Availability and quality of procedural sedation and analgesia in emergency departments without emergency physicians: A national survey in the Netherlands
Maybritt I. Kuypers, Adinda Klijn, Nieke E. Mullaart-Jansen, Frans B. Plötz
1 Amsterdam University Medical Center, Amsterdam, the Netherlands
2 Emergency Department, Dijklanderziekenhuis, Hoorn, the Netherlands
3 Department of Pediatrics, Tergooi Hospital, Blaricum, the Netherlands
KEY WORDS: Procedural sedation and analgesia; Emergency departments; Emergency physicians
INTRODUCTION
Procedural sedation and analgesia (PSA) is an effective method to treat emergency department (ED) patients who need to undergo painful procedures.[1-4]Research has shown that EDs with emergency physicians have been successful in implementing PSA. The residencytraining program of Emergency Medicine (EM) includes extensive PSA instruction and practice. Accordingly,PSA performance in EDs has markedly increased since emergency physicians and EM residents began staffing EDs.[5-8]Emergency physicians are also the main performers of both paediatric and adult PSA in the ED,when compared to other specialities.[9]
In the Netherlands, 13.8% (13/94) of the EDs are not staffed by emergency physicians. Currently it is unknown who is performing PSA in EDs without emergency physicians, and if it is done according to the national guideline. We suspect EDs without emergency physicians are struggling to implement PSA in their department. By assessing the current situation and evaluating the needs of the health care professionals working in these EDs,we hope to discover what potential solutions could help implement safe PSA practice in these EDs. We designed this nationwide survey to investigate PSA availability and quality, specifically in EDs without emergency physicians.
METHODS
Design
We performed an exploratory cross-sectional study amongst ED nurses and physicians in all EDs without emergency physicians in the Netherlands. Data were gathered using a standardized questionnaire. Our main outcome was availability of PSA in the ED. The secondary outcomes were the rationale provided for the limited availability. Furthermore, we looked at quality in terms of self-assessment on prof iciency and guideline adherence of the respondents who are performing/involved with PSA.
Procedure
All EDs in the Netherlands were assessed for presence of emergency physicians, registered by the Royal Dutch Medical Association (KNMG).The managers of the EDs earmarked as ED without emergency physicians by the Dutch Society for Emergency Physician (NVSHA), were approached for short interviews in the period from September 2017 to January 2018. The purpose of these meetings was to obtain a better understanding of the local organisation of emergency PSA. We asked permission to perform interviews and send questionnaires to the health care professionals who were involved with PSA in the ED.Participation was on a voluntary and anonymous basis.
Study population
The study included all Dutch EDs without registered emergency physicians. We performed a convenience sample amongst ED nurses, residents and consultants who were involved with/performing PSA in the ED.
Variables and measurements
The survey is divided into two general topics.The first part of the survey is focussed on the general organisation and availability of PSA in the ED. The second part is focussed on self-assessment questions regarding performance of PSA and guideline adherence.The providers are asked if they are capable and competent in performing PSA and if they are able to perform advanced life support (ALS)/advanced paediatric life support (APLS) appropriately.
Some of the guideline recommendations are incorporated as questions. For example, adverse event reporting, choice of medication, if PSA-provider performs other tasks simultaneously. Answers to survey items were either indicated on a six-point Likert scale ( 0= completely disagree, 5 = completely agree) or multiple choice).
Data analysis
Data were analysed both qualitatively and quantitatively with SPSS, version 23.0 (IBM Corp,Armonk, NY, 2015). Demographics and survey information are presented as descriptive data.
RESULTS
Participants
We received response from all 13 EDs identified as having no emergency physician staff, out of the total of 94 EDs nationwide. We sent out a total of 432 questionnaires across the different institutions. The response rate was 36.3% (157/432), after correction for incomplete surveys(34.3%, 148/432). The responses came from ED nurses(64.2%), residents (23.0%), consultants (10.1%), and of 2.7% the profession was unknown.
Table 1 shows the survey results on PSA practice in adult versus paediatric patients. First choice sedative medication was midazolam in both groups. For analgesic medication fentanyl was the first choice in adults and paracetamol in paediatric patients. The most frequent indication for PSA, both for adults and paediatric patients, were dislocation and/or dislocated fracture.
Primary outcome - availability of PSA in the ED
Of the respondents, 56.8% (84/148) provided adult PSA and 20.3% (30/148) provided paediatric PSA in the ED.
Secondary outcomes Rationale for limited availability
The reasons why 43.2% of the respondents did not provide adult PSA were absence of trained staff to support PSA in the ED (34.4%), insufficient training and exposure (17.2%), insuff icient numbers to maintain skills (9.4%) and unsuitable space for PSA in the ED(4.7%), and for 34.6% the reason was unknown. For the 79.7% of the respondents who did not provide paediatric PSA the reasons were insuff icient training and exposure(32.2%), insuff icient numbers of trained staff to support PSA in the ED (24.6%), insuff icient numbers to maintain skills (22.0%) and unsuitable space for PSA in the ED(9.3%), respectively.
Quality
Self-assessment on prof ciency
PSA providers reflected on their PSA competencies in both adult and paediatric PSA (Tables 2 and 3).
Guideline adherence
The PSA procedure was documented in the medical record by 77.1%. Adverse events were registered by 42.7%. The respondents disclosed that for 61.4% of adult PSA and 55.6% of paediatric PSA the executor of the procedure was simultaneously providing the PSA.Medication of f irst choice is displayed in Table 1.
DISCUSSION
Our results show that availability of PSA was low in EDs without emergency physicians especially for paediatric patients. Absence of trained PSA professionals in the ED appears to be the main cause. Moreover,PSA guideline compliance and self-assessment on PSA proficiency appears to be rather low. This reflects a worrisome situation. Patients are likely not receiving PSA when needed in the ED, and if provided the staff may not be optimally proficient and not working according to the current guidelines. This raises some important concerns in the safety and quality of patient care.
