Minimally invasive maxillary sinus augmentation with simultaneous implantation on an elderly patient: A case report
Shi-Hui Yang, Wan-Qi Yu, Jing-Jie Zhang, Zhe Zhou, Fan-Rong Meng, Jun-Yan Wang, Rui-Ning Shi, Yan-Min Zhou, Jing-Hui Zhao
Shi-Hui Yang, Wan-Qi Yu, Jing-Jie Zhang, Zhe Zhou, Jun-Yan Wang, Rui-Ning Shi, Yan-Min Zhou,Jing-Hui Zhao, Department of Dental Implantology, School and Hospital of Stomatology, Jilin University, Changchun 130021, Jilin Province, China
Fan-Rong Meng, Department of Stomatology, Aviation General Hospital, Beijing 100000, China
Abstract BACKGROUND In this case study, a minimally invasive transalveolar approach using platelet-rich fibrin and bone substitute with simultaneous implantation was carried out in an elderly patient. We analyzed the cone-beam computed tomography (CBCT)findings to evaluate bone regeneration.CASE SUMMARY A 65-year-old female with no contraindications for dental implants and loss of maxillary bilateral molars is described. Examination by CBCT showed the available vertical bone height in the bilateral posterior maxilla was 0.5-6.8 mm in the left and 2.8-6.5 mm in the right. The patient underwent a transalveolar approach using platelet-rich fibrin and bone substitute with simulataneous placement of an implant 10 mm in length. Six months post-surgery, the implant showed excellent osseointegration with the bone graft. Thereafter, full-ceramic crowns were fitted. Follow-up at 2 years demonstrated satisfactory prognosis.CONCLUSION Platelet-rich fibrin and bone substitute can be used to augment the maxillary sinus with a vertical bone height less than 4 mm.
Key Words: Maxillary sinus augmentation; Bone substitute; Bone regeneration; Plateletrich fibrin; Internal sinus floor elevation; Case report
INTRODUCTION
Insufficient height of the residual bone in the posterior maxilla is commonly encountered after tooth loss in elderly people. Alveolar bone resorption and increased pneumatization of the maxillary sinus results in a decrease in vertical bone height(VBH) of the posterior alveolus in the edentulous areas. Maxillary sinus augmentation is an effective way of resolving inadequate bone height in the posterior region of the maxilla. There are two main approaches to sinus augmentation in preparation for implant placement: Transalveolar and lateral antrostomy[1]. Rosen and colleagues[2]found that the implant survival rate was 85.7% when the VBH was 4 mm or less in the posterior region of the maxilla, which improved to 96% in locations with more than 4 mm of initial bone height. When the residual bone height is less than 5 mm, the lateral antrostomy approach is recommended[3]. However, with continuous developments in implant technology, the indications for the transalveolar approach are expanding, and it is increasingly favored by oral surgeons and patients due to its advantages of simple operation, less trauma, mild postoperative response, and low cost.
CASE PRESENTATION
Chief complaints
A 65-year-old female complained about the loss of maxillary bilateral molars which were extracted 6 mo previously.
History of present illness
Maxillary bilateral molars were extracted 6 mo previously.
History of past illness
The patient had good general health with a history of bruxism.
Physical examination
Oral examination shows that the attached gingiva was normal and the alveolar crest was less plump. There was no obvious elongation of the jaw teeth and prosthesis. #25 used to be an abutment tooth with vital pulp, which was ready for restoration. The rest of her teeth were heavily worn and she had a tight bite. Sufficient space was available for crown implants with an anatomical design (Figure 1B).
Laboratory examinations
No abnormalities were observed following laboratory examinations.
Imaging examinations
Examination by cone-beam computed tomography (CBCT, Figure 1A) showed that the available VBH was 0.5-6.8 mm in the left and 2.8-6.5 mm in the right.
FINAL DIAGNOSIS
The final diagnosis was Kennedy II dentition defect with a VBH less than 4 mm.
