Continuous B scan ultrasound guided post-traumatic sub-periosteal orbital hematoma drainage: An advantage over routine needle drainage procedure
Dr. Rajendra Prasad Centre for Ophthalmic Sciences, All India Institute of Medical Sciences, New Delhi 110029, India
Dear editor,
Traumatic orbital haemorrhage is an unfortunate complication with potential vision-threatening consequences.[1-3]The collection of blood can occur anywhere along the potential free orbital spaces,[4]but the subperiosteal collection of the blood is an important clinical variant where careful and timely intervention can give commendable rewards to the surgeon as well as to the patient.[1,2]Subperiosteal hematoma could be traumatic or non-traumatic, in turns, the non-traumatic cases may be due to bleeding tendency as in cases of leukaemia, blood dyscrasia and haemophilia or could be due to vascular malformation, venous congestion,infection, inflammation and neoplastic and nonneoplastic causes.[4]Here in this report, we elaborate the advantage of continuous ultrasound-guided needle drainage of the post-traumatic subperiosteal hematoma to enhance the clinical accuracy and to avoid the untoward complications.
CASE
A 15-year-old male patient was rushed to ocular emergency with a history of rapidly progressive leftsided proptosis and inferior dystopia following blunt trauma to the left forehead region (Figure 1). The patient sustained blunt trauma to his left side of the forehead while playing with other kids (he accidentally fell on the f loor with the left-sided forehead as the f irst contact point). The duration was around twelve hours from the time of trauma to first clinical examination. On examination, visual acuity was 20/20 in the right eye and 20/40 in the left eye. Rest of the ocular examination was essentially within normal limits in the right eye, whereas left eye showed severe restriction in the extraocular motility. Left forehead had small abrasions over the tense and stretched upper eyelid, the globe was inferiorly dystopic (around 5 millimetres) with mild conjunctival chemosis, however, the cornea and anterior chamber were within normal limits. Intraocular pressures were 15 mmHg in the right eye and 30 mmHg in the left eye and left fundus was normal. The left upper eyelid was minimally mobile, thus, preventing the corneal exposure with added lubricating gel and eye patching.
Immediately B scan ultrasonography of the orbit was considered. The patient was made to lie down in a comfortable supine position, and the orbit was screened by placing the probe along all four longitudinal planes.The inferior longitudinal view directed along the superior orbit revealed a large biconvex hypoechoic space with mild to moderate amplitude internal contents underneath the roof of orbit, suggestive of probable subperiosteal blood collection (Figure 2A). Further characterization of the lesion was considered with a non-contrast computed tomography (NCCT) of the orbit and brain. The imaging revealed a well defined biconvex hypodense area along the roof of orbit in absence of any bony discontinuity or any other associated intracranial pathology. Thus, based on these clinical and radiological f indings a diagnosis of post-traumatic subperiosteal hematoma was confirmed and immediate needle drainage was planned.
After application of topical skin numbing anaesthetic gel over the upper eyelid for 10 minutes, good surface anaesthesia was achieved. Again with the help of B scan ultrasonography the anatomical extents of the hematoma were once again confirmed. Now the B scan probe was placed along the inferior longitudinal plane and the cavity was continuously imaged. Another individual introduced a 22 gauze, 1.5 needle with a 10 mL syringe along the superior orbital margin after making the space between the globe and the superior orbital rim by insinuating a f inger. As the needle was negotiated easily along the soft tissue planes, the needle entry into the cavity was observed and confirmed (Figure 3A, yellow arrow). Under the constant guidance of ultrasonography,complete drainage was performed (Figure 3B) which in turn was indicated by a gradual reduction in the size of the cavity. The dystopia reduced immediately (Figure 3C)and the patient experienced prompt symptomatic relief.Postoperatively patient was advised with oral antibiotics,steroids and anti-inflammatory medications for a week.At the end of one week, the extraocular motilities were full with a functional upper eyelid. Immediately following drainage, the dystopia was completely reduced with the globe in actual anatomical position (Figure 4).
DISCUSSION
Post-traumatic subperiosteal hematomas are rarely encountered in ocular emergencies; even then it is important for an ophthalmologist to be fully aware of the clinical scenario. Following blunt trauma to the forehead,the fragile vessels along the loosely adherent periosteum to the frontal bone may bleed easily, leading to a rapid collection of blood along this potential space.[1-3,5]This clinical scenario is mainly seen in second-decade male individuals, who are continuously involved in outdoor activities. However, there are reports in female patients and other age groups as well.[2,6-8]

Figure 1. Clinical prof ile at the time of presentation showing a leftsided inferior globe dystopia with proptosis.
