Conf irmation of endotracheal tube placement using disposable f iberoptic bronchoscopy in the emergent setting
Avir Mitra, Asaf Gave, Kelsey Coolahan, Thomas Nguyen
1 Department of Emergency Medicine, Mount Sinai Beth Israel, Icahn School of Medicine, New Jersey 08043, USA
2 Department of Surgery Critical Care, Mount Sinai Beth Israel, Icahn School of Medicine, New York 10009, USA
KEY WORDS: Airway; Simulation; Bronchoscopy; Tube conf irmation
INTRODUCTION
Prehospital intubation of critically ill patients or patients in cardiac arrest is an indispensable component of emergent care. Despite its necessity in certain patients,intubation in the field is fraught with complexities inherent to the prehospital setting. Patients often present in extremis, emergency medical service responders may have less experience with intubation and intubations often occur in poorly controlled environments in which there may not be adequate lighting, monitoring, access or assistance. All of these factors ultimately serve to make outcomes less predictable.[1-3]Despite all precautions and adequate technique, endotracheal (ET) tubes can easily be mistakenly placed in the esophagus or the right mainstem bronchus.
For these reasons it is of utmost importance that any patient who has been intubated in the f ield receive a quick but thorough conf irmation of tube placement upon arrival in the emergency department. The clinical policy statement from the American College of Emergency Physicians (ACEP) details several common strategies for ET tube confirmation in emergency departments.[4]The gold standard is direct visualization of the tube passing the vocal cords, but technical approach is not specified.Anatomic visualization requires techniques such as direct laryngoscopy or video laryngoscopy. However, the f ield is commonly obscured by vomitus, blood, sputum, or tissue,which is often more profuse given the manipulation that occurred in the f ield. Also, attempts to visualize the tube can theoretically dislodge or affect positioning of the tube in a way that causes the airway to be lost. In addition,ongoing cardiopulmonary resuscitation (CPR) makes blade positioning and adequate exposure diff icult at best.C-spine precautions, which may also be present in these patients, can make visualization diff icult as well.
Of available adjunct approaches (auscultation for bilateral breath sounds, visualization of symmetric chest rise, chest X-ray, pulse oximetry, capnography, etc.),capnography offers especially useful evidence when determining proper ET tube placement.[5,6]However,while capnography proves to be highly sensitive and specif ic for conf irming ET tube placement in patients with adequate tissue perfusion, results may be unpredictable in the setting of poor tissue perfusion such as during cardiac arrest.[4,7-15]Despite its utility, capnography does not provide direct visualization; therefore, it is important to evaluate other available methods of confirmation,particularly those that rely on direct visualization.
With that said, evaluation of f iberoptic bronchoscopy for ET tube placement confirmation in the emergent setting is warranted. We acknowledge that capnography is often more readily available, but believe fiberoptic bronchoscopy may offer several benefits as it becomes more ubiquitous in the emergency department. Direct visualization methods offer the benefit of a more nuanced assessment by allowing the user to distinguish mainstem from tracheal placement. In addition, the suction capability within the bronchoscope would allow providers to simultaneously clear the tube of fluid or debris should any be found. Laryngoscopy offers similar benefits but requires significant airway manipulation which may make visualization diff icult, as described above.
The goal of our study is to assess the effectiveness,ease and speed with which ET tube placement can be confirmed by emergency medicine providers using a disposable f iberoptic bronchoscope having had minimal training with its use. We hypothesize that this approach can be a viable alternative for quick, reliable and direct visualization of ET tube placement.
METHODS
Study setting and population
In order to study this approach, we recruited emergency medicine residents at a busy, three-year residency program who had limited to no experience with bronchoscopy. We recruited 7 postgraduate year 1 (PGY1), 8 postgraduate year 2 (PGY2), and 8 postgraduate year 3 (PGY3) emergency medicine residents for a total of 23 residents. Residents were recruited at the end of their respective years based on interest and availability out of a pool of 43 potential residents. Residents were chosen to evaluate for diff iculty of technique, given their relative lack of prior experience with this technique. Furthermore, in most academic settings, residents are performing the majority of the procedures in the department. Trials were conducted between May to August of 2017. An IRB exemption was granted by the IRB board for this study.