Since the worldwide evolution of Emergency Medicine, safe PSA performance has markedly increased in the EDs.[10,11]In the Netherlands, EM residency training includes extensive PSA instruction and practice.[12]The national PSA training focuses on the importance of screening patients eligible for PSA,proper preparation of the PSA procedure, adequate knowledge on sedative and analgesic medications and their potential interactions, monitoring of the patient and ability to recognize and treat adverse events. Emergency physicians are also tested on their knowledge of thenational guideline as part of this training. A recent survey amongst Dutch emergency physicians revealed a much higher compliance to the national guideline.[9]For example, adverse event registrations was performed by 98% compared to 47% in the current studied population.These findings may indicate that solely distributing a national guideline appears to be insufficient. Rigorous training of PSA skills in combination with testing of guideline knowledge is probably needed to improve the current situation in EDs without emergency physicians.

Table 1. Survey results on PSA practice in adult versus paediatric patients in emergency departments without emergency physicians in the Netherlands
We acknowledge the limitations of our study. We aimed to survey as many ED nurses and physicians working in an ED instead of single expert opinions from each centre. Unfortunately the response rate (35.9%) was rather low. Participation was voluntary and anonymous to limit reporting bias. However, we cannot exclude all reporting bias.
This study demonstrates a low availability of PSA,low proficiency of PSA by self-assessment and a lack of guideline compliance in EDs without emergency physicians. There appears to be a clear need for rigorous training of ED health care professionals (nurses and physicians) and/or acquiring PSA professionals who are available in the ED and who are dedicated to improve PSA in the ED-setting. The results of our study may reflect similar difficulties with the implementation of emergency PSA in other countries without emergency physicians.
Funding:None.
Ethical approval: This study was approved by the Medical Ethics Committee.
Conf icts of interest: No benef its in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Contributors:MK and AK conceived the study, acquired and managed the data. MK, AK and NM analysed and interpreted the data. MK and FP drafted the manuscript. MK, AD, NM,MB and FP contributed substantially to its revisions. MK takes responsibility for the paper as a whole.

Table 2. Self-assessment by nurses, residents and consultant on adult PSA competencies (n=84)
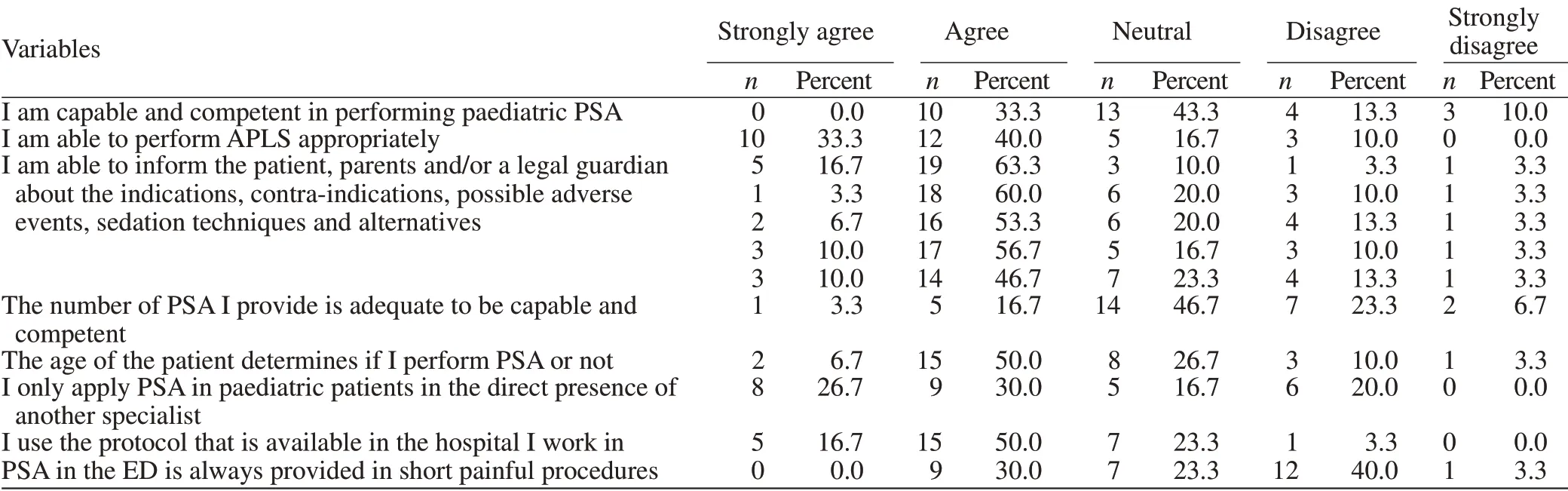
Table 3. Self-assessment by nurses, residents and consultant on paediatric PSA competencies (n=30)
 World journal of emergency medicine2020年2期
World journal of emergency medicine2020年2期
- World journal of emergency medicine的其它文章
- Presenting patterns of dermatology conditions to an Australian emergency department
- Effect of neutrophil CD64 for diagnosing sepsis in emergency department
- Post-dilatation improves stent apposition in patients with ST-segment elevation myocardial infarction receiving primary percutaneous intervention: A multicenter, randomized controlled trial using optical coherence tomography
- Predictive role of interleukin-6 and CAT score in mechanical ventilation in patients with chronic obstructive pulmonary disease at the acute exacerbation stage in the emergency department
- Changes in peak inspiratory f ow rate and peak airway pressure with endotracheal tube size during chest compression
- Comparison of invasive dynamic blood pressure between superior mesenteric artery and common carotid artery in rats
