Electrical stimulation and denervated muscles after spinal cord injury
Subhalakshmi Chandrasekaran, John Davis, Ines Bersch , Gary Goldberg , Ashraf S. Gorgey,
1 Spinal Cord Injury and Disorders, Hunter Holmes McGuire VA Medical Center, Richmond, VA, USA
2 Swiss Paraplegic Centre, Nottwil, Switzerland
3 Institute of Clinical Sciences, Department of Orthopedics at the University of Gothenburg, Gothenburg, Sweden
4 Department of Physical Medicine and Rehabilitation, Virginia Commonwealth University, Richmond, VA, USA
5 Electrodiagnostic Center, Hunter Holmes McGuire VA Medical Center, Richmond, VA, USA
Abstract Spinal cord injury (SCI) population with injury below T10 or injury to the cauda equina region is characterized by denervated muscles, extensive muscle atrophy, infiltration of intramuscular fat and formation of fibrous tissue. These morphological changes may put individuals with SCI at higher risk for developing other diseases such as various cardiovascular diseases, diabetes, obesity and osteoporosis. Currently, there is no available rehabilitation intervention to rescue the muscles or restore muscle size in SCI individuals with lower motor neuron denervation. We, hereby, performed a review of the available evidence that supports the use of electrical stimulation in restoration of denervated muscle following SCI. Long pulse width stimulation (LPWS) technique is an upcoming method of stimulating denervated muscles. Our primary objective is to explore the best stimulation paradigms (stimulation parameters, stimulation technique and stimulation wave) to achieve restoration of the denervated muscle. Stimulation parameters, such as the pulse duration, need to be 100-1000 times longer than in innervated muscles to achieve desirable excitability and contraction. The use of electrical stimulation in animal and human models induces muscle hypertrophy. Findings in animal models indicate that electrical stimulation, with a combination of exercise and pharmacological interventions, have proven to be effective in improving various aspects like relative muscle weight, muscle cross sectional area, number of myelinated regenerated fibers, and restoring some level of muscle function. Human studies have shown similar outcomes, identifying the use of LPWS as an effective strategy in increasing muscle cross sectional area, the size of muscle fibers, and improving muscle function. Therefore, displaying promise is an effective future stimulation intervention. In summary, LPWS is a novel stimulation technique for denervated muscles in humans with SCI. Successful studies on LPWS of denervated muscles will help in translating this stimulation technique to the clinical level as a rehabilitation intervention after SCI.
Key Words: denervation; DXA; electrical stimulation; LMN injury; LPWS; MRI; spinal cord injury; stimulation parameters
Introduction
Prevalence of spinal cord injury (SCI) has been estimated to be 250,000-400,000 with an estimated 14% growth since 1988 (Devivo et al., 2002; Strauss et al., 2006). An immediate loss of voluntary movement and contractile force is one of the most crippling effects of SCI which often results in remarkable muscle atrophy within the first few months post injury (Kern et al., 2010). This is accompanied by increased intramuscular fat. This is followed by dramatic changes in body composition characterized by decreasing percentage lean mass and increasing fat mass as well as subsequent reduction in basal metabolic rate and thus leads to increasing prevalence of obesity among the SCI population (Gorgey and Gater, 2007; Gorgey et al., 2014). This increase in ectopic adiposity is likely to be associated with reduction of muscle mass and is linked to several cardio-metabolic disorders and other health-related comorbidities, such as reduced aerobic fitness, glucose intolerance, insulin resistance, and decrement in mitochondrial function (Gorgey et al., 2014; Sumrell et al., 2018). These secondary health related consequences may lead to several disparities which challenge the productivity, quality of life, and well-being of those with SCI, but may be reversible with appropriate exercise or pharmaceutical interventions (Gorgey et al., 2019). This is primarily of interest because advances in neuroscience research may offer the development of novel rehabilitative intervention for functional restoration after SCI (McDonald and Sadowsky, 2002).
Individuals with SCI may suffer an upper motor neuron (UMN) lesion, lower motor neuron (LMN) lesion, or a combination of both. Clinically, it is necessary to determine whether an individual has an UMN or LMN lesion (Kirshblum et al., 2011). The type of lesion whether UMN or LMN, cannot be determined solely based on the neurological level of the injury (Doherty et al., 2002). Within the spinal column, damage to the motor unit can involve motor neuron cell bodies in the spinal segment of the cord or axonal damage at the spinal root level. Following UMN lesion, the inhibitory pathways get disrupted and can be followed by loss of voluntary motor controls. Clinically, a UMN lesion above the lumbar spinal cord segments may lead to spastic paralysis and exaggerated deep tendon reflexes in the paralyzed limbs (Doherty et al., 2002). In contrast, the effects of LMN damage can be associated with severe muscle atrophy, hypotonia, fibrillations in the muscles, and flaccid paralysis in the lower limbs (Doherty et al., 2002).