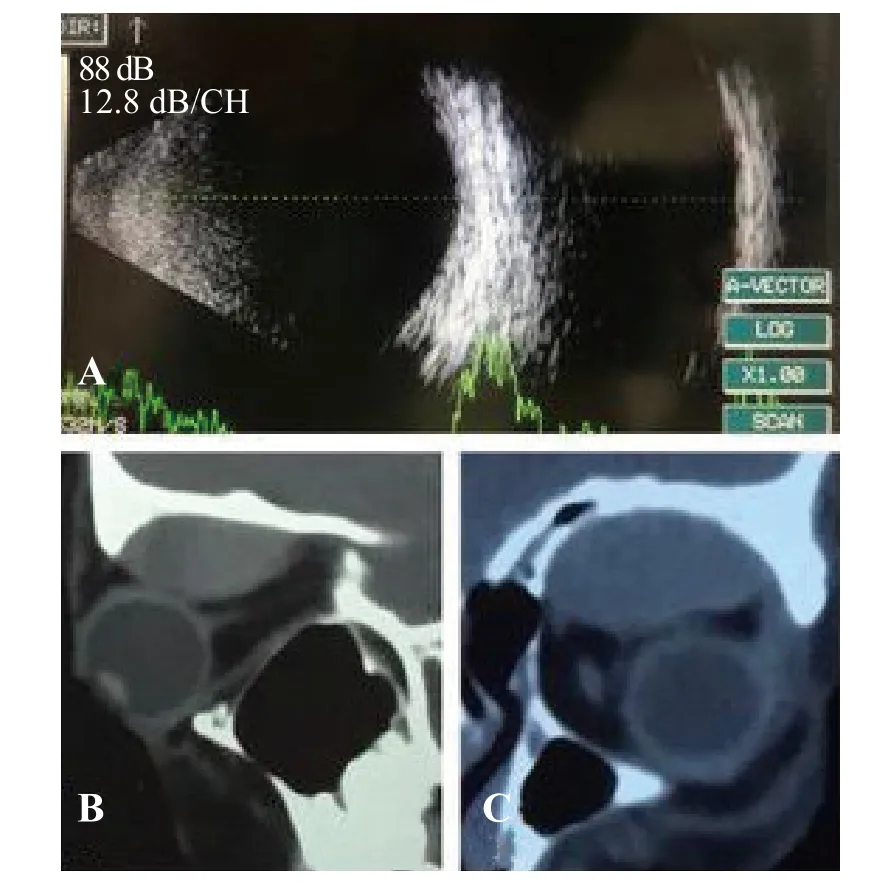
Figure 2. B scan ultrasonography of the orbit. A: B scan ultrasonography showing a well defined biconvex cystic space between the frontal bone and the globe; B, C: saggital and coronal sections of the NCCT conf irming a subperiosteal collection along the superior orbit.
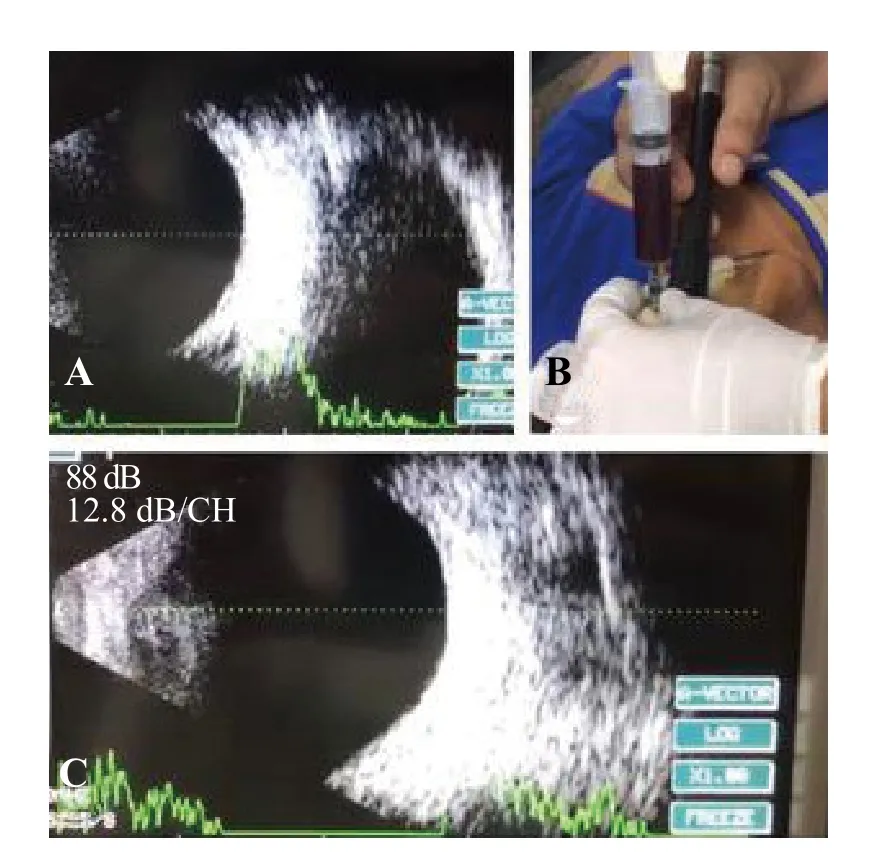
Figure 3. B scan ultrasound-guided drainage. A: while performing B scan ultrasound-guided drainage, the needle tract was evident along the superior aspect of the cystic cavity (yellow arrow); B: the blood was evacuated completely with the needle in situ and the ultrasound probe along the lower orbital margin; C: following the evacuation, there was a drastic reduction in the size of the cystic cavity with the needle in situ.
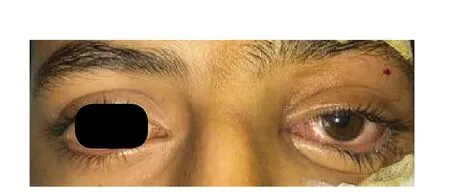
Figure 4. Immediately following drainage, the dystopia was completely reduced with the globe in actual anatomical position.
Usual clinical features include rapidly progressive proptosis (globe dystopia as well), excruciating pain,diplopia and restricted extra-ocular motility.[1-5]The collected hematoma can be managed in different ways depending upon the size, extent and associated complications. Small subperiosteal collection or the less symptomatic hematomas can be observed with oral broad-spectrum antibiotics and steroids. Secondly, in cases of moderate to a severe collection with rapidly deteriorating proptosis having vision endangering consequences, immediate needle drainage can be performed.[5,6,7,9]Thirdly, if there is associated intracranial hematoma or other faciomaxillary complications then a combined approach from multi speciality is necessary.[2,7,8]Chelnis et al[5]discussed simple officebased needle drainage procedure in a case of idiopathic orbital hematoma, and they achieved successful results in the immediate period. In addition, the air in the orbit following trauma needs to be differentiated from blood in the subperiosteal plane. Following the