How can proton pump inhibitors damage central and peripheral nervous systems?
Proton-pump inhibitors (PPIs) are first line therapy for most gastroesophageal acid-related disorders. They include reflux disorders, Helicobacter pylori infections, Zollinger-Ellison syndrome, and gastroesophageal malignancies. In clinical practice, PPIs have largely replaced histamine-2 receptor antagonists (H2RAs) due to their superior efficacy and are currently widely prescribed and sold worldwide. (Kantor et al.,2015). Since the PPIs are, in addition, freely available without prescription in the United States, there has been a growing concern over proton-pump inhibitor prolonged use and serious side effects such as Alzheimer’s disease (AD) type dementia. A few large scale studies have shown an increased risk of the AD type and non-AD type dementia with PPI use,while others have questioned this association (Novotny et al.,2018; Khan et al., 2020). Aside from the memory impairment related adverse events, PPI use has been reported to be associated with neuropathies in a few case reports (Rajabally and Jacob, 2005). We investigated these associations by analyzing of postmarketing adverse event (AE) reports for patients on PPI (n= 42,537) and H2RA (n= 8309) monotherapy in United States Food and Drug Administration Adverse Event Reporting System datasets. Initially, every report where a PPI or an H2RA was used were selected into the antacid cohort. The data set was further split into PPI and H2RA arms.Reports where a PPI or an H2RA was the only medication used were selected into their respective cohorts, excluding all concurrent medications and comorbidities. Adverse event report rates were analyzed via odds ratio analysis and 95%confidence intervals. We found a significantly increased risk of memory impairment, including both AD- and non-AD type dementia conditions, in PPI-treated patients (odds ratio 3.28, 95% confidence interval [2.31, 4.67]) (Makunts et al., 2019a). Additionally, we found that virtually every neurologic disease state related adverse event had a significantly higher reporting frequency and increased risk in the PPI monotherapy cohort: hearing impairment (11.64 [5.20,26.11]), visual impairment (1.85 [1.44, 2.37]), neurological/neuropathic impairment (8.68 [3.86, 19.49], seizure related adverse events (1.54 [1.06, 2.24]), and migraines (2.19 [1.29,3.72]) (Makunts et al., 2019a). To the best of our knowledge this was the first large scale study to confirm the previously observed associations of PPI use with a wide range of neurological AEs involving both central and peripheral nervous systems (CNS and PNS).
While the real reason of this problematic association is still unknown, due to a relatively broad pharmacology, PPIs could potentially affect the nervous system through several extracellular factors (metabolite/electrolyte-related) and intracellular-damage-related mechanisms of action affecting cells outside stomach and gastrointestinal tract.
Vitamin B12 and Magnesium vs. PPIs:Extracellular mediators may include cofactors and electrolytes such as Vitamin B12 (a.k.a. cobalamin) and magnesium. Vitamin B12 absorption is pH dependent and its absorption is affected by proton-pump inhibitor induced increase in gastric pH (Leishear et al., 2012). B12 deficiency has been associated with poor sensory and motor nerve function, cognitive and memory impairment, and peripheral neuropathies, possibly through demyelination of nerves and tracts in CNS and PNS (Leishear et al., 2012). It should be noted that although both PPIs and H2RAs affect B12 levels, in our analysis the neurological side effects were significantly higher in the PPI cohorts, possibly due to stronger efficacy in increasing pH levels or additional,non-B12 related, mechanisms.
Another mechanism by which PPI could affect the nervous system is related to hypomagnesemia. This adverse event has been documented in all the PPIs’ Food and Drug Administration package inserts/drug labels. Furthermore, we and our colleagues confirmed this association in an earlier study on PPI use association with renal injury and electrolyte abnormalities (Makunts et al., 2019b). Magnesium plays a major role in CNS functioning though its effect on N-methyl-D-aspartate receptor activity. When deficient it can cause increased calcium influx and cause excitotoxicity, a process which causes neuronal dysfunction and death due to overactivation (Vink and Nechifor, 2011). Magnesium also exhibits neuroprotective effects through regulation of oxidative stress by inhibiting reactive oxygen species production and reducing lipid peroxidation. There is an association of magnesium deficiency with increased plasma Substance P levels, which in turn is associated with neurogenic inflammation (Vink and Nechifor, 2011).