Anecdotal evidence from our laboratory suggests that about 20-25% of the SCI population experiences LMN denervation. Due to the lack of innervation, the denervated muscles cannot be activated using the standard commercially available electrical stimulator units. Currently, there is no available rehabilitation intervention for SCI individuals with LMN denervation.
The primary objectives of the current mini-review are 1) to review the consequences of denervation in SCI persons with LMN injury and 2) to explore the available stimulation paradigms of electrical stimulation from animal and human models with LMN injury. Results from this review will facilitate a greater understanding of the methodology necessary to determine the impact of long-term exercise on muscle hypertrophy, as well as metabolic and local cellular adaptations following LMN injury after SCI.
Search Strategy and Selection Criteria
We searched PubMed, Web of Knowledge, MEDLINE, and Google Scholar for studies that reported the effects electrical stimulation in denervated muscles after spinal cord injury (SCI). We used the following search strategy (SCI* OR LMN injury* OR Denervation* OR Cauda Equina Injury) AND (electrical stim* OR Functional Electrical Stimulation* OR LPWS* OR stimulation therapy). No restrictions by publication period were used. In addition, we manually scanned the references list of retrieved articles for relevant studies.
Lower Motor Neuron Injury and Denervation
LMN injury is commonly accompanied by peripheral nerve injury to the sensory, motor, autonomic, and terminal branches of the peripheral nervous system. Based on the severity of the injury, and whether there is continuity of the nerve preserved or not, peripheral nerve injury is classified into three major types (Seddon, 1968); 1) Neurapraxia, 2) Axonotmesis and 3) Neurotmesis. A simplified illustration of the different types of peripheral nerve injury based on Seddon’s classification is shown in Figure 1.
Neurapraxia is known to be the mildest form of peripheral nerve injury and is characterized by temporary interruption in the conduction of the impulses however, there is no loss of axonal continuity. Concussive or shock-like injury to the fiber by either a compressive, tensile, or chemotoxic insult can also result in a biomechanical lesion. The other two types of peripheral nerve injury are axonotmesis and neurotmesis. These types of injury usually occur due to a more severe crush or a contusion injury and can be characterized by loss of relative continuity of the neuron (Carp, 2015). Neurotmesis, is the most severe kind of injury involving peripheral nerves, based on the level of trauma and the impact of the damage. In this case, severe compression, or tension injury occurs affecting the nerve and axonal continuity. Along with axonal injury, the encapsulating connective tissue is damaged resulting in complete loss of motor, sensory and autonomic functions. In addition, electromyography examinations performed 2-3 weeks after the injury shows fibrillations and denervation potentials in the skeletal muscles distal to the injury site. Partial functions may be retained in some cases if there is a dual dermatomal or myotomal innervation present through an undamaged peripheral nerve fiber (Carp, 2015).
The cellular changes that occur in the nerve stumps located distal to the lesion site are collectively described as Wallerian degeneration (Rotshenker, 2011). This is a process that follows after axonotmetic and neurotmetic nerve injuries (Kaye, 1991). Following loss of axonal continuity, axonal degeneration occurs as a result of separation from the neuron’s nucleus.
The process of degeneration usually begins 24 to 36 hours after the injury (Coleman and Freeman, 2010). The rate of Wallerian degeneration depends on various factors like species, axonal diameter and the length of the distal segment (Gilliatt and Hjorth, 1972; Lubińska, 1977; Beirowski et al., 2005).
The first response following axonal injury is acute axonal degeneration, characterized by the separation of the proximal and distal parts of the axon within the first 30 minutes of injury (Kerschensteiner et al., 2005). The axolemma then swells up in the form of a bead; which takes about 24 hours. The axolemma then undergoes degradation followed by granular disintegration of the axonal cytoskeleton and the inner organelles.
Response following Denervation
The severity of SCI is described by the International Standards for Neurological Classification of Spinal Cord Injury. Individuals with denervation after SCI could have traumatic complete or incomplete SCI with injury level T10 or below; also known as conus and cauda equina lesion. The lesion results in motor deficit below the level of injury. Figure 2 shows the conus medullaris and the cauda equina region.
