Beneficial effects of AAV1-Rheb(S16H) administration in the adult hippocampus
Neurotrophic factors against neurodegenerative diseases such as Alzheimer’s disease (AD) and Parkinson’s disease (PD):A clear understanding of the etiology of neurodegenerative diseases, such as AD and PD remains elusive. Although there is still no therapy to prevent or block neurodegeneration, in vivo and in vitro experimental results have shown that the direct administration of neurotrophic factors, such as brain-derived neurotrophic factor (BDNF) and ciliary neurotrophic factor (CNTF), and the induction of these neurotrophic factors via specific gene delivery may protect neurons against neurotoxicity in neurodegenerative disease models (Kim et al., 2012; Jeong et al., 2013, 2015). However, the application of neurotrophic factors to treat brain diseases is limited by the bloodbrain barrier preventing macromolecular therapeutic agents from entering the central nervous system. Additionally, intra-cerebroventricular injection and intra-putaminal infusion of neurotrophic factors have led to limited penetration and distribution to the target brain areas (Peterson and Nutt, 2008; Nam et al., 2015). Neurotrophic factors that induce the sustained delivery of the appropriate amount to the target areas can be considered a potential therapeutic strategy for neurodegenerative diseases, such as AD and PD.
BDNF and CNTF in AD:BDNF, which is decreased in brains affected by AD, is a neurotrophin that mediates neuronal survival and differentiation, and its delivery has neuroprotective effects in animal models of AD (Arancibia et al., 2008; Nagahara et al., 2009; Jeon et al., 2015). CNTF, a neurotrophic cytokine belonging to the interleukin-6 family, is an important regulator of neuronal survival, neurogenesis, and neuronal plasticity in the central nervous system (Jeong et al., 2013; Jeon et al., 2019), and its delivery also alleviates cognitive impairments in models of AD in vivo and in vitro (Garcia et al., 2010; Wang et al., 2015).
The effects of these neurotrophic factors are mediated by specific receptors, such as tropomyosin receptor kinase B (TrkB) for BDNF (Jeon et al., 2015, 2019; Nam et al., 2015) and CNTF receptor (CNTFR), which is composed of its ligand-specific α subunit (CNTFRα); leukemia inhibitory factor receptor β; and gp130 for CNTF (Jeong et al., 2013; Jeon et al., 2019). Additionally, TrkB and CNTFRα for BDNF and CNTF binding, respectively, are well-expressed in hippocampal neurons (Jeon et al., 2019), and the stimulation of these receptors by treatment with neurotrophic factors activates the protein kinase B (Akt)/mammalian target of rapamycin (mTOR) signaling pathway, resulting in the downstream activation of pro-survival pathways in neurons (Jeong et al., 2013; Jeon et al., 2015, 2019; Nam et al., 2015). Interestingly, we have observed the presence of a neuroprotective system involving increases in reactive astrocytes and neurotrophic signaling receptors, such as TrkB and CNTFRα, in the lesioned hippocampi of AD patients, which may contribute to the protection of hippocampal neurons against neurodegeneration (Jeon et al., 2019). However, the endogenous construction of a neuroprotective system may be insufficient for controlling neurodegeneration in AD because of insufficient binding of neurotrophic factors to stimulate hippocampal receptors.
Importance of ras homolog enriched in brain (Rheb)/mTORcomplex 1 (mTORC1) signaling activation in hippocampi affected by AD:Many investigators have reported that the activation of the Akt/mTOR signaling pathway enhances the activity of intracellular cell survival pathways under a variety of conditions, such as ischemic shock, oxidative stress, and the withdrawal of trophic factors (Jeong et al., 2013; Jeon et al., 2015; Nam et al., 2015). mTOR kinase, which can play central roles in the integration of cell growth in response to various environmental conditions, exists in two complexes, mTORC1 and mTORC2 (Kim et al., 2012, 2014). Among these two complexes, mTORC1 is well known as an important mediator of many effects of Akt, which can be activated by mTORC2 and act as an activator of mTORC1, on the increased activities of intracellular cell survival pathways that are induced by neurotrophic factors (Kim, 2014; Nam et al., 2015).