Lysosomal vacuolar-type H+-ATPase (V-ATPase) versus PPIs:A possible direct mechanism of PPIs causing neurological adverse events may involve modulation of ATPase.V-ATPase is an intracellular ATP driven proton pump that acidifies intracellular compartments. It is involved in protein degradation, and tumor metastasis. Only recentlyin vitrostudies demonstrated direct PPI inhibition of V-ATPase by esomeprazole (Song et al., 2017). V-ATPase impairment affects lysosomal function which it turn compromises necessary autophagy and is associated with a wide range of proteinopathy related neurodegenerative diseases including Alzheimer’s dementia (Colacurcio and Nixon, 2016).
Endothelial cell senescence versus PPIs:Outside of the nervous system PPIs have been associated with senescence and aging of endothelial cells. Anin vitrostudy has demonstrated PPI effect on senescence in endothelial tissues through shortening of telomeres, decrease nitric oxide levels, impaired autophagy (Yepuri et al., 2016). These findings, while not yet confirmedin vivo, offer a plausible explanation for peripheral neuropathies which are one of the main manifestations of microvascular damage often seen in diabetic patients.
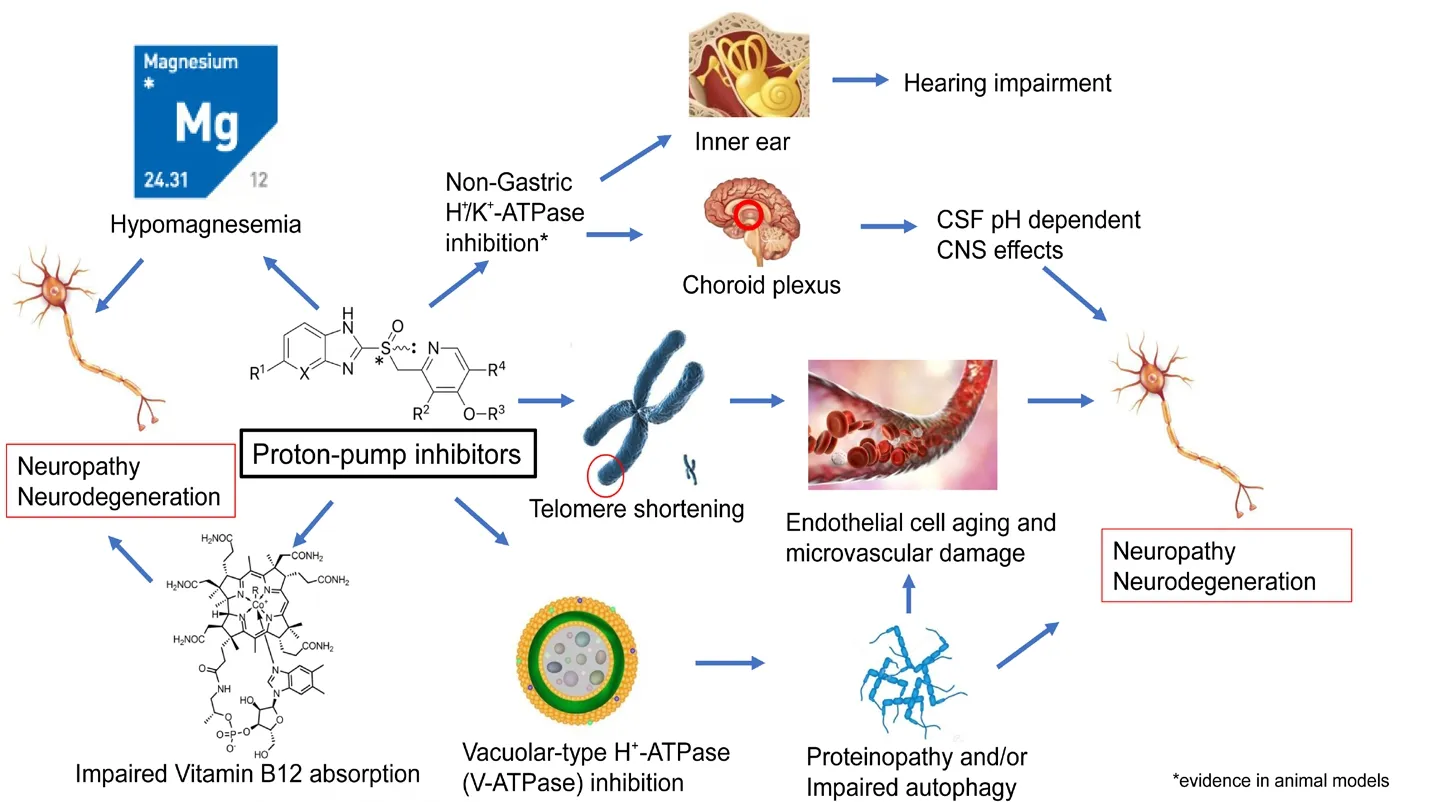
Figure 1 Possible mechanisms of neurological side effects of proton-pump inhibitors.
Non-gastric expression of the main PPI target: H+/K+ATPase:Studies using animal models have demonstrated not-gastric tissue expression in H+/K+ATPase that is the main target of PPIs. Interestingly the highest expression of the hydrogen/potassium pump outside of the gastrointestinal system was found in the choroid plexus and inner ear in rats (Lecain et al., 2000). This finding, if confirmed in experiments on human tissues, could also explain the hearing impairment related and other CNS AEs.
