Characteristics of non-conveyance ambulance runs: A retrospective study in the Netherlands
Remco H.A. Ebben, Mariola Castelijns, Joost Frenken, Lilian C.M. Vloet,3
1 HAN University of Applied Sciences, Faculty of Health and Social Studies, Research Department of Emergency and Critical Care, Nijmegen, the Netherlands
2 Ambulance Service Brabant Zuid Oost, Eindhoven, the Netherlands
3 Radboud University Medical Center, Nijmegen, the Netherlands
Dear editor,
Emergency medical services (EMS) have developed from conveyance facilities into providers of advanced pre-hospital care.[1,2]Alongside this development there is a growing demand for EMS care, and the number of ambulance deployments is increasing.[3,4]Suggested reasons for this growing demand are changes in social support of people, accessibility of healthcare and social facilities, and the aging population.[4]However, not all patients who call for an ambulance and where an ambulance is dispatched are in need for conveyance to an emergency department, despite the acute nature of the healthcare problems of these patients.[5]A signif icant part of those patients are treated and left on-scene. Nonconveyance is an appropriate ambulance deployment where the patient after on-scene assessment and/or treatment does not require conveyance with medical personnel and equipment to a healthcare facility.[6]Non-conveyance can be initiated by the professional,the patient or through shared decision making.[7]Nonconveyance has an impact on ambulance availability and system efficiency, and the safety of non-conveyance is questioned.[8]
In 2015, the Netherlands counted 1,253,295 ambulance runs.[6]Of these, 255,471 (20.4%) ended up in nonconveyance. In literature, reported non-conveyance rates for general patient populations range from 10.7%-31.7%.[9-12]Although a signif icant number of patients were not conveyed, there is limited insight in characteristics of non-conveyance ambulance runs and non-conveyed patients. Previous research reported that 26% of the nonconveyance runs were dispatched by the EMS dispatch center with the most urgent dispatch code.[13]As for patient characteristics, 51.8% of the patients had complaints related to ICD-10 chapter 21 (factors influencing health status and contact with health services) and ICD-10 chapter 18 (symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified).[10]Other studies reported chief complaints related to trauma,neurology, general illness and psychiatry.[8,12]
Despite these studies, further insight in characteristics of non-conveyance ambulance runs is necessary.Therefore, the objective of this study was to describe characteristics of the runs, involved patients, and the care process of ambulance runs ending in nonconveyance.
METHODS
Design
This study had a retrospective, observational design.The study is reported using the STROBE-statement.[14]In concordance with Dutch legislation, no approval of a medical ethical committee was needed.
Setting
Ambulance care in the Netherlands is provided by 25 regional ambulance services (EMS), using ambulances or solo vehicles (car or motorcycle).[15]Ambulance care is dispatched through the emergency medical dispatch center, and can be requested via the national emergency number, or by another healthcare professional (such as the general practitioner). Dispatch interrogation is structured by the Advanced Medical Priority Dispatch System, digital variant Professional Quality Assurance(AMPDS/ProQA), or the Dutch Triage Standard.[16]After interrogation, ambulance care can be dispatched with urgency level A1 (arrival <15 minutes), A2 (arrival <30 minutes), and B (planned ambulance care). AMPDS/ProQA codes are therefore linked to response times. The dispatch center can dispatch a fully equipped ambulance or a solo vehicle. Ambulances are staffed with one driver and one registered ambulance nurse; a solo vehicle is staffed by one registered nurse, a nurse practitioner or physician assistant. Registered nurses become qualified as ambulance nurses after following a specific national training course. Ambulance nurses work autonomously and are allowed to make non-conveyance decisions using their national EMS protocol,[15]without direct consultation of an EMS physician.