The upstream regulator of the activation of mTORC1 is Rheb, which is a member of the small GTPase superfamily and encodes a lipid-anchored cell membrane protein with five repeats of the RAS-related GTP-binding region. Rheb can be activated by Akt and is involved in various cellular processes, such as protein synthesis, cell growth, proliferation, survival, and synaptic plasticity (Kim et al., 2012; Jeon et al., 2015; Nam et al., 2015). Rheb synthesis is upregulated, similarly to immediate early genes, after toxic insults or due to growth factors, such as epithelial growth factor or basic fibroblast growth factor (Kim, 2014; Nam et al., 2015). The effects of Rheb are mediated by tuberous sclerosis complex (TSC)1/TSC2, and GTP-bound active Rheb can stimulate mTORC1 activation, which enhances the activity of intracellular cell survival pathways (Kim et al., 2012; Jeon et al., 2015; Nam et al., 2015). Furthermore, the serine at position 16 of Rheb is sensitive to TSC GTPase activation, and Rheb(S16H), the constitutively active form of Rheb containing a serine to histidine mutation at position 16, results in the persistence of GTP-bound Rheb in an activated state because of resistance to TSC activation (Kim et al., 2012; Jeon et al., 2015; Nam et al., 2015), suggesting that Rheb(S16H) expression can strongly induce mTORC1 activation.
Although Rheb mRNA has been shown to be rapidly and transiently induced in hippocampal granule cells by seizures and by N-methyl-aspartate-dependent synaptic activity in a long-term potentiation paradigm, recent findings have demonstrated that Rheb could be dysregulated in the brains of patients with AD (Jeon et al., 2015, 2019). Moreover, there was a report showing that Rheb upregulation could promote the degradation of β-site amyloid precursor protein-cleaving enzyme 1 in a model of AD; however, the effects of Rheb on the level of β-site amyloid precursor protein-cleaving enzyme 1 were mTORC1-independent (Shahani et al., 2014). Recently, I and my colleagues reported that the activation of Rheb/mTORC1 signaling pathways by a delivery of Rheb(S16H) using adeno-associated virus 1 (AAV1), which could sustainably deliver the target protein to the specific brain areas through the stereotaxic brain surgery (Kim et al., 2012; Jeon et al., 2015; Nam et al., 2015), induced neurotrophic effects in the hippocampus, and protected hippocampal neurons against thrombin-induced neurotoxicity (Jeon et al., 2015, 2019). These observations suggest that the upregulation of active Rheb, which can induce mTORC1 activation, may be an important mechanism for the survival of hippocampal neurons in the adult brain.
Neuroprotective interactions between neurons and astrocytes in the AAV1-Rheb(S16H)-transduced hippocampus in vivo:
Astrocytes, which are the most abundant cells in the brain, play an important role in homeostatic maintenance. Although excessive astrocyte activation may be involved in neurodegeneration through inflammatory responses in the adult brain, reactive astrocytes can also induce beneficial effects, such as increasing neuronal survival, growth, and activity through barrier function to restrict tissue damage and neuroinflammation, as well as by producing neurotrophic factors, as demonstrated in animal models of neurodegenerative diseases (Jeon et al., 2019). Recently, in AAV1-Rheb(S16H)-treated rat hippocampi, we observed morphological changes in astrocytes with no significant change in the levels of pro-inflammatory cytokines, which could induce neurodegeneration in the adult brain (Jeon et al., 2019), suggesting that astroglial activation following Rheb(S16H) transduction of hippocampal neurons might contribute to AAV1-Rheb(S16H)-induced neuroprotection.

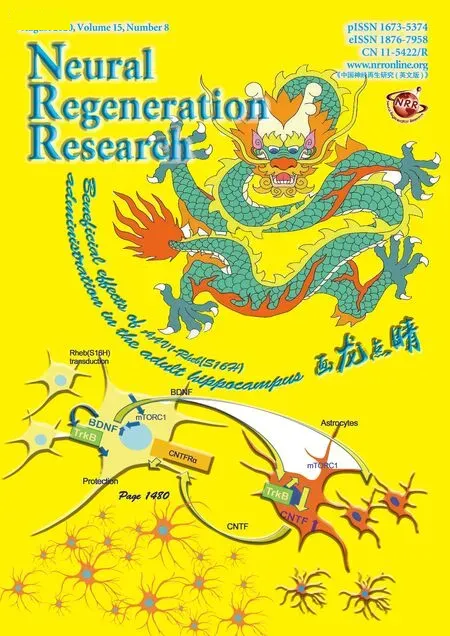
Figure 1 Schematic representation of the construction of a neuroprotective system following AAV-Rheb(S16H) administration.