TREATMENT
According to the patient’s condition, the treatment plan was performed using the transalveolar approach to the bilateral maxillary posterior area with four Nobel Active implants. The second stage surgery and crown repair were performed 6 mo later.Before surgery, two blood samples were centrifuged at 3000 rpm for 10 min without any anticoagulant to establish platelet-rich fibrin (PRF, Figure 2E). After coagulation,each PRF clot was prepared in membrane form (Figure 2E). In addition, 0.12%chlorhexidine mouthwash was used to rinse the mouth for 3 min/rinse which was repeated 3 times. Local infiltration of Articaine with adrenaline 1:100000 was administered to induce anesthesia. A release incision was performed to make a mucoperiosteum flap in the alveolar crest, then a pilot drill was used to prepare the implant socket leaving an approximately 1 mm gap from the maxillary sinus floor boundary (Figure 2A and B). Next, using a rounded and blunted osteotome to elevate the maxillary sinus membrane, the cortical bone of the sinus floor was up-fractured(Figure 2C and D). After that, the patient’s nose was pinched to check the integrity of the maxillary sinus. The implant, PRF and bone substitutes were simultaneously implanted (Figure 2H-J). The implants were placed (4.3 mm × 10 mm, Nobel Active,Sweden) with a torque of 35 N·cm, overlapped by a cover screw (Figure 2K and 2L).Postoperative CBCT revealed that the implants were located in the appropriate position (Figure 3).
Antibiotics, including cephalosporin and ornidazole, were administered for 3 d postoperatively.
OUTCOME AND FOLLOW-UP
Six months later, direct contact between the bone and implant interface was observed on CBCT images (Figure 4). The cover screws were replaced with healing abutments(Figure 5). Two weeks later, a zirconia ceramic crown was constructed (Figure 6). The whole permanent abutments added torque force of 35 N·cm. At 1 mo after loading, the CBCT scan showed that the gained bone height was stable (Figure 7). The patient was followed-up for 30 mo after the first stage of surgery, with satisfactory stability, and without gingival recession (Figure 8).
DISCUSSION
Tasouliset al[4]reviewed the literature and found that the success rate of the lateral antrostomy approach was 86%-100% while that of the transalveolar approach was 92.8%-97%. There was no significant difference in the long-term clinical effect between the two approaches. The transalveolar approach is more conservative and less invasive than the lateral approach[5]. Adequate VBH is a critical factor to avoid complications such as sinus membrane perforation. However, the VBH did not reduce the success rate of the implants and associated prostheses. Gonzalezet al[6]carried out the crestal approach with simultaneous implantation with VBH of 2-4 mm on the posterior maxillary alveolar. In this case, the elderly patient had bone rarefaction in the maxilla,and was more suitable for lateral antrostomy, but considering the patient's poor tolerance, lateral antrostomy takes longer and is more traumatic, the postoperative trauma would be greater, and recovery would be slower. Therefore, following a discussion with the patient and informed consent for treatment, we chose the crest approach. To ensure the success rate, bone substitutes, and PRF were combined to induce bone regeneration.
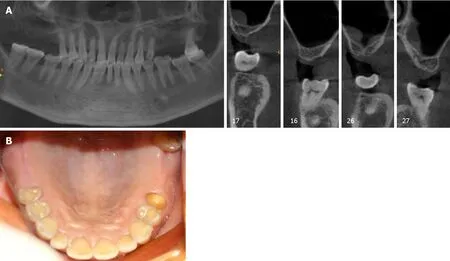
Figure 1 Preoperative cone-beam computed tomography and intraoral photograph. A: Preoperative cone-beam computed tomography; B: Intraoral photograph.
The combination of PRF and bovine bone graft material may be an alternative treatment option to the routinely used combination of bovine bone graft material and collagen membrane. Rodriguezet al[7]believe that the use of platelet-rich plasma in combination with bovine bone is effective for maxillary sinus augmentation with simultaneous insertion of endosseous dental implants in severely resorbed posterior maxillae. In 2001, Choukrounet al[8]developed a simpler method to concentrate platelets and fibrin without blood treatment instead of platelet-rich plasma which is more expensive and difficult to obtain. PRF belongs to the second generation of platelet concentrates, with simplified processing and without biochemical blood handling which contains a strong fibrin matrix and releases cytokines slowly, such as transforming growth factor-beta, vascular endothelial growth factor, and plateletderived growth factor[9]. Also, fibrin is applied as a delivery system for growth factors in tissue engineering[10]. Moreover, fibrin has a significant effect on collagen synthesis in osteoblast-like cells. Thus, both cytokines and the fibrin matrix in PRF are synergistic in terms of cell migration and rapid vascularization, providing a favorable environment for the promotion of proliferation and differentiation of osteoblasts[11]. On the one hand, PRF as a sole filling material could promote natural bone regeneration when implants are placed simultaneously[12]. On the other hand, due to its good intrinsic adherence to the Schneiderian membrane, it is not only used to cover the perforation but is also used preventively to reduce the risk of perforation during the transalveolar approach[13].