Individuals with SCI and LMN denervation exhibit dramatic musculoskeletal and dermal changes below the level of injury. Denervation leads to a great loss in muscle mass and preserving skeletal muscle integrity is vital for the maintenance of cellular and whole-body metabolism (Pedersen and Febbraio, 2008, 2012; Kanzleiter et al., 2014). These individuals are at an increased risk for several chronic diseases such as type II diabetes, dyslipidemia, cardiovascular disease and osteoporosis.
Skin quality following denervation
Skin is the largest organ in the body and acts as a protection for the internal organs against physical, chemical and biological insults (Albertin et al., 2018). Skin quality is associated with the integrity of the skin, including perfusion of the deep tissue and sufficient blood flow in the vascular system. Loss of blood supply to the soft tissue, immobility, and pressure from internal bony prominence can typically lead to pressure sores (Dolbow et al., 2013). These physiological changes are why persons with SCI are known to be at the highest risk for developing pressure ulcers (Kruger et al., 2013). Most decubitus ulcers or pressure injuries occur in the sacral area in persons with spinal denervation. In this region, the ischial tuberosities as well as the coccyx are particularly exposed. Anatomically, there is no muscle mass superficial to protect these bony structures. Muscle atrophy also decreases the presence of soft tissue and vascularity. This results in the loss of the desired cushioning effect, heightening the risk of pressure ulcers (Liu et al., 2006). Pressure ulcers can have consequences like limited mobility, decreased quality of life, and they can hinder everyday activities (Chen et al., 2005). Pressure ulcers, when left untreated, can increase in severity and become extremely difficult to restore leading to serious medical conditions and possibly even life-threatening problems (Garber and Rintala, 2003).
Electrical stimulation has been widely used as a treatment or prevention method for pressure ulcers in the past few decades (Houghton et al., 2010; Curtis et al., 2011; Franek, et al., 2012). It has been demonstrated that electrical stimulation therapy stimulates wound healing, by promoting the activation and proliferation of major key factors such as fibroblast, growth factors, and epithelial cells (Bourguignon and Bourguignon, 1987; Sheridan et al., 1996; Houghton et al., 2010).
Bone degradation following denervation
Denervation also leads to continuous bone resorption and osteoporosis. Previous studies have concluded that bone osteoporosis occurs as a result of lack of muscle activity (Gillespie, 1954; Gargiulo et al., 2011). This may be attributed to the micro and macro structural changes due to the loss of muscle contraction and weight bearing (Zamarioli et al., 2014). Figure 3 shows the DXA scan of the pelvic region including hip bone and femoral neck in a person with T7 American Spinal Injury Association Impairment Scale grade C following 6.5 years with LMN SCI. Notice the anatomical changes that occur in the femoral head and hip joint following injury. Based on the anatomical region, the bone mineral density can diminish by about 50% at the distal epiphyses of the femur and by 60% at the proximal epiphyses of the tibia post 3-4 years after SCI (Eser et al., 2004). The risk of fracture in an individual with SCI is twice as high the risk of fracture in an able-bodied individual (Eser et al., 2004). About 50% of individuals with complete SCI experience a post-injury bone fracture at some point (Morse et al., 2009). Complications such as increased pain, spasticity, pressure ulcers, risk of non-union fracture, and limb amputation are common post fracture (Morse et al., 2009).
Non-invasive rehabilitative techniques to restore bone strength and density post-SCI are becoming increasingly popular. Several studies have demonstrated that electrical stimulation for exercise, cycling, and standing, for muscle strengthening, induces an increase in bone mass (Chen et al., 2005; Shields and Dudley-Javoroski, 2006; Lauer et al., 2011; Zamarioli et al., 2013). Previous work by Johnston et al. (2016) has suggested that 6 months of functional electrical stimulation (FES) to the paralyzed muscles results in remarkable improvement in trabecular bone parameters after SCI. However, this supportive evidence is still lacking following LMN injury after SCI. There is also inconclusive evidence to support that improvement in muscle quality may lead to direct improvement to bone health following SCI.