The sustained activation of the Rheb/mTORC1 signaling pathway in adult neurons can produce neurotrophic factors in the adult brain in vivo (Jeon et al., 2015; Nam et al., 2015). In a recent study, the induction of Rheb(S16H) in hippocampal neurons by AAV1 transduction was shown to activate the mTORC1 signaling pathway, resulting in the production of neuronal BDNF and astrocytic TrkB and CNTF as neuroprotective biomolecules against thrombin-induced neurotoxicity in the rat hippocampus, though the transduction of Rheb(S16H) by AAV1 administration was limited within hippocampal neurons (Jeon et al., 2015, 2019). Moreover, we observed that the upregulation of astrocytic CNTF contributed to neuroprotection against thrombin-induced neurotoxicity in the hippocampus in vivo (Jeon et al., 2019), suggesting that the upregulation of BDNF induced by neuronal transduction with AAV1-Rheb(S16H) could stimulate astroglial activation, supporting the neuroprotective effects through the production of astrocytic CNTF in the adult hippocampus. Additionally, neuronal BDNF produced by Rheb(S16H) transduction protects hippocampal neurons through the autocrine signaling pathway, indicating activation of neuronal TrkB in the hippocampus in vivo (Jeon et al., 2015, 2019).In conclusion, our recent results suggest that viral transduction of hippocampal neurons, through methods such as AAV1-Rheb(S16H) administration, can intensify the construction of a potential neuroprotective system, which was demonstrated in the hippocampus of a rat AD model, through functional interactions between neurons and astrocytes triggered by an increase in neuronal BDNF. We also demonstrated that the intensified neuroprotective system following AAV1-Rheb(S16H) administration contributes to neuroprotection by both autocrine and paracrine signaling activation in the hippocampus (Figure 1). Additionally, the induction of Rheb might have contributed to a reduction of amyloid beta peptide generation (Shahani et al., 2014). Thus, although further studies are needed to identify the clinical relevance of the AAVRheb(S16H) transduction approach for neurodegenerative diseases, the AAV1-Rheb(S16H) transduction approach may be considered a useful strategy for protecting hippocampal neurons in the lesioned brain, and its effects may be relevant to patients with AD.
This work was supported by grants from the National Research Foundation of Korea (NRF-2017R1A2B4002675, to SRK), and the Korea Healthcare Technology R&D Project, funded by the Ministry of Health & Welfare, South Korea (HI14C1135).
Sang Ryong Kim*
School of Life Sciences; BK21 plus KNU Creative BioResearch Group; Institute of Life Science & Biotechnology; Brain Science and Engineering Institute, Kyungpook National University, Daegu, Korea
*Correspondence to:Sang Ryong Kim, PhD, srk75@knu.ac.kr.
orcid:0000-0003-0299-1613 (Sang Ryong Kim)
Received:November 15, 2019
Peer review started:November 19, 2019
Accepted:December 7, 2019
Published online:January 31, 2020
doi:10.4103/1673-5374.274335
Copyright license agreement:The Copyright License Agreement has been signed by the author before publication.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Open peer reviewer:Paulina Carriba, Cardiff University, UK.
Additional file:Open peer review report 1.
- 中国神经再生研究(英文版)的其它文章
- Exercise promotes recovery after motoneuron injury via hormonal mechanisms
- Large animal ischemic stroke models: replicating human stroke pathophysiology
- Autophagy and inflammation in ischemic stroke
- Electrical stimulation and denervated muscles after spinal cord injury
- Beneficial effects of saffron (Crocus sativus L.) in ocular pathologies, particularly neurodegenerative retinal diseases
- Toxic tau: structural origins of tau aggregation in Alzheimer’s disease