances[2]. There is increasing evidence of the involvement of gut microbiota on the health-beneficial effects of food[3]. Given this,microbial metabolites have recently been profoundly studied in phytopharmacology as potential sources of novel therapeutics. It has been demonstrated that phytochemicals, which are poorly absorbed in the intestine, undergo microbiota mediated biotransformation there, such as ring cleavage, demethylation,dihydroxylation, deglycosylation,etc. The generated metabolites can be absorbed and distributed into various tissues, which often correlates with lowered disease risk[4].Ellagitannins (ETs), a class of hydrolyzable tannins found mainly in pomegranate,berries and nuts, are hydrolyzed spontaneously into ellagic acid (EA) during digestion in the upper GI tract. EA can be transformed by the gut microbiota to urolithins D, C, A and B in the intestine and then transported into blood circulation through intestinal epithelial cells as their lipophilicity increases[5-7]. Absorbed urolithins, which reach micromolar concentrations in the bloodstream, undergo phase I and II metabolism including methylation, glucuronidation, and sulfation[8,9]. The presence of urolithins, including urolithins A, in peripheral plasma and their glucuronides and methyl glucuronides in bile after the administration of ETs to pigs,confirms a very active enterohepatic circulation[10]. A regular intake of ET-rich food has been reported to enable the achievement of physiologically relevant concentrations of urolithins and their phase II derivatives in plasma. However, it has been found that their concentration in plasma after consumption of dietary precursors varies considerably between individuals[8,9]. In addition, significant differences among subjects in the ability to produce the final urolithins and the health benefits associated with consumption of ET-containing food products have been reported due to the various compositions of their gut microbiota[11]. In respect to the microbial metabolism, individuals are stratified into three urolithin metabotypes: metabotype A- individuals producing only urolithin A (UA, 25%-80% of the volunteers),metabotype B, yielding isourolithin A and/or urolithin B in addition to UA (10%-50%), and metabotype 0, which is not able to produce any urolithin (5%-25%).Remarkably, metabotype B has been reported to be associated with gut microbial dysbiosis and colorectal cancer (CRC) in patients (reviewed in[12]). Three urolithinproducing bacteria from the human gut belonging to thegenus Gordonibacter(G.pamelaeaeandG. urolithinfaciens) andEllagibacter isourolithinifacienshave been identified to correlate with metabotype A positively[13]. Recently, Gayaet al[14]have reported that alsoBifidobacterium pseudocatenulatumstrain can produce UA.
UA (3,8-dihydroxy-dibenzopyranone), including its glucuronide derivative, has been found to be the predominant isoform of urolithins found in the plasma and urine following the consumption of ETs (reviewed in[8]). It has been demonstrated that this metabolite is also accumulated in organs. The presence of UA in rodent colon,intestinal, prostate and even brain tissues has been reported, whereas UA glucuronide was primarily detected in liver and kidney tissues[7,15,16]. UA has been demonstrated both inin vitroandin vivoexperiments to possess a broad spectrum of bioactivities,including antioxidative, anti-inflammatory, antiproliferative and apoptosis-inducing that might contribute to potential cancer chemoprotection (reviewed in[3]). Since bioavailability of urolithins and their anti-inflammatory, antioxidant and antiproliferative properties are higher relative to parent compounds, the biological activity of EA and ETs including their chemopreventive and chemotherapeutic effects,have been suggested to be mediated by these metabolites[9].
The purpose of this review is to gather evidence fromin vitro,in vivoand clinical studies showing the potential of UA in GI protection alongside suggested mechanisms by which UA can protect against cancer and inflammatory diseases of the digestive tract.
INTESTINE
Given the location of UA generation, it can be expected that UA exerts its effects within the intestinal tract and intestinal walls. This may include inhibitory effects on CRC and suppressive effects on inflammatory bowel diseases (IBDs)[17]. Results of human and animal studies and an experiment performed in the combined SHIME/Caco-2 cell system have indicated that UA can occur along the GI tract, from the duodenum to the rectum, upon long-term ETs consumption due to enterohepatic circulation[10,18]. Moreover, free availability of UA in inflammatory microenvironmental sites due to tissue deconjugation, especially within the intestinal tract,demonstrated in a systemic inflammation rat model, supports its beneficial effects on IBDs or in colon cancers[19]. Based on these findings, it is likely that UA provides significant protection against common intestinal pathologies.