Muscle atrophy following denervation
There are several biochemical, morphological and physiological changes that occur in the muscle fiber following denervation with muscle atrophy being the most prominent. Within the first few months post-injury, there is rapid onset of skeletal muscle atrophy and decrease in fat free mass (Kocina, 1997; Castro et al., 1999; Spungen et al., 2000; Buchholz and Bugaresti, 2005; Md and Clasey, 2006; Gorgey and Dudley, 2007, 2011; Gorgey et al., 2011). The dramatic muscle atrophy after SCI begins within a few weeks of injury and continues at least until the end of the first year (Castro et al., 1999; Gorgey and Dudley, 2007). Skeletal muscle cross sectional area (CSA) could be as low as 50% compared to healthy able-bodied controls (Castro et al., 1999). Muscle atrophy is also associated with a massive adipose tissue infiltration of intramuscular fat (Gorgey and Dudley, 2007). The extensive muscle atrophy has been attributed to a number of factors including reduction in the level of physical activity, unloading, disuse, and reduction in anabolic hormone secretion as well as an increased release of proinflammatory cytokines (Castro et al., 1999; Md and Clasey, 2006; Sumrell et al., 2018; Abilmona et al., 2019). This is further accompanied by an increase in fat mass (Kocina, 1997; Spungen et al., 2000; Buchholz and Bugaresti, 2005; Md and Clasey, 2006), waist circumference (Buchholz and Bugaresti, 2005) and visceral adiposity (Castro et al., 1999; Gorgey and Gater, 2011).
The rate of muscle atrophy varies among different species, different individuals of the same species, different muscle groups in the same individual, and sometimes even within the fibers in the same muscle group (Eberstein and Eberstein, 1996). In rats, two weeks after denervation, the hindlimb weight is reduced by 50%. Whereas in humans, within the same time frame, changes may be negligible, taking about 2-3 months of denervation for the muscle fibers to reduce by 50% in diameter (Adams, 1975; Ohira, 1989). Furthermore, in rats, the extensor digitorum longus muscle atrophies at a slower rate as compared to the soleus muscle (al-Amood et al., 1991; Wroblewski et al., 1989).

Figure 1 Seddon’s classification of peripheral nerve injury.
Following denervation, the muscles proceed to terminal atrophy; this process can be divided into various stages. The duration of these stages is different in different species. For example, each stage could be several months in laboratory animals like rats; but it might take years to progress through similar stage in case of humans (Carlson, 2014). This progressive decline of the muscles post-denervation can be mainly divided into three main stages (Tower, 1935; Lapalombella et al., 2008). The first stage begins immediately after the nerve injury and is mainly characterized by immediate loss of function resulting in expedited muscle fiber atrophy and rapid weight loss. In rats, this phase lasts for two months. The denervated muscles have restorative capacity equal to that of a normal control muscle, although by the end of the first phase, the muscle loses 90% of its original mass. During the second stage, there is an extreme muscle atrophy, along with the break-down of sarcomere and muscle fiber organization. In rats, from 2-7 months, there is a striking fall in the restorative ability of the muscles during this stage. The third stage, also known as the terminal stage, is when the tissue architecture undergoes fibrosis; this phase starts post 7 months in rats and is characterized by severely diminished muscle fibers accompanied by an excessive increase of adipocytes that is referred to as fat infiltration (Gulati, 1990; Carlson et al., 1996, 2002). Mödlin et al. (2005) found that in human subjects the rate of muscle degeneration after denervation is slower. The quadriceps muscles of an individual denervated for 0.7 years consists of small, multiangular myofibers with a mean diameter of 18.6 μm. After 4 years quadriceps consist of severely atrophic myofibers with mean diameter of 9.0 μm. It is also during this period that the muscle fibers begin to be substituted by adipocytes and collagen. Post 8.7 years of denervation the muscles enter the long-term stage defined by minimal muscular structure consisting of multiangular, atrophied fibers measuring 7.9 μm (Mödlin et al., 2005). As severe atrophy develops post SCI, the muscle tissue undergoes both fibrosis as well as fat infiltration, hence producing denervated degenerated muscle (Carraro et al., 2015). Using sciatic nerve injury as a common denervation model, there were elevations of ubiquitin ligase genes, MAFbx and MURF1 over the course of 2 weeks. Despite the initial increase in insulin-like growth factor-1 in the first 3 days, with increase in fibrillation, there were noted declines in insulin-like growth factor-1 which was correlated with the extent of atrophy (Zeman et al., 2009). In Figure 4, note the dramatic muscle atrophy in the right thigh following SCI in a person with partial denervation as measured by magnetic resonance imaging. Contractile tissue is completely diminished, and muscle fibers were replaced with infiltrated fat and connective tissues. Failure to restore muscle size may lead to serious health-related complications including obesity, higher risk of type II diabetes and cardiovascular diseases (Castro et al., 1999; Buchholz and Bugaresti, 2005; Md and Clasey, 2006; Gorgey and Dudley, 2007; Gorgey et al., 2011; Gorgey and Gater, 2011). Therefore, providing electrical stimulation paradigm may facilitate restoration of denervated muscle following SCI. Surface neuromuscular electrical stimulation (NMES) has been recommended as an effective rehabilitation approach that facilitates restoration of muscle bulk after UMN lesion SCI (Ryan et al., 2013).