breach in orbital walls, a sudden proptosis can appear following a rigorous Valsalva manoeuvre. These patients may possess crepitation on palpation and added computed tomography will delineate the entrapped air along the orbital spaces.Therefore, differentiation of these conditions is necessary for management as well as for prognostication.[10,11]
However, as we are aware, B scan ultrasonography is an indispensable tool for a quick and accurate diagnosis of various orbital and posterior segment diseases,[12]addition of continuous B scan guided imaging while draining subperiosteal hematomas will provide a realtime information of the needle track, its direction and the changes along the cavity throughout the observation.In addition to this, the other unique advantage of this technique is to avoid any inadvertent globe perforation and subsequent vision-threatening complications. .
CONCLUSION
To conclude, while draining subperiosteal hematomas in emergency settings, an ultrasound-guided approach can be followed for better anatomical and visual outcomes.
Funding:None.
Ethics approval:Not needed.
Conf licts of interest:The authors have no conf lict of interest, no f inancial issues to disclose.
Contributors:All authors have substantial contributions to the acquisition, analysis, or interpretation of data for the work;drafting the work or revising it critically for important intellectual content; and f inal approval of the version to be published.
 World journal of emergency medicine2019年4期
World journal of emergency medicine2019年4期
- World journal of emergency medicine的其它文章
- Information for Readers
- The utility of point-of-care ultrasound in the assessment of volume status in acute and critically ill patients
- Application of 4% formaldehyde under electronic colonoscope as a minimally invasive treatment of chronic hemorrhagic radiation proctitis
- Instructions for Authors
- My mother is looking blue
- Empyema and mediastinal abscess in pyriform sinus f istula: A case report