Study protocol and design
Each resident was provided with approximately 5 minutes of active teaching and practice with the bronchoscope on a simulated patient mannequin (Sim Man 3G, Laerdal Medical), supine, in a natural anatomic position. A session duration of 5 minutes proved to be sufficient time for developing familiarity with the equipment. In that time, residents viewed the trachea,the bronchi and the esophagus of the SIM patient. They were shown that the trachea could be identified by tracheal rings and visualization of a carina; the mainstem could be identified by tracheal rings, an increasingly tight bronchial passage and absent carinal views;the esophagus could be identified by lack of tracheal rings, a collapsing esophageal structure and eventual presence of gastrum. During the session, the resident was stationed at the head of the bed with an Ambu aScope(Ambu A-scope 4 Broncho Regular 5.0/2.2, Columbia,MD) which is a disposable, sterile single-use flexible intubation scope that interfaces with a separate monitor for easy visualization. Each resident was then surveyed on prior experience with bronchoscopy.
After this, the resident was instructed to leave the room and the researcher placed the ET tube in either the trachea, the esophagus or the mainstem at random in the same SIM patient. Left mainstem was not included as right mainstem is a more commonly encountered clinical scenario. ET tube placement was randomized using an online random number generator prior to placement.Residents returned to the room and were told that the tube was in one of the three potential positions. They were asked to identify where the tube was placed using the bronchoscope alone. To do this, the resident placed the bronchoscope in the ET tube and visualized the inside of the tube on the screen as they threaded it toward the distal end of the tube. When the bronchoscope emerged from the distal end, residents attempted to identify the anatomy and thereby determine tube placement.
Measurements
Each resident underwent four trials with the tube position being changed at random between each trial and no feedback being given between attempts, resulting in a total of 92 data points (23×4). Residents did not adjust the tube position in any way and were only asked to identify placement.
We assessed their accuracy in identification of tube position (trachea vs. right mainstem vs. esophagus)and their time-to-guess in seconds for each trial. Timeto-guess was defined as the interval between initiation of bronchoscope insertion and reported guess of ET tube placement. After the four trials, we surveyed them regarding their perceived difficulty or ease of the bronchoscopic approach (on a 1-5 scale with 1 being very easy, 2 being somewhat easy, 3 being neutral, 4 being somewhat diff icult and 5 being very diff icult).
Data analysis
This data was compiled and parsed in order to give us an overall accuracy rate, an average time and an overall average level of comfort by novice providers.
RESULTS
Of the 23 residents, only 1 had used a bronchoscope in the past, and in that case only briefly on two prior occasions. All other residents had never used a bronchoscope. Despite minimal prior experience and just f ive minutes of training, residents were able to accurately identify the exact location of the ET tube in 88 out of 92 trials (95.7%) using the bronchoscopic approach. The median time-to-guess was 7.0 seconds, IQR (5.0-10.0).Time distributions among the participants are displayed in Figure 1. The average comfort amongst the residents was 1.6 on a scale from 1-5, with 1 being very easy, 2 being somewhat easy, 3 being neutral, 4 being somewhat diff icult and 5 being very diff icult. No residents found the approach to be somewhat or very diff icult. There were no complications, no instances of tube or scope damage, no damage to any anatomic structures on the SIM patient,and no instances in which the tube was displaced.
Failures were defined as incorrectly reported placement. A total of 4 out of the total 92 trials were incorrectly identified. All 4 failed identifications happened to be placed in the right mainstem and incorrectly identified as either esophageal (50%) or tracheal (50%). Of note, all actual esophageal placements were correctly identif ied.
DISCUSSION
Confirming a secure airway in a timely manner is critical in situations where prehospital intubation has occurred by paramedics with varying levels of experience. This study was based on the hypothesis that a f iberoptic bronchoscope threaded through a previously placed endotracheal tube enables physicians to quickly and easily assess endotracheal tube position.
The use of fiberoptic bronchoscopy in the emergent setting has been discussed and studied, but its use has thus far been limited in the emergency department.[16,17]Certainly,trials and studies regarding “awake intubations” or fiberoptic-assisted intubations have shown promising results.[18,19]However, little literature is present regarding the use of fiberoptic bronchoscopy for confirmation of an already placed endotracheal tube. Budde et al[20]and Hollingsworth et al[21