Figure 2 Briefly summarizes the anatomy of the conus medullaris and the cauda equina.

Figure 3 Dual-energy X-ray absorptiometry scan of the right (A) and left (B) hip joints of a denervated individual with T7 level of injury.
Excitability of denervated muscles
The excitability of a tissue is determined mainly by two parameters, stimulation amplitude and pulse duration. The relationship between these two parameters is called the strength-duration curve. Rheobase and Chronaxie are two points on this curve that can be used to accurately describe the excitability of the tissue. Rheobase is defined as the minimum amplitude of the stimulus that is required to trigger a response at an infinitely long pulse duration. Whereas, chronaxie can be defined as the minimum pulse duration required to elicit a response when the amplitude is twice the rheobasic strength (Ashley et al., 2005).
One of the many changes that occur in the skeletal muscles after denervation is decrease in the excitability of the muscle. Chronaxie, the tissue-excitability constant is especially high in case of denervated muscles. Based on the chronaxie, the optimum pulse duration used to stimulate the muscles is determined (Geddes, 2004). It has to be about 100-1000 times longer for denervated muscle to respond to stimulation as compared to innervated muscle (Kern et al., 1999). Denervated muscles respond to longer pulse duration compared to those that are adequate to elicit a response for innervated muscles (Ashley et al., 2005).
Previous studies on the strength-duration curve by Ashley et al. (2005) have successfully found the effect of denervation on parameters like rheobase and chronaxie. Six New Zealand rabbits were denervated and their TA muscle was implanted with stimulator. Rheobase was determined with a constant pulse duration of 100 ms and the amplitude used to determine the Chronaxie was twice the Rheobase. Chronaxie increased 3 times over the course of 2 weeks of denervation (Ashley et al., 2005).
Following complete denervation, paralyzed muscles in the lower limb may demonstrate large amounts of fibrillation potentials (Katirji, 2007). The fibrillation activity is an indication of significant LMN pathology with likely damage at the segmental or at the radicular level where the peripheral axons are damaged leaving the muscles denervated (Purves et al., 2004). In this situation, the muscle fiber membrane becomes electrically unstable and the fiber starts to fibrillate at about 21 days after the injury (Katirji, 2007). Fibrillation continues until the fiber is either re-innervated or it degenerates to the point where it becomes electrically silent. However, most persons with SCI lesions are discomplete, showing signs of residual neurophysiological brain control below the level of lesion (Sherwood et al., 1992). These individuals with T11-12 complete SCI may show no signs of abnormal fibrillation activity in the lower limb muscles, or only a very limited amount of abnormal spontaneous activity and could actually have some reflexively activated or otherwise limited spontaneous motor unit activity. In these individuals, the peripheral axons and motor neurons at the segmental level are most likely relatively intact with the pathology being primarily suprasegmental. Using electromyography techniques, muscle activity can be determined before and after long pulse electrical stimulation treatment to evaluate the effects on denervated muscles.
Neuromuscular Electrical Stimulation
The application of Electrical current to neuromuscular junctions and its surrounding muscle fibers to trigger muscle contraction is referred to as NMES (Bax et al., 2005). This form of electrical stimulation has been widely used in conjunction with other rehabilitation techniques in individuals with SCI. It is used to evoke muscle hypertrophy, relax muscular spasms, increase range of motion, prevent muscle atrophy, and increase peripheral blood flow (Pichon et al., 1995; Maffiuletti et al., 2000). NMES has been used to train atrophied muscles in rehabilitative settings as well as athletic or preventive strength training (Pichon et al., 1995; Maffiuletti et al., 2000; McDonough and Kitchen, 2002). Pichon et al. (1995) found that by using electrical stimulation strength training on the latissimus dorsi of athletes, performance was increased by 30% over the course of 3 weeks. Ryan et al. (2013) noted an increase in muscle mass of 30% post sixteen weeks of home-based electrical stimulation resistance training. Gorgey et al. (2019) have recently used electrical stimulation with resistance training to evoke muscle hypertrophy and increase basal metabolic rate in persons with SCI. Several other studies have used electrical stimulation during cycling or exercise to improve muscle health, bone health and metabolic profile in the SCI population (Johnston et al., 2016; Gorgey et al., 2019). Several reports have highlighted the significance of using NMES-resistance training to provoke 35-40% hypertrophy in individuals with chronic SCI (Mahoney et al., 2005).