Data collection and analysis
The study setting was located in one EMS region in the south-eastern part of the Netherlands. This EMS provides ambulance care for 750,000 people, and managed 50,252 ambulance runs in 2015.[6]This EMS uses the AMPDS/ProQA system. Each ambulance run is stored in a database and has an unique identification number. In 2015 the EMS had 35,207 ambulance runs with A1 or A2 urgency level at dispatch. We selected the ambulance runs, that had patient contact and (i) ended in non-conveyance, and (ii) where the ambulance was requested through the national emergency number, and(iii) where the ambulance runsheet had complete data.This automatically excluded ambulance runs without patient contact and cancelled ambulance runs. From the ambulance runs meeting our criteria, we randomly selected 500 ambulance runs for our sample. After anonymizing the ambulance runs in the sample we collected the characteristics of the run (urgency level,time of the ambulance run, geographical location), the patient (age, sex, social status), and the care process(EMS dispatch complaint, EMS dispatch code, initial onscene diagnosis, referral). Data from dispatch and from the actual ambulance run were linked by using the unique identif ication number. Descriptive statistics were used to analyze the data and the results with SPSS version 23.0.
RESULTS
About 31.2% (10,980/35,207) of the ambulance runs in 2015 ended up in non-conveyance. Of the 500/10.980 ambulance runs from which data was extracted, 74 were excluded as these patients were conveyed by another ambulance not included in our sample, leaving 426 ambulance runs of which 74.4% had A1 -urgency level.All ambulance runs included unique patients.
Table 1 and Figure 1 show the non-conveyance run characteristics. Most ambulance runs ending in nonconveyance were made during day time and evening time. Over half of these ambulance runs were made in urban areas. The percentage of non-conveyance across the year varies from 6.3% in September up to 12.0% in February. Non-conveyance runs were equally distributed across the week.
About 51.6% (220/426) of the patients were male,and the average age was 49.7 years (SD ±23.1). The age distribution is shown in Figure 2 and was equal among groups, although less non-conveyed patients were younger than 20 years.
