Empyema and mediastinal abscess in pyriform sinus f istula: A case report
Hai-jiang Zhou, Wen-peng Yin, Tian-fei Lan, Shu-bin Guo
1 Department of Emergency Medicine, Beijing Chao-yang Hospital, Capital Medical University, Beijing 100020, China
2 Department of Allergy, Beijing Shijitan Hospital, Capital Medical University, Beijing 100038, China
Dear editor,
Though notorious for its tendency to induce recurrent neck abscess, pyriform sinus fistula is of importance despite its rarity. It usually presents diagnostic and therapeutic challenges. Because of post-infectious f ibrosis, the embryologic origin of pyriform sinus f istula is diff icult to appreciate in certain cases. Here we present a case with empyema and mediastinal abscess caused by pyriform sinus f istula and share our experience in the treatment of this patient.
CASE
A 42-year-old male with an 8-year history of diabetes mellitus was admitted for a two-week history of fever, sore-throat, severe fatigure and malaise after catching cold. The highest temperature was 38.8 ℃. He had dysphagia with back pain and right chest pain. The symptoms were aggravated and a CT scan in the local hospital revealed pleural effusions. In order to get further treatment, he was transferred to our department.
The patient’s weight was 75 kg and he lost about 4 kg in the last two weeks. On examination, his heart rate was 98 beats/minute, respiratory rate 22 breaths/minute and blood pressure 142/70 mmHg. Oxygen saturation was 94% on room air. Examination of the oral cavity,neck and axillae was unremarkable. Chest examination revealed decreased air entry in the right lung and basal crackles in the left lung. Cardiovascular and abdominal examinations were normal.
Routine blood test showed white blood cell count of 14.56×109/L, hemoglobin level 145.0 g/L and platelet level 244×109/L. Arterial blood gas revealed pH 7.432, PO260.9 mmHg and PCO231.1 mmHg on room air. Blood biochemistry test revealed albumin level of 25.7 g/L and blood glucose level of 15.8 mmol/L.Procalcitonin was 2.18 ng/mL. Serum tumor markers revealed carbohydrate antigen 125 (CA125) 99.61 U/mL,ferritin (sFerr) 727.80 ng/mL, carcino-embryonic antigen(CEA) 0.83 ng/mL and neuron-specific enolase (NSE)16.76 ng/mL. High-resolution computed tomography demonstrated patchy blurred shadow in the right lung,which was suggestive of pneumonia. The patient was treated empirically with amoxicillin sodium and sulbactam sodium for injection. Lung enhanced CT scan revealed pericardial effusions and encapsulated pleural effusions in the right thoracic cavity and in the mediastinum (Figure 1). Thoracentesis was performed and 1,000 mL coffee-colored pleural effusion was drained. Follow-up pleural effusion analysis revealed Rivalta test ++++, total cellular count of 246,141/μL and total white blood cell count of 125,141/μL. Bacterial culture revealed streptococcus dysgalactiae equisimilis.
After 5 days of antimicrobial treatment, the patient did not improve and was transferred to the thoracic surgery department for a presumed tracheoesophageal fistula. No obvious abnormality was found in preoperative laryngoscopy and f lexible bronchoscopy examination. Video-assisted thoracoscopic surgery for empyema exenteration revealed coffee-colored pus in the thoracic cavity and within the mediastinum (Figure 2). Thoracic cavity drainage tube was placed and iodine water was found leaking from the mouth of the patient when performing post-operative thoracic lavage,suggesting fistula formation. Nasogastric tube was then placed and enteral nutrition was given. Esophagram with Barium swallow demonstrated contrast agent leaking into the trachea (Figure 3). Follow-up examination of f lexible gastroscopy (10 mm) revealed an opening about 1 cm in diameter in the sinus posterior wall, through which we could get access into the thoracic cavity (Figure 4). The diagnosis of right pyriform sinus fistula was made and percutaneous endoscopic gastrostomy was performed.The patient received intravenous antimicrobial therapy and enteral nutrition treatment without surgery.Fortunately, he was discharged successfully and regular follow-up was performed in the out-patient department. He recovered well and percutaneous enteral nutrition tube was successfully removed one month later. Re-examination of gastroscopy revealed complete closure of the fistula without recurrence. The patient is now undergoing regular follow-up in the outpatient department.
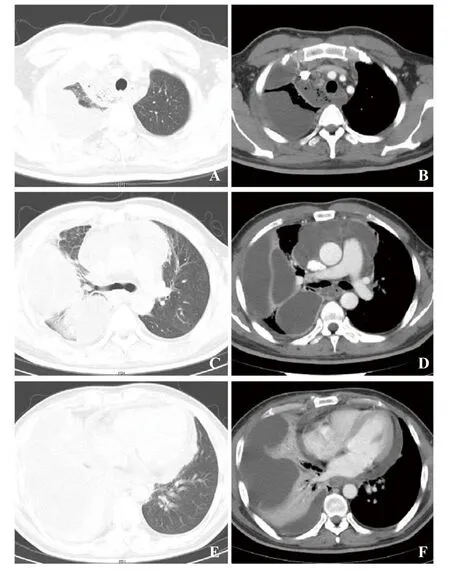
Figure 1. Enhanced CT scan of the lung revealed pericardial effusion and encapsulated pleural effusion in the right thoracic cavity and in the mediastinum.
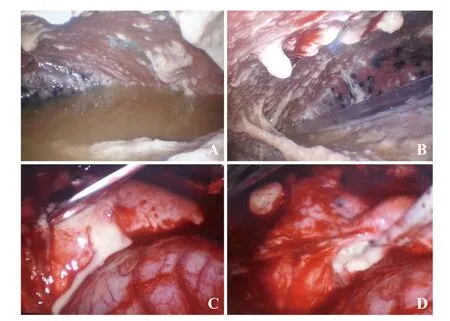
Figure 2. Video-assisted thoracoscopic surgey for empyema exenteration revealed coffee-colored pus in the thoracic cavity (A, B) and within the mediastinum (C, D).