Unfortunately, individuals with SCI who present with LMN injury as evidenced by muscle denervation cannot benefit from standard NMES. Following LMN injury, the affected skeletal muscle experiences extensive loss of contractile material as well as undergoes fibrosis and fat infiltration (Boncompagni, 2012; Carraro et al., 2015). Unpublished data from previous studies suggests that approximately 20-25% of the SCI population experience injury to their conus medullaris which may lead to LMN denervation. Denervated muscles do not respond to typical stimulation, therefore we aim to explore the benefits of LPWS as a means to stimulate these muscles.
Electrical Stimulation as a Treatment for Denervated Muscles
According to the current European regulations for the stimulators, the maximum output energy for the standard NMES is 300 mJ per impulse. Most commercially available stimulators have an amplitude that does not exceed 200 mA because of an increased risk of skin irritation and burns, especially in individuals with SCI. However, this is not sufficient to trigger usable contractions in denervated muscles via surface electrodes, unless these muscles remain partially innervated (Mayr et al., 2002). Unpublished data suggests that 25% of the SCI population cannot benefit from the standard NMES protocol because of LMN denervation.
Denervated muscles have lost their peripheral nerve supply. This results in a decrease in the amount of tension which can be generated and an increase in the time required for contraction. In individuals with denervated muscles, various parameters need to be modified as compared to the standard NMES in order to achieve desirable muscle contraction and minimize muscle atrophy. As the amplitude or pulse duration increase, the nerve fibers nearest the electrodes are depolarized to activate the target muscle. All available NMES applications are based on direct excitation of neural structures and indirect activation of the target muscle. Due to the denervation, the cellular membrane of each target muscle fiber must be depolarized to elicit muscular contractions (Boncompagni, 2012). The average pulse duration used for individuals with LMN denervation is 100-200 ms. The intensity of the current should be sufficient to elicit strong contractions and the pulse duration should be greater than or equal to the chronaxie of denervated muscles. This pulse has extremely long duration and is expressed in milliseconds (ms) as compared to the standard NMES in microseconds (μs).
The European project, Research and Innovation Staff Exchange has developed a novel technique, LPWS, which is capable of training and restoring muscle size following denervation in persons with SCI (Kern et al., 2009; Boncompagni, 2012; Carraro et al., 2015). Biphasic rectangular direct current (DC) impulses with duration between 30-150 ms and a frequency in between 2-22 Hz may have to be applied with an amplitude higher than that of standard NMES (200 mA) to maximize the electrical charges and to exceed the chronaxie of the denervated muscles. This imposes direct activation of the myofibers independent of LMN denervation. Continuous stimulation can increase the excitability of the denervated muscles, and the pulse duration can be gradually regulated down to 30-50 ms. The LPWS has the capacity to penetrate deeply and activate muscle fibers. For this much current, large size rubber electrodes of 12 × 15 cm with salt free gel covered with wet spongy pads should be used to reduce chances of electrical burn of the exposed skin (Figure 5).
LPWS has been proven to restore functional use of muscles post denervation. An extensive amount of research has been done to explore the benefits of FES in denervated muscles in animal models. One study on 42 male rats with denervated tibialis anterior muscle showed positive effects on the muscle weight and a significant increase in bone strength in the denervation with electrical stimulation group (Tamaki et al., 2017). Morphological findings in another study, post electrical stimulation on cranial tibialis muscle in rats showed that the experimentally denervated and treated group had no significant difference when compared with initial control group (Bueno et al., 2017). Another study involving adult horses with transected laryngeal nerve showed improvement in inspiratory loads following 8 weeks of stimulation (Cheetham et al., 2015).

Figure 4 A comparison between two patients with SCI.

Figure 5 Placement of the electrodes in a SCI patients with LMN.
Human studies are beginning to emerge, that support the findings of previous animal studies showing that LPWS can potentially be established as the rehabilitation technique for muscle restoration post denervation. Previous study on FES, on individuals with varied levels of denervation demonstrated regain of active standing up of 7 patients over a 2-year training period (Kern et al., 1999). The effects of home-based FES using LPWS (120-150 ms) at an intensity of 250 mA for 5 days/week has been studied for two years in 25 SCI persons with complete LMN denervation (Kern et al., 1999, 2002; Carraro et al., 2002; Hofer et al., 2002). The trial showed that knee extensor CSA increased by 24% following the first year and an additional 7% in the second year, respectively, with no changes in the CSA of the hamstring muscles (Kern et al., 2010).
Tables 1 and 2 provide a brief literature review of electrical stimulation of denervated muscles in animal models and humans, respectively. The parameters and the specific techniques used are highlighted in order to better understand the effects of electrical stimulation on denervated muscles.