CRC
Numerous studies have given evidence of the beneficial effects of this metabolite against CRC, which is the third most commonly diagnosed malignancy and the second leading cause of cancer death worldwide[20]. Most of these reports documenting chemopreventive effects are based onin vitrostudies. UA has been demonstrated to cause a dose-dependent[21-24], a time-dependent[25,26]and both a concentration- and time-dependent proliferation decrease of CRC cell lines[27,28].Moreover, it has been revealed that a mixture containing mostly UA (85%) and its precursors - urolithin C and EA, at concentrations detected in colon tissues of individuals with metabotype A following the intake of ET-rich food, exerted inhibitory activity against colon cancer stem cells (CSCs), which are considered to be involved in the control of cancer metastasis and the acquisition of chemotherapy resistance[29]. The inhibition of cell proliferation was accompanied by cell cycle arrest in the G2/M and S stages[26-28], and in the G2/M phase[21-23]followed by induction of apoptosis[21-23,26]. Since the delay in the G2/M transition has been reported to be a hallmark of topoisomerase II inhibition[30], potent catalytic inhibition of this human enzyme by UA could be suggested. However, competition tests performed for submicromolar concentrations did not confirm this property of UA, which was inactive up to 5 μmol/L[31]. Several reports indicate that UA-induced apoptosis is associated with increased caspases activity[22,23]. More recent evidence[28]showing a dose-dependent anti-clonogenic effect of long-term exposure to UA in CRC cell lines,indicates that a decrease in the colony formation is exerted through the senescence inductionviathe p53/p21 pathway, rather than by cell cycle arrest or apoptosis,which required much higher concentrations[28]. These data are consistent with previous results[32], also suggesting that the antiproliferative effect of long-term exposure to UA in a colon cancer cell line was mediated through the p53/p21-dependent senescence-like growth arrest. This action was synergistic with the standard chemotherapeutic drug oxaliplatin[32]. González-Sarríaset al[33]have also demonstrated that UA at concentrations achievable in the human colorectum, can potentiate the anticancer effects of 5-fluorouracil (5-FU) on human colon cancer cells.Interestingly, unchanged tannins such as proanthocyanidins extracted from grape seeds, have also been demonstrated to exert anti-tumorigenic effects on colon cancer cells through inhibition of cellular proliferation[34,35], induction of apoptosis and cell cycle arrest, inhibition of the formation of spheroid derived stem-like colon cancer cells[35]as well as by enhancing the impact of 5-FU chemotherapy. However, the activity of PCs has been limited to the proximal jejunum, due to its degradation in the distal region of the small intestine[34]. It has now been suggested that the anticancer effects of UA may also result from autophagy induction since, at concentrations found in the intestine after dietary polyphenols’ consumption, it triggered autophagy, and as a result, inhibited CRC cell growth and metastasis[21]. Kojadinovicet al[36]have demonstrated that both long- and short-term exposure of colorectal adenocarcinoma Caco-2 cells to a mixture of UA and UB, at concentrations reached in the lumen of the gut, contributed to the reduction of oxidative stress, thus preventing the damage caused by reactive oxygen species. The colon cancer chemopreventive property of UA has been supported through the inhibition of CYP1 enzymes involved in the metabolic activation of dietary carcinogens[23,37]. On the other hand, González-Sarríaset al[25]have revealed the induction ofCYP1A1gene expression and activity in the Caco-2 cells after exposure to UA, suggesting that this could reflect the mobilization of detoxification mechanisms. TheCYP1A1induction was accompanied by increased mRNA expression of an enzyme catalyzing the glucuronidation reaction, which is generally considered to facilitate detoxification of potential colon carcinogens[25].