DISCUSSION

Figure 3. Esophagram with Barium swallow demonstrated contrast agent leaking into the trachea (arrow).

Figure 4. Painless gastroscopy examination revealed an opening about 1 cm in diameter in the sinus posterior wall (B), through which we could get access into the thoracic cavity (C, D).
The pyriform sinus is a true space bordered by the laryngeal cartilage and the hypopharynx.[1]Pyriform sinus fistula, first reported by Sandborn and Shafer in 1972 and represented by malformation of the third or fourth branchial pouch, is a rare congenital anomaly that originates from the pyriform sinus.[2]It usually penetrates the cricothyroid muscle and then ends in the left lobe of the thyroid gland or thereabouts.[3]Due to the similarity in their course, distinguising between third and fourth branchial pouch f istulas is diff icult on clinical ground alone.[4]The key difference between the two is the relationship to the superior and recurrent laryngeal nerves.[5]The third branchial fistula passes superficial to both superior and recurrent laryngeal nerves, while the fourth branchial fistula passes deep to the superior laryngeal nerve but superf icial to the recurrent laryngeal nerve.[5]Left-sided f istula is more common and the leftneck-sided predominance is possibly due to suppressed embryogenesis of the ultimobranchial body on the right side and asymmetry of transformation of the fourth branchial arch.[5]The sinus tract acts as the pathway for the infection spreading. In certain cases, the embryologic origin of the pyriform sinus is diff icult to appreciate due to postinfectious f ibrosis.
Pyriform sinus fistula presents diagnostic and management challenge and misdiagnosis exposes patients to the risk of repeated infection and inadequate management.[6]A majority of patients have their onset in infancy or childhood without gender predominance.The formation of pyriform sinus fistula is a chronic inflammatory process involving the thyroid gland and the surrounding tissues.[6]The most common symptoms include recurrent cervical suppurative infections or neck abscesses. Children with pyriform sinus fistula often present with acute suppurative thyroiditis. Diagnosis of pyriform sinus f istula should be considered in any child or young adult with recurrent lateral cervical abscess. All suspected patients with neck/thyroid infection or mass should undergo further examinations.
Diagnostic procedures encompass ultrasound,computed tomography (CT), magnetic resonance imaging (MRI), barium swallow esophagography,and laryngoscopy. Among them, barium swallow esophagography is taken as the golden standard with a high rate of success. Ultrasonography can be used repeatedly to demonstrate the inf lammatory process with the advantages of non-invasiveness and no radiation.[7]The echogenic tract in the follow-up ultrasound examination is highly suggestive of a pyriform sinus-thyroid fistula and is helpful for the diagnosis. Ultrasound is also helpful in demonstrating the relationship of the mass with thyroid and the presence of gas within the lesion.[7]CT is a useful examination to rule out other lateral cervical diseases and to determine the direction of the fistulectomy.Performing a CT scan immediately after barium swallow may increase the sensitivity of the scan by highlighting the sinus tract. CT is superior to MRI in detecting air density in the sinus or f istulous tracts as well as depicting thyroid involvement. Nasal fiberoptic endoscopy usually revealed a f istulous opening in the hypopharynx.Conf irming the internal orif ice of the f istula and injecting pigment such as blue dye is a useful method for detecting the f istula tract during surgery.[8]
Treatment is variable and surgical excision is considered definitive therapy and should be proceeded by administration of appropriate antibiotics to allow regression of inflammation.[9]Resection of fistula and appropriate ligation is of vital significance to prevent recurrence. Chemocauterization of the internal opening is alternative treatment that is less invasive and does not leave a cutaneous scar, but its recurrent rate is higher than complete resection.[10]However, although complete resection is deemed as the best method for treating a pyriform sinus fistula, complete resection of the whole tract is diff icult, because recurrent infection and previous surgery usually make complete resection of the tract hazardous. Pyriform sinus fistula must be considered when encountering patients with cervical abscess, in rare cases, emphysema or mediastinal abscess.
CONCLUSION
Pyriform sinus fistula is a rare congenital anomaly that originates from the pyriform sinus due to failure of complete obliteration of the third or fourth branchial pouch. It presents diagnostic and management challenge to physicians. Diagnosis of pyriform sinus fistula should be considered in any child or young adult with recurrent lateral cervical abscess and suspected cases should undergo barium swallow esophagography and CT scanning. Treatment varies and surgical excision is deemed as def initive therapy and should be proceeded by administration of appropriate antibiotics. Physicians in emergency department should enhance their awareness when encountering patients with cervical abscess.
Funding:None.
Ethical approval:Not needed.
Conflict of interest:The authors declare that they have no conf licts of interest.
Contributors:HJZ and WPY contributed equally to this study. All authors have substantial contributions to the acquisition, analysis,or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; and f inal approval of the version to be published.
 World journal of emergency medicine2019年4期
World journal of emergency medicine2019年4期
- World journal of emergency medicine的其它文章
- Information for Readers
- The utility of point-of-care ultrasound in the assessment of volume status in acute and critically ill patients
- Application of 4% formaldehyde under electronic colonoscope as a minimally invasive treatment of chronic hemorrhagic radiation proctitis
- Instructions for Authors
- My mother is looking blue
- Continuous B scan ultrasound guided post-traumatic sub-periosteal orbital hematoma drainage: An advantage over routine needle drainage procedure