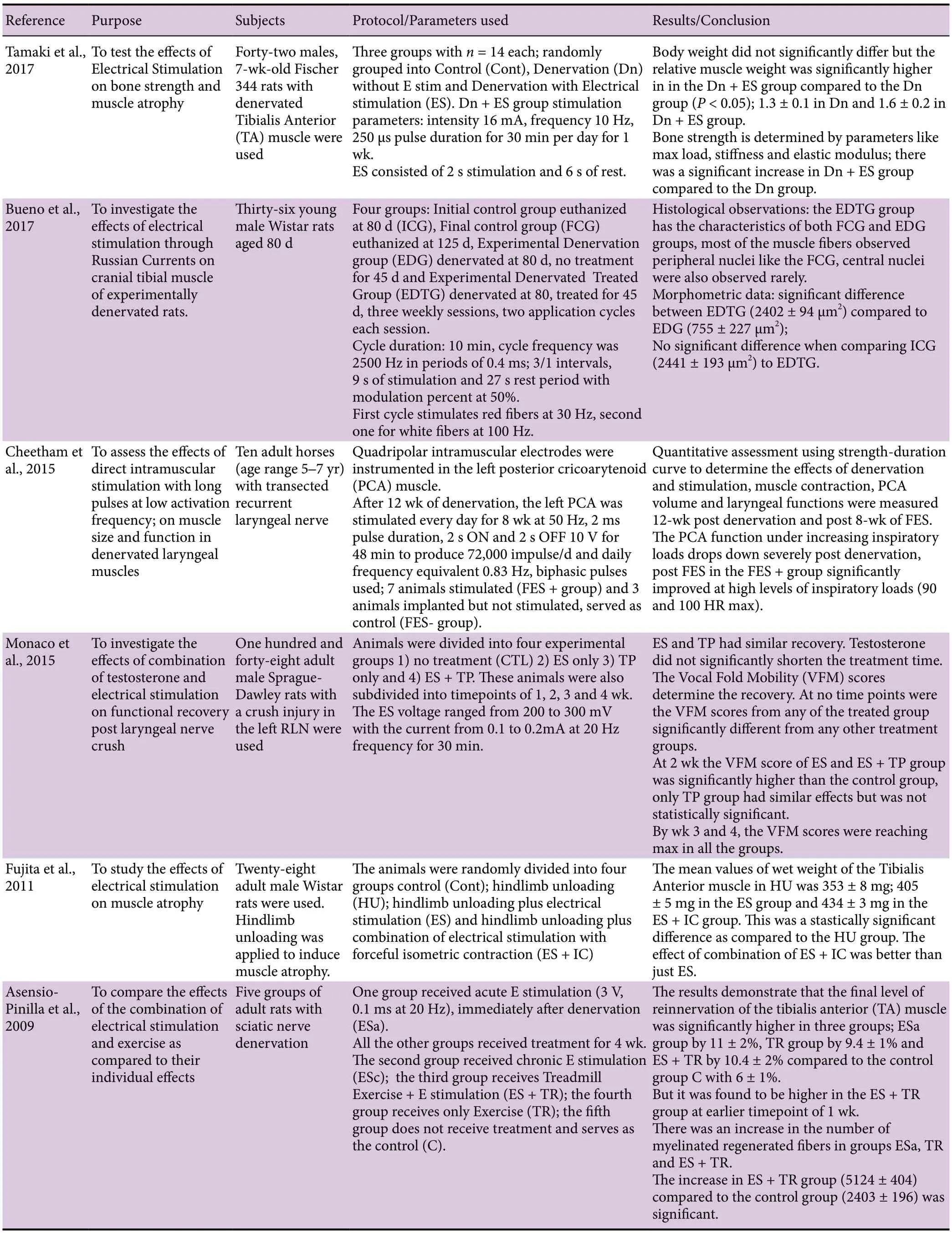
Table 1 Functional electrical stimulation (FES) of denervated muscles in animal models

Table 1 Continued

Table 2 Functional electrical stimulation (FES) of denervated muscles in humans
Simulation parameters used with lower motor neuron Currents
There are two types of electrical stimulation current that have been commonly used to activate the paralyzed muscles: either DC or alternating current (AC). In DC, the flow of electrons is in one direction and is considered constant, while the flow using AC could be either unidirectional (monophasic) or bidirectional (biphasic); symmetrical or asymmetrical. AC can be represented as a sine wave to visualize the flow of electrons. AC is usually delivered at high frequencies which reduces the effect of skin impedance, resulting in more current being delivered to the motor units of the target area. With continuous DC, the current intensity needs to reach the threshold for the motor unit for muscle contraction to occur. The ability of DC to cause chemical changes is one of the biggest differences between AC and DC (Howe and Trevor, 2002; McDonough and Kitchen, 2002).