Although there are numerousin vitrostudies supporting UA as a CRC chemopreventive agent, there is a lack of clinical evidence in this area. The only study by Nuñez-Sánchezet al[38]has revealed that the consumption of an ET-containing pomegranate extract counterbalanced the expression of several CRC-related genes in cancerous colon tissues; however, this effect was not associated with the UA level in these tissues.
Data on the chemopreventive activities of UA against CRC are presented in Table 1.
IBDs
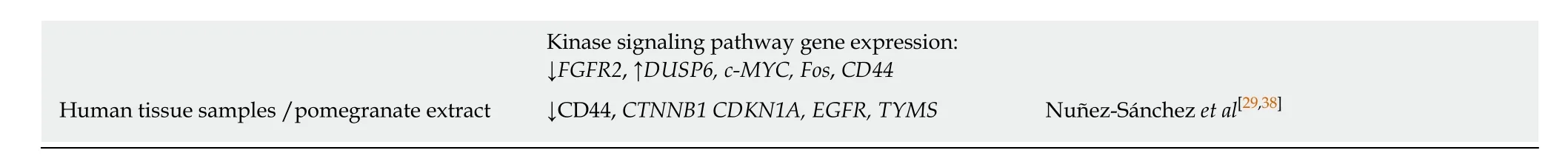
Chronic inflammation is regarded to be involved in approximately 20% of all human cancers. The tight link between long-standing inflammation of the GI tract and carcinogenesis is most apparent in CRC. IBDs, and particularly ulcerative colitis, are thought to be at increased risk for CRC. It is supported by the results of epidemiological studies indicating that IBDs and CRC have a similar prevalence worldwide[39]. The anti-inflammatory effects of UA, which has been demonstrated in lipopolysaccharide (LPS)-induced inflammation in RAW 264.7 murine macrophages[40], may be especially relevant in the intestine, where it can reach considerable micromolar concentrations through a diet rich in ETs. Giménez-Bastidaet al[41]have demonstrated that UA can contribute to the prevention of intestinal inflammations also in colon fibroblasts - cells playing a pivotal role in the inflammatory response sincethe increased permeability of the tight junctions then allows for direct contact of luminal content with the cells resident in the lamina propria. UA at a concentration that is achieved in the colon through the diet has been found to inhibit two critical processes of the intestinal inflammatory response:fibroblast migration and monocyte adhesion that was accompanied by the downregulated expression of their modulatory factors. The reduction of the colon fibroblast migration, mediated by UA, might protect against excessive fibrosis as mechanisms controlling wound healing become disordered in IBDs. Overall, UA contributed to the prevention against the detrimental effect of inflammation on the cells’ viability, which was slightly improved following exposure to the metabolite[41].In a dextran sodium sulfate (DSS)-induced colitis rat model, pre- and co-treatment with UA attenuated the severity of colon injury as preserved mucosal architecture and a decreased epithelium loss have been observed, which was accompanied with improved hematological parameters. The effects were due to the attenuation of inflammatory signaling and the upregulation of the tumor suppressor genes[42]. Of note, procyanidins have been reported to decrease the severity of selected markers of DSS-induced colitis; however, only in the distal ileum and proximal colon. The declined bioactivity of procyanidins in the large bowel has been suggested to be due to their degradation by endogenous microflora[43]. In addition, UA has been shown to modulate the gut microbiota composition favorably in DSS-treated rats, and the authors of the experiment have suggested the prevention of dysbiosis as an additional protective mechanism of UA against intestinal inflammatory diseases[42]. The importance of functional dynamics of gut microbiota and their metabolites has recently become the object of studies, including those concerning intestine health[41,44,45]. The black raspberries diet is also a source of UA that has been demonstrated in mice to impact colon mucosal microbial composition with a robust effect in the luminal microflora[44]. In addition urolithins at concentrations achievable in the gut through the diet, including UA, have been suggested to exert inhibitory effects against intestinal pathogens[46]. Besides its anti-inflammatory activity, UA has been reported to improve gut health by enhancing barrier function[45]. This ETsderived microbial metabolite has been demonstrated to enhance the expression of tight junction proteins such as claudins, Zona occluding-1, and occludin that are critical for epithelial cell barrier functions and to inhibit inflammation both in cell lines and in mice. These effects were a result of activating the phase I (AhR-Cyp1A1)and phase II (Nrf2-antioxidative pathways) metabolic pathways. In mice, oral treatment with UA significantly mitigated systemic inflammation and colitis supporting its important role in the regulation of barrier function[45]. Mukuet al[47]have demonstrated that UA was able to attenuate chemically induced stimulation of CYP1A1 mRNA levels in Caco-2 cells, that was accompanied by inhibition of mRNA levels, both basal and cytokine-induced interleukin 6 and prostaglandinendoperoxide synthase 2 in the human Caco-2 cell line. These effects, at least in part,were due to competitive binding with an aryl hydrocarbon receptor (AhR) since AhR knockdown by siRNA prevented the UA repression of the transcriptional activity regarding both CYP1A1 and inflammatory mediators. As an AhR antagonist, UA failed to induce AhR retention in the nucleus[47]. However, the authors have pointed towards the risks of uninterrupted excessive AhR activation caused by inflammatorysignaling such as Toll-like receptor activation or cytokine release in the tumor microenvironment. Thus, antagonizing AhR by UA has been found to be beneficial to maintain balanced AhR activity for overall homeostasis and to prevent pathological conditions correlating with elevated AhR activity such as cancer[47]. Data on the antiinflammatory activity of UA relevant to the intestine are presented in Table 2.
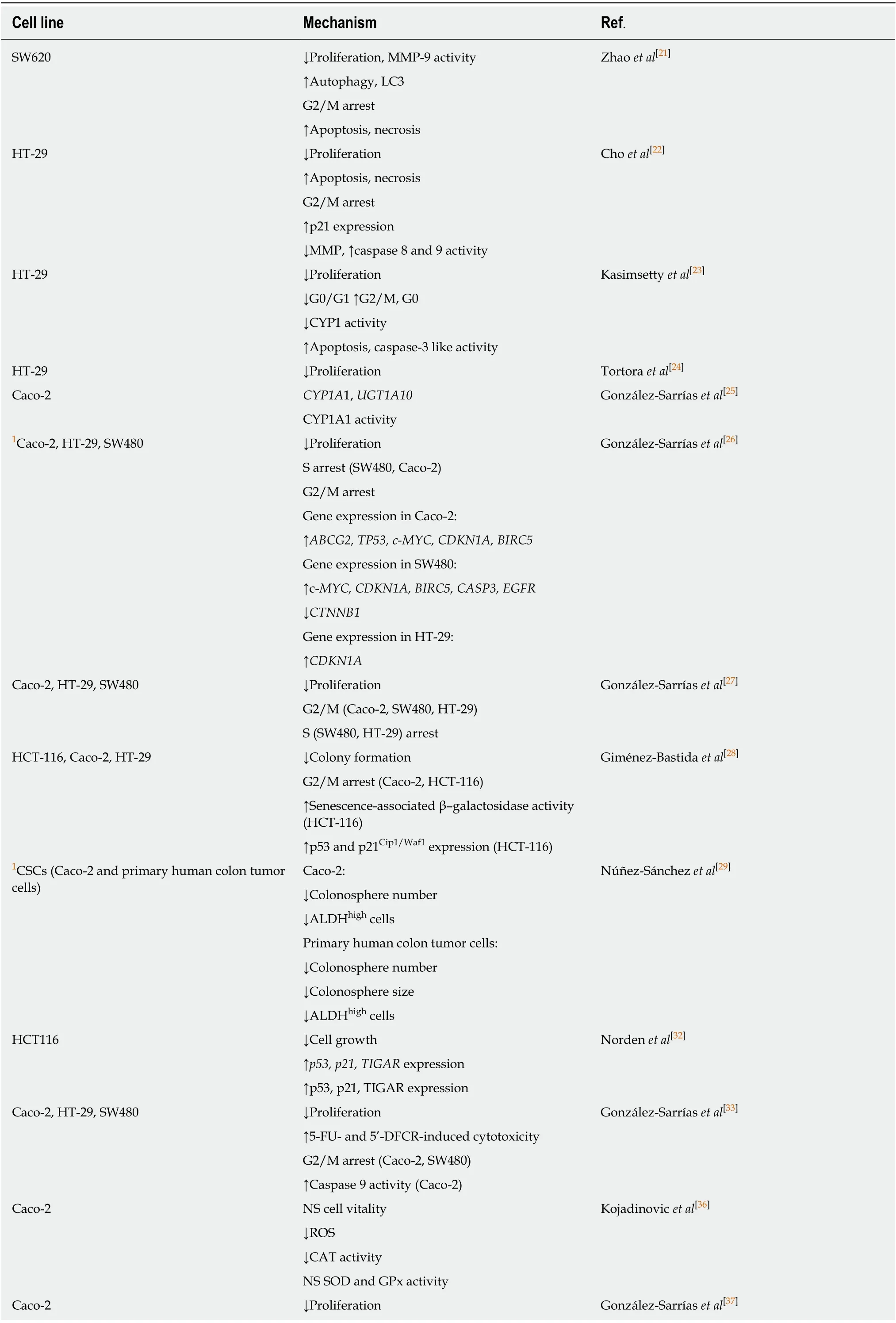
Table 1 Chemopreventive activities of urolithin A against colorectal cancer