The care process is displayed in Table 2. Common initial complaints during EMS dispatch interrogation of ambulance runs ending in non-conveyance were “loss of consciousness/fainting” (16.7%), “fall/fall of height”(12.7%), and “breathing problems” (9.4%). Common EMS dispatch codes were “possibly dangerous body area” (6.8%), “difficulty speaking between breaths”(5.4%), and “unconscious-effective breathing” (5.2%).“syncope” (9.9%), “psychiatric” (9.4%), and “panic attack” (8.9%) were the most common initial diagnosis of the ambulance nurses. In 46.7% (199/426) of the nonconveyance runs there was referral to other healthcare facilities (general practitioner, medical specialist or ED).

Table 1. Non-conveyance run characteristics (n=426)
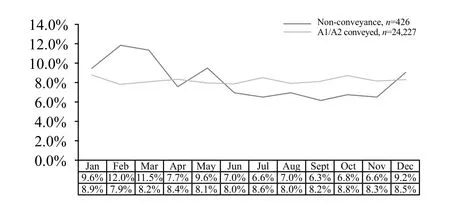
Figure 1. The characteristics of non-conveyance run.
DISCUSSION
This study describes the characteristics of ambulance runs that end in non-conveyance. In total, 31.2% of the ambulance runs with A1 or A2 urgency ended in nonconveyance. This percentage falls in the non-conveyance range of 3.7% up to 93.7% for general patient populations as described in literature.[17]Our results show that almost 75% of the ambulance runs in our sample was dispatched with the highest urgency level. Thispercentage is extremely high compared to literature,where high urgency dispatch codes represent 26% of the non-conveyance runs.[13]A possible explanation is that our sample consisted of ambulance runs dispatched with medium to high urgency levels, excluding planned ambulance runs. On the other hand, this percentage raises questions about the predictive value of EMD dispatch codes that are based on the callers’ information in relation to actual patient presentation and professional assessment on-scene. Unnecessary ambulance dispatch puts pressure on ambulance availability and might compromise patient and community safety. Therefore,the predictive value of EMS dispatch systems in relation to non-conveyance should be further investigated.Furthermore, non-conveyance runs in our sample are equally distributed across the week. This distribution is in line with all ambulance runs made in 2015 in the Netherlands.[6]Compared to literature,[8,12]our results show a comparable distribution of non-conveyance runs across daytime. The percentage of non-conveyance runs in urban areas is also comparable.[18]
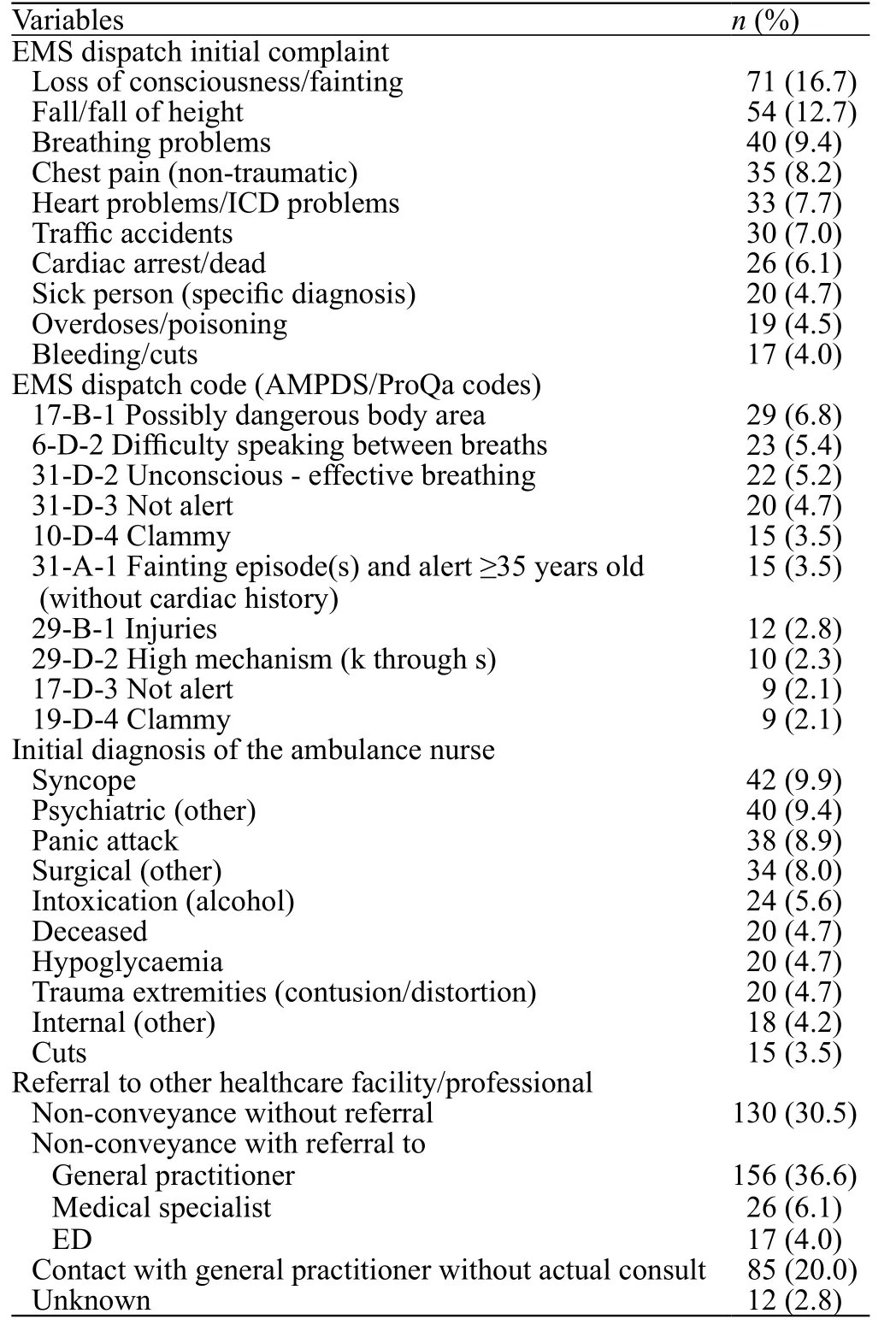
Table 2. Care process (top ten)

Figure 2. The age distribution (n=426).