Pulse
A pulse could be discrete, or it could be a series of pulses or a pulse train. A sudden step of short duration of voltage or current to form a steady value is called a pulse (Howe and Trevor, 2002). The pulse can have different shapes like square, rectangular and triangular pulse. They could be delivered at different durations depending on the requirement of the training.
Pulse duration
The pulse duration, also known as the pulse width is the time between the onset and offset of the stimulus. It is expressed in μs or ms. The pulse duration required to generate a contraction in denervated muscle is usually 100-1000 times greater than that required to elicit the same response for the innervated muscles (Kern et al., 1999).
It is worth noting that the outcome of the training is primarily determined by the initial condition of the denervated muscles. Those in the chronic stage, 2 years or more after denervation, may take up to 12 weeks to illicit a twitch response and even longer to create a tetanic contraction. Denervated muscles following 5 years of SCI, especially in older individuals (> 40 years of age) may require extensive training and longer duration of training to elicit reasonable tension. Muscle restoration within 5 years of denervation is more desirable. Post 5 years of denervation, there is severe loss of muscle and fat substitution advances so far that it is highly challenging at this point to attempt restoration (Kern et al., 2002).
Initially, the LPWS with limited frequency is likely to elicit twitches of the denervated muscles in the acute and subacute phase after SCI. After 3 months, the pulse duration can be shortened by 30-50 ms with the intention to gradually increase the frequency of the pulses to 15-25 Hz. This may enhance tension generating capacity in the denervated knee extensor muscles and would allow the stimulated muscles to gradually produce tetanic contraction. It is recommended that the frequency of the pulses should not exceed 30 Hz to reduce the possibility of developing muscle fatigue (Gorgey et al., 2009). Direct muscle stimulation with the described parameters requires attention due to a risk of developing electrical burns as a result of high current density developed under the electrodes. Applications are commonly performed in prone position or in standing position in a standing frame or on a tilting table. It is recommended to stimulate the muscles for 30-60 minutes every day (Boncompagni et al., 2007; Gargiulo et al., 2011). In our laboratory, we have been successful in stimulating the denervated knee extensor in a seated position. The emphasis is to move the leg fully against gravity prior to load the muscles using standard ankle weights.
Summary and Conclusion
Denervation after SCI is a serious consequence that leads to extensive muscle atrophy. Skeletal muscle integrity is vital for the maintenance of cellular and whole-body metabolism. It is important to continue developing exercise interventions that benefit these individuals and decrease the risk for chronic diseases. LPWS is an emerging rehabilitation intervention technique which is used to stimulate denervated muscles. Parameters like pulse duration, frequency, and amplitude are altered in order to achieve muscle contractions. The excitability of denervated muscles is extremely low and hence, the pulse duration needs to be exponentially long to achieve desirable contraction. Muscle atrophy can be mitigated, and hypertrophy can be achieved in denervated muscles via LPWS and appropriate loading. The application may be feasible in clinical settings and may help reducing the associated healthcare costs. Future studies using LPWS are likely to maximize the rehabilitation potential for clinical care of LMN in persons with SCI.
Author contributions:Review of literature, writing the manuscript, revision of the manuscript: SC and JD; provided expertise on LPWS parameters and contributed to references: IB; wrote and provided expertise for EMG and denervated muscle fibrillation: GG; review of literature, supervision of manuscript, revision of paper and provide funding: ASG. All authors approved the final manuscript.
Conflicts of interest:The authors declare no conflicts of interest.
Financial support:None.
Copyright license agreement:The Copyright License Agreement has been signed by all authors before publication.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-Non-Commercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
- 中国神经再生研究(英文版)的其它文章
- LIM kinases in synaptic plasticity and their potential as therapeutic targets
- Increased thalamocortical connectivity from the affected thalamus to the unaffected hemisphere in a stroke patient
- Expression of long non-coding RNAs in complete transection spinal cord injury: a transcriptomic analysis
- Abnormal brain activity in adolescents with Internet addiction who attempt suicide: an assessment using functional magnetic resonance imaging
- Inhibition of BACE1, the β-secretase implicated in Alzheimer’s disease, by a chondroitin sulfate extract from Sardina pilchardus
- Neuroprotective effect of deferoxamine on erastininduced ferroptosis in primary cortical neurons