Future directions:Considering the narrow spectrum of therapeutic options available for neurodegenerative disease,it is essential to maximize preventative measures which include responsible prescribing and use of medications that can potentially cause, often irreversible, neuronal degeneration. The possible mechanisms of neurologic adverse effects of PPIs are very broad (Figure 1) and make it challenging to pinpoint any unique mechanism. Furtherin vivostudies are necessary to confirm and quantify the damage and elucidate the molecular mechanisms responsible for these side effects of proton-pump inhibitors.
Tigran Makunts, Ruben Abagyan*
Skaggs School of Pharmacy and Pharmaceutical Sciences,University of California, San Diego, La Jolla, CA, USA
*Correspondence to:Ruben Abagyan, PhD, ruben@ucsd.edu.
orcid:0000-0001-9309-2976 (Ruben Abagyan)
Received:December 19, 2019
Peer review started:December 26, 2019
Accepted:February 26, 2020
Published online:May 11, 2020
doi:10.4103/1673-5374.282252
Copyright license agreement:The Copyright License Agreement has been signed by both authors before publication.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Open peer reviewers:Abdollah Amini, Shahid Beheshti University of Medical Sciences, Iran; Lorenzo Di Cesare Mannelli, University of Firenze, Italy.
Additional file:Open peer review reports 1 and 2.
- 中国神经再生研究(英文版)的其它文章
- The role of the TrkB-T1 receptor in the neurotrophin-4/5 antagonism of brain-derived neurotrophic factor on corticostriatal synaptic transmission
- Could non-invasive brain-stimulation prevent neuronal degeneration upon ion channel re-distribution and ion accumulation after demyelination?
- The role of exercise in brain DNA damage
- Combined effect of repetitive transcranial magnetic stimulation and physical exercise on cortical plasticity
- Should mast cells be considered therapeutic targets in multiple sclerosis?
- Neuroprotection mediated by natural products and their chemical derivatives