Our results show that men and women are equally represented in the non-conveyance population. This is in line with literature.[13,18-20]As for age, our results show that non-conveyance occurs less frequently for patients aged below 20 years. Literature shows comparable non-conveyance rates for this age group.[21]Possible explanations might be that the Dutch national EMS protocol is more likely to advise to convey for younger children, that ambulance nurses are less willing to take risks with children and younger patients, or parental involvement during the conveyance decision-making process leading to higher conveyance rates. For all other age categories, non-conveyance rates are comparable,with the highest rate (15.3%) in the 50-59 years age group. One fourth of the non-conveyed patients were 70 years or older. We expected a higher percentage of older people as they have more comorbidities, and an increasing number of comorbidities is associated with an increase of (inappropriate) ambulance usage.[22]
Looking at the care process, during EMS dispatch there are a lot of initial patient complaints that are difficult to indicate, distinguish or triage based on the subjective information of the caller.[23]This indicates a need for on-scene assessment which justif ies the dispatch of an ambulance unit.
Looking at on-scene diagnosis from ambulance nurses in cases of non-conveyance, these patients had a variety of on-scene diagnosis. Common on-scene diagnosis were related to mental/psychiatric well-being and intoxication, both vulnerable patient populations.Literature shows contrasting percentages for these patient groups. For instance, a recent study shows that 12.5%of the non-conveyed patients had diagnosis related to psychiatry and alcohol abuse, although these patients were more left on scene in comparison to other patient groups.[24]On the other hand our results stand in contrast to a study that found that low-acuity patients with chief complaints related to psychiatry and toxicology were more likely to be transported by an ambulance to the ED.[25]This discrepancy indicates that patients with psychiatric conditions, and drug and alcohol misuse represent a difficult group for dispatch and ambulance professionals to correctly triage, treat and refer. These challenges are acknowledged in literature[1]and underline the need to develop protocols and alternative care pathways for vulnerable patient groups with psychiatric or intoxication problems. Furthermore, patients with syncope were well presented in the non-conveyance population. This is a difficult patient population as syncope can be part of serious or harmless medical conditions.[26]
Limitations
Firstly, although our study provided insight in the non-conveyance population, it did not look at patient outcomes, follow-up care, and re-contacts with the EMSsystem. Secondly, we did not compare non-conveyed with conveyed patients. Therefore, we do not know whether these two groups have different characteristics,complaints and outcomes, and this can be a direction for future research. Thirdly, this study had a small sample size with a single center character, and was conducted in the Netherlands with its own unique EMS system where referral to the ED, general practitioner or medical specialist is an option. This might limit generisability to other healthcare systems. Finally, we did not assess EMS dispatchers’ adherence to dispatch protocols.
CONCLUSIONS
This study shows a non-conveyance rate in a general patient population of 31.2%, meaning a significant part of all ambulance runs ended in non-conveyance. Men and women of all ages were equally represented within the non-conveyance population, although there were less younger children. Non-conveyance percentages varied throughout the year, but were equally distributed across days of the week and daytime. Non-conveyed patients called an ambulance with a variety of initial complaints,making triage difficult. Common on-scene diagnosis were related to syncope, psychiatry and alcohol abuse.Almost half of the non-conveyed patients were referred to another healthcare provider.
Funding:None
Ethical approval:Not needed.
Conf licts of interest:Authors have no f inancial or other conf licts of interest related to this submission.
Contributors:All authors proposed and conducted the study.RE wrote the first draft. All authors read and approved the final version of the paper.
 World journal of emergency medicine2019年4期
World journal of emergency medicine2019年4期
- World journal of emergency medicine的其它文章
- Ascending aortic dilatation rate after transcatheter aortic valve replacement in patients with bicuspid and tricuspid aortic stenosis: A multidetector computed tomography follow-up study
- Can emergency physicians perform extended compression ultrasound for the diagnosis of lower extremity deep vein thrombosis?
- Conf irmation of endotracheal tube placement using disposable f iberoptic bronchoscopy in the emergent setting
- Comparison between Emergency Severity Index and Heart Failure Triage Scale in heart failure patients: A randomized clinical trial
- A survey of ventilation strategies during cardiopulmonary resuscitation
- Empyema and mediastinal abscess in pyriform sinus f istula: A case report