Choukrounet al[14]evaluated the effectiveness of freeze-dried bone allograft (FDBA),and an FDBA and PRF mixture in sinus augmentation surgery, and found that the addition of PRF to FDBA accelerated graft maturation and decreased the healing period before implant placement[15,16]. Zhanget al[16]found that compared with PRF mixed with FDBA, the absence of precursor cells was the reason for the lack of effect of PRF mixed with bio-oss on bone formation. Tatulloet al[17]demonstrated that the combination of PRF and bovine bone graft material can promote the early stability of implants, and revealed that marked neoangiogenesis acted as good trophic support for the newly-formed bone tissue.
CONCLUSION
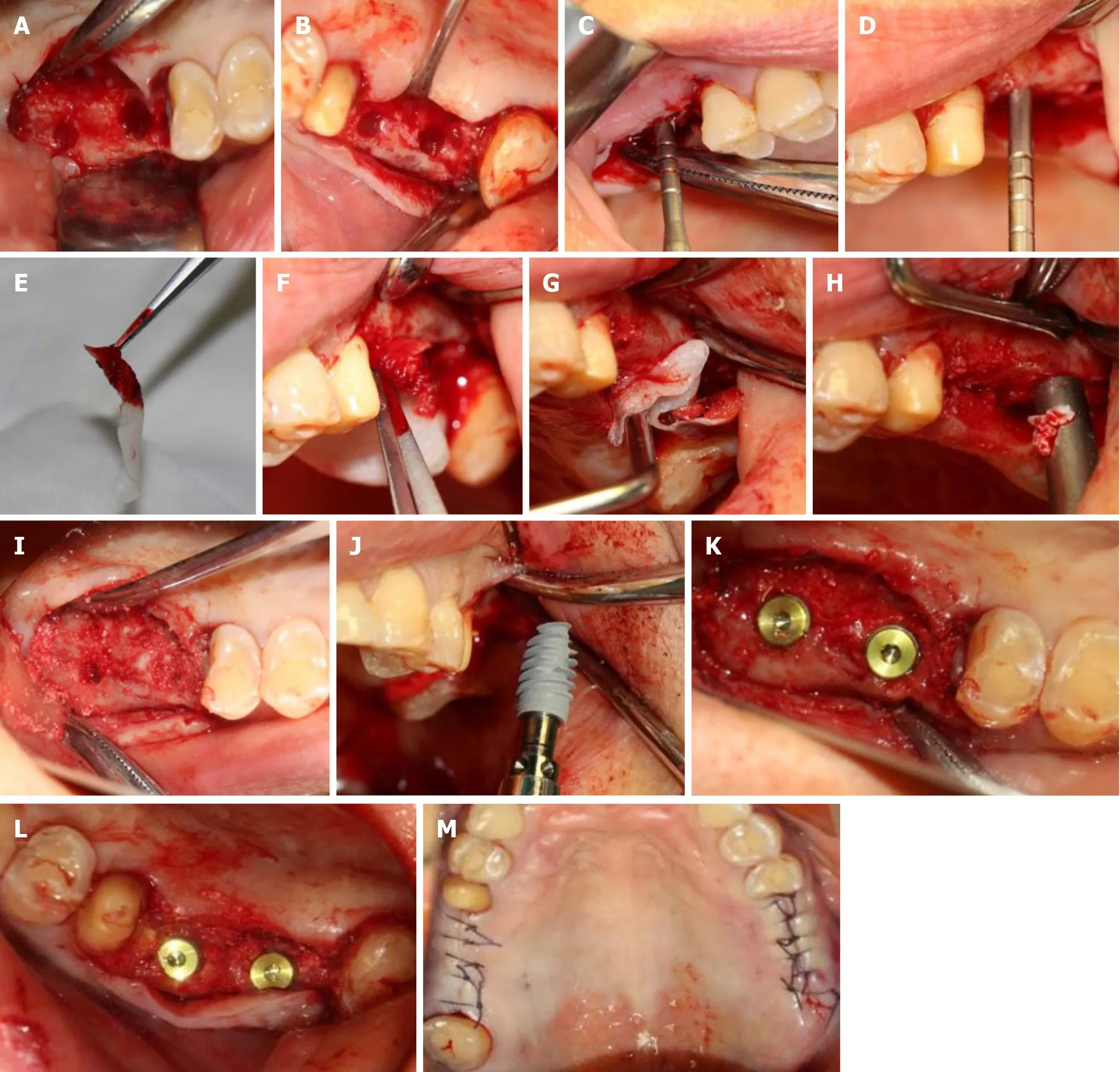
Figure 2 First-stage surgery. A and B: Nest preparation on the right; C and D: Bilateral internal maxillary sinus floor elevation; E: Platelet-rich fibrin (PRF) clots were compressed between sterile dry gauze; F and G: Established PRF membranes were placed in the primary elevated sinus floor; H and I: Implantation of the bovine bone graft material; J: Implant (4.3 mm × 10 mm, Nobel Active, Sweden) was implanted with a torque of 35 N·cm; K and L: Placement of a suitable cover screw; M: Stitches in the wound.
In this case, we placed PRF and bovine bone graft material in the floor of the maxillary sinus using the crest approach, and performed the restoration 6 mo later with the torque force at 35 N·cm. This method promotes early bone healing, and guarantees initial stability of the implant. The results in this case show that minimally invasive implantation and repair in elderly patients can be achieved, with reduced surgical trauma, postoperative pain, swelling, surgical costs and a significantly shorter implantation and repair time. Therefore, in elderly patients, based on the premise of strict mastery of surgical indications and operating skills, this minimally invasive method of simultaneous implantation in the maxillary sinus can be considered.
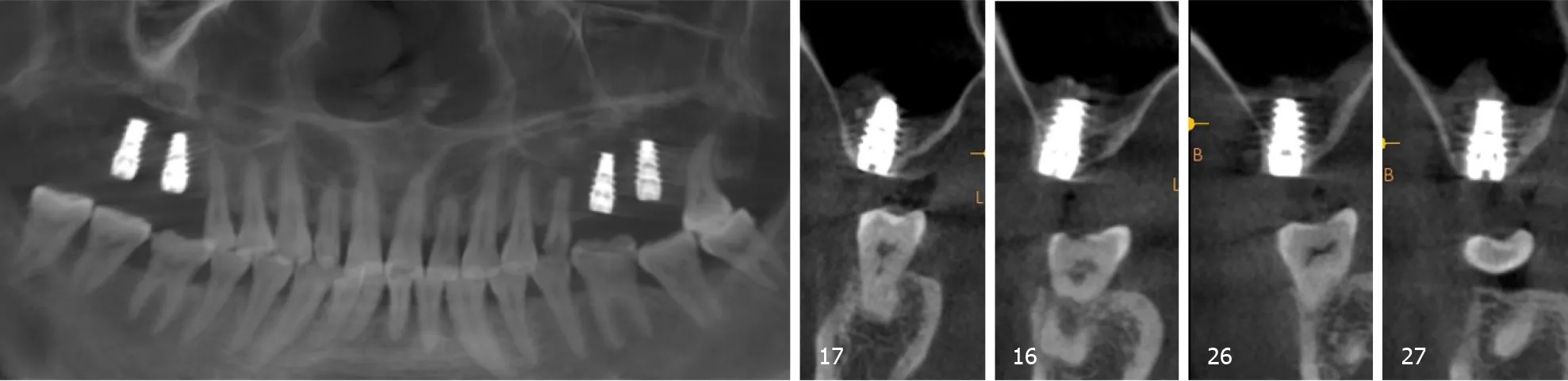
Figure 3 Cone-beam computed tomography after the first-stage surgery.
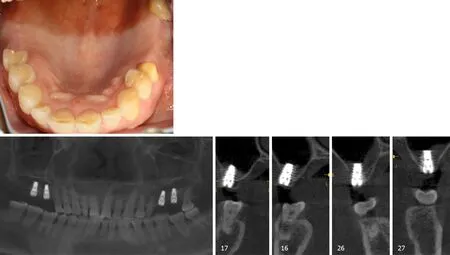
Figure 4 Six months after the first surgery.