1mixture containing urolithin A. 5-DFCR: 5-deoxy-5-fluorocytidine; 5′DFUR: 5-deoxy-5-fluorouridine; ALDH: Aldehyde dehydrogenase; CAT: Catalase;CYP450: Cytochrome P450; GPx: Glutathione peroxidase; LC3: GFP-microtubule-associated protein 1 light chain 3; MMP-9: Matrix metalloproteinase-9;NS: Non significant change; ROS: Reactive oxygen species; SOD: Superoxide dismutase; TIGAR: TP53 induced glycolysis regulatory phosphatase.
LIVER
According to the “World Cancer Report 2014”[48]published by the International Agency for Research on Cancer, liver cancer is the second largest cause of cancer death. The most common primary liver malignancy is hepatocellular carcinoma(HCC) which develops under the influence of chronic inflammation and oxidative stress[49]. Given the antioxidant, anti-inflammatory and antiproliferative activity of UA and its active enterohepatic circulation the chemopreventive potential of UA has also been studied with regard to hepatoprotection. In hepatic carcinoma cell lines,physiologically achievable micromolar concentrations of UA were sufficient to inhibit cell proliferation and induce cytotoxicity in a dose-dependent manner[50,51]. UA suppressed cell proliferationviacaspase-3 dependent apoptosis[50,51]accompanied by down-regulation of the Bcl-2/Bax ratio. Moreover, Wang and co-workers[50]have shown that the antiproliferative effect of UA on HepG2 cells was due to the synergistic action of p38-MAPK activation and suppression of Wnt/β-catenin signaling. UA decreased protein expression of β-catenin and its downstream transcriptional factor c-Myc and Cyclin D1 thereby promoting p53 protein expression,which also resulted from a direct induction of p38-MAPK phosphorylation by UA.The capability of UA to affect Wnt signaling was demonstrated previously by Sharmaet al[52], who observed this pathway inhibition with IC50at 9 μg/mL (39 μmol/L) in a human 293T cell line. Given the fact that over 90% of colon cancers are believed to originate from activating mutations in the Wnt pathway[53], this finding by Wanget al[50]has proven the anticancer activity of UA against CRC. Additionally, since inflammatory response plays a crucial role at all stages of tumor development and HCC is an inflammation-driven disease with up to 90% of cases occurring on the background of chronic liver inflammation[54], the anti-inflammatory role of UA in HepG2 cells by blocking the NF-κB signaling pathway and therefore suppressing the release of inflammatory mediators supports its chemopreventive potential against HCC. Furthermore, the anti-inflammatory effect was accompanied by decreased intracellular ROS production and increased level of intracellular SOD and GPx activity[50]. The antioxidant property of UA has been supported by preventing in a dose-dependent manner the oxidative injury and cytotoxicity in cultured rat primary hepatocytes[55].
The leading risk factor for the development of HCC is the hepatitis B virus (HBV)infection. Accumulated evidence attributes the HBV-encoded x protein (HBx) as a multifunctional oncoprotein in the development of HCC. Previous studies have demonstrated that HBx can upregulate the proteins of the Lin28 family, known inhibitors of let-7a, classified as tumor-suppressor miRNAs[56,57]. Qiuet al[51]have revealed the capacity of UA to act against HBx relevant cell proliferation and invasionviaregulation of the Lin28a/let-7a axis. In this study, UA also inhibited the expression of let-7a downstream targets, such as the high mobility group AT-hook 2 and K-ras,through regulation of the epithelial-to-mesenchymal transition occurring in the initiation of invasion and metastasis of tumor progression[51].
OTHERS
The capability of UA to target kinases downstream of KRAS, in particular, the PI3K/AKT/mTOR signaling pathways, has been demonstrated to be a promising therapeutic approach in pancreatic ductal adenocarcinoma (PDAC) treatment. UA treatment has inhibited human PDAC cell proliferation, migration, and enhancedapoptosis by blocking the phosphorylation of AKT and p70S6Kin vitro. Interestingly,UA only slightly affects pAKT and p70S6K expression in normal epithelial cell lines,thereby suggesting its selective potential against cancer cells. The mechanism of the anticancer action of UA through the inhibition of AKT and p70S6K phosphorylation,reduction of proliferation, and enhancement of cellular apoptosis has been confirmed in both xenograft and transgenic mouse models of pancreatic cancer. Additionally,UA treatment has reprogrammed the tumor microenvironment, as evidenced by reduced levels of infiltrating immunosuppressive cell populations such as myeloidderived suppressor cells, tumor-associated macrophages, and regulatory T-cells thus inhibiting tumor growth resulting in enhanced survival[58].
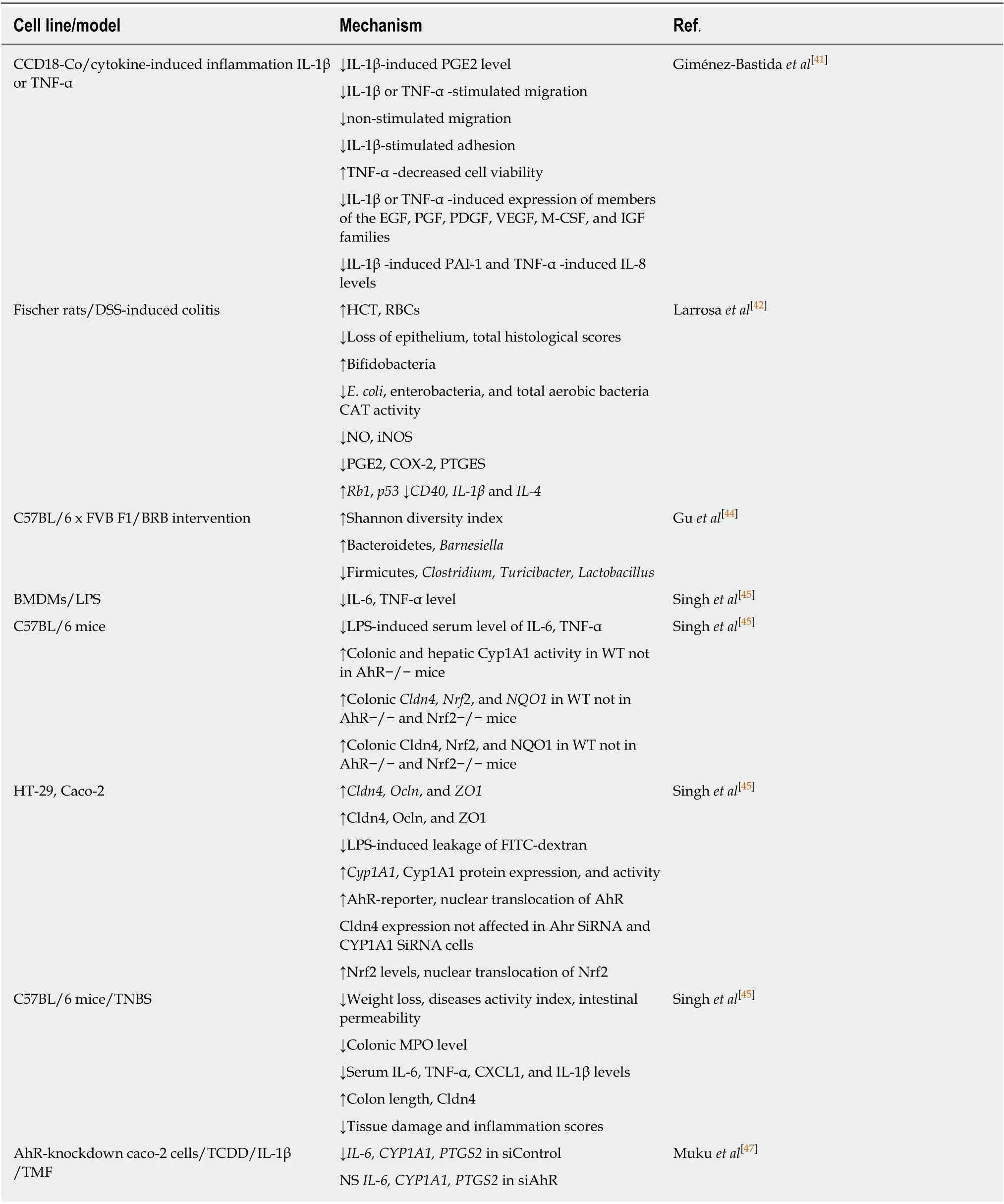
Table 2 Anti-inflammatory activity of urolithin A relevant to the intestine
In Barrett’s esophagus (BE) patients, a 26-wk intervention with lyophilized black raspberries significantly increased GST-pi, a marker of detoxification, in BE epithelium, with over 50% of subjects responding favorably. The presence of UAglucuronide and sulfate in the urine of the BE patients may support the involvement of UA in the observed beneficial effect on BE epithelium[59]. Data on the chemopreventive activities of UA against the above mentioned other cancers of the alimentary tract are presented in Table 3.
CONCLUSION
The above reviewed studies have revealed the multidirectional role of the gut bacterial metabolite UA in the regulation of multiple tumor and inflammatory signaling pathways and the modulation of enzyme activity, including those involved in carcinogen biotransformation and antioxidant defense. These mechanisms have been demonstrated to contribute to the alleviation of inflammation and counteraction of the growth of cancer cells in various structures and organs of GI. Based on the above, UA can be considered as a potential candidate to use as an anti-cancer or antiinflammatory agent in treatment interventions related to GI ailments. Since UA concentrations in human serum and tissues depend on their gut microbial composition, the direct supplementation of UA would overcome the individual variation in microbiota among populations and offer health benefits.
Table 3 Chemopreventive activities of urolithin A against other cancers of the alimentary tract
 World Journal of Gastroenterology2020年23期
World Journal of Gastroenterology2020年23期
- World Journal of Gastroenterology的其它文章
- Liver-directed therapies for liver metastases from neuroendocrine neoplasms: Can laser ablation play any role?
- Endosonographic diagnosis of advanced neoplasia in intraductal papillary mucinous neoplasms
- Medications in type-2 diabetics and their association with liver fibrosis
- Pancreatic necrosis and severity are independent risk factors for pancreatic endocrine insufficiency after acute pancreatitis: A long-term follow-up study
- Impact of a national basic skills in colonoscopy course on trainee performance: An interrupted time series analysis
- Sodium glucose co-transporter 2 inhibition reduces succinate levels in diabetic mice