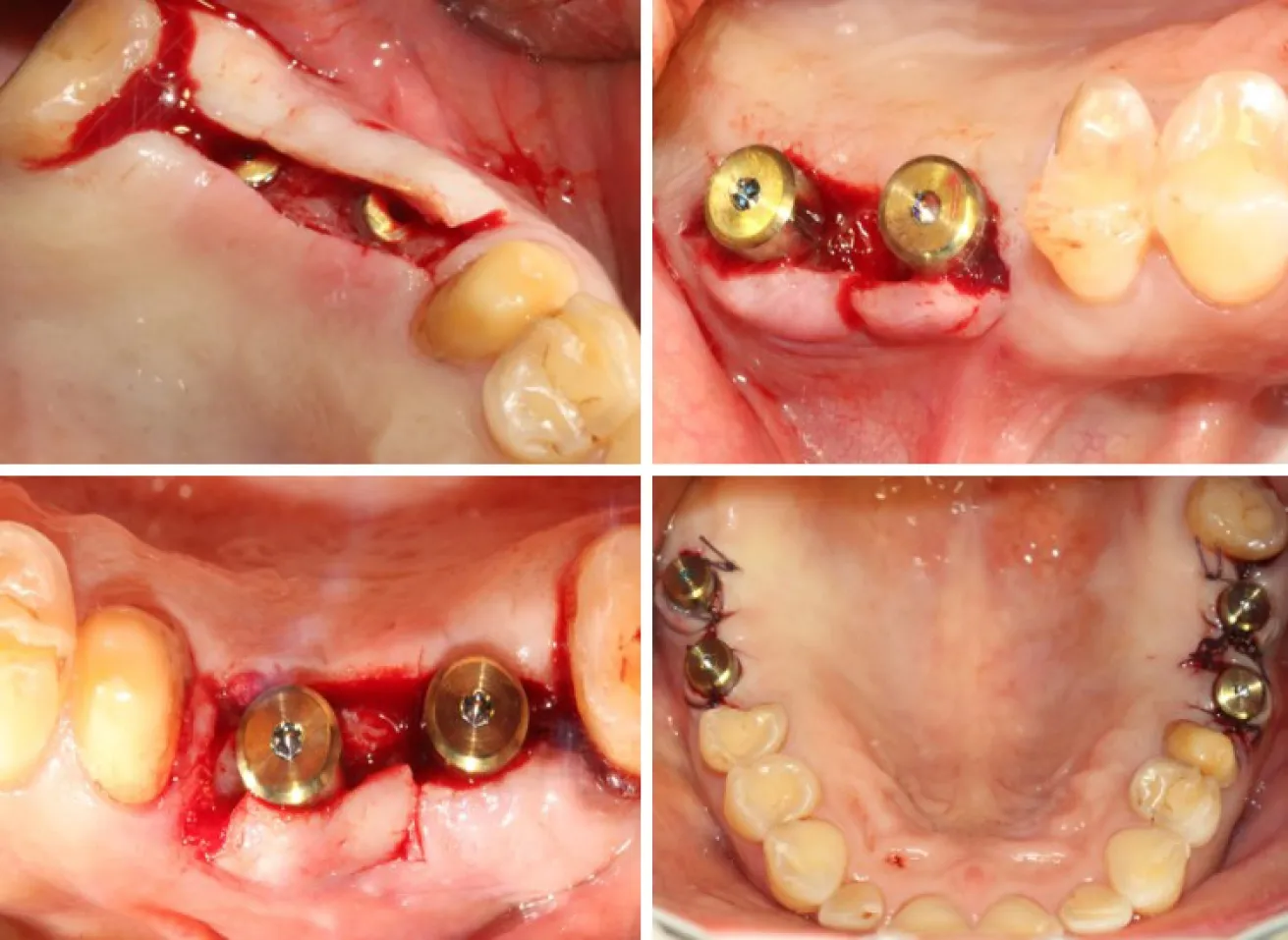
Figure 5 Six months later, the second-stage surgery was performed and the cover screw was replaced with the healing cap.

Figure 6 Zirconia ceramic crowns were constructed. A-D: A painless 35 N·cm torque was added to put the abutment in place; E and F: Zirconium-ceramic crowns; G and H: Buccal view of the final prosthesis in place; I-K: Occlusal view of the final prosthesis in place.

Figure 7 One month after permanent restoration.
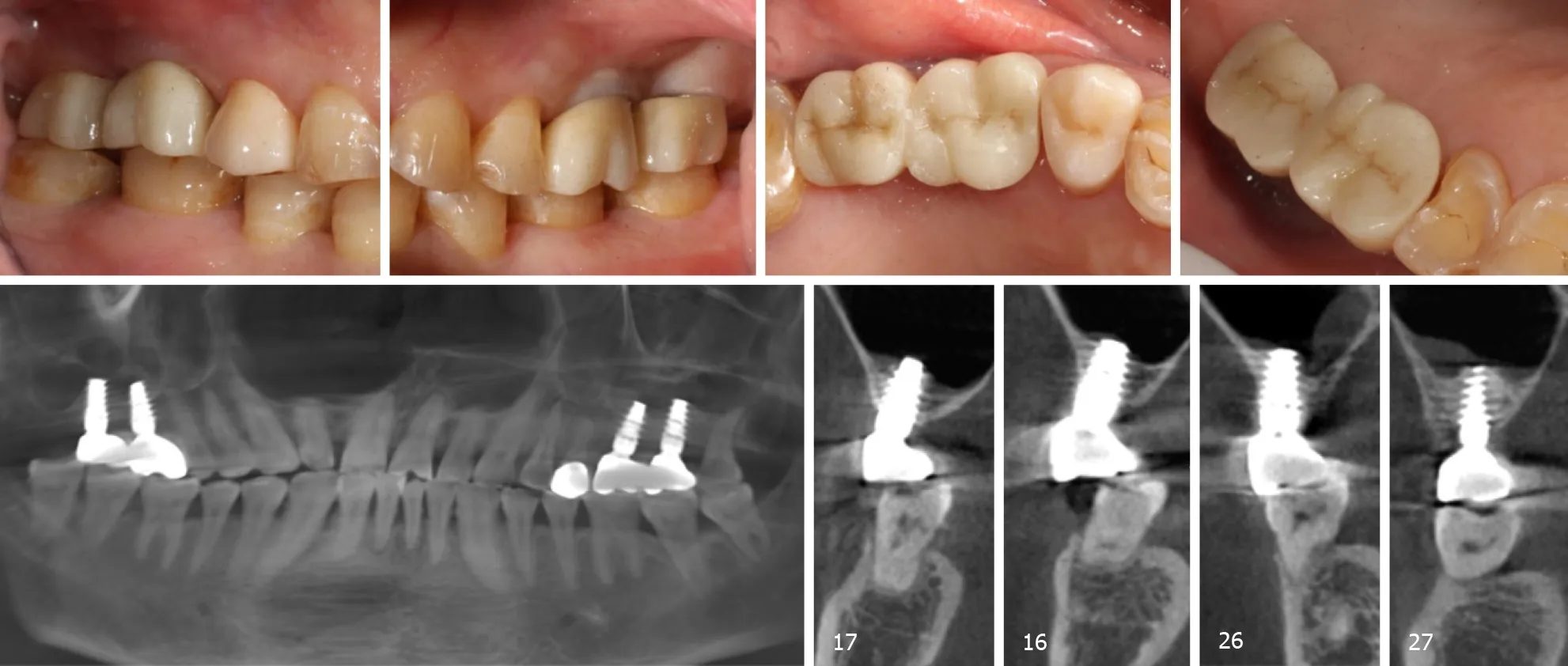
Figure 8 Patient was followed-up for 30 mo after the first stage surgery.
 World Journal of Clinical Cases2020年24期
World Journal of Clinical Cases2020年24期
- World Journal of Clinical Cases的其它文章
- Role of gut microbiome in regulating the effectiveness of metformin in reducing colorectal cancer in type 2 diabetes
- lmpact factors of lymph node retrieval on survival in locally advanced rectal cancer with neoadjuvant therapy
- Three-year follow-up of Coats disease treated with conbercept and 532-nm laser photocoagulation
- Virus load and virus shedding of SARS-CoV-2 and their impact on patient outcomes
- Risk factors for de novo hepatitis B during solid cancer treatment
- Cause analysis and reoperation effect of failure and recurrence after epiblepharon correction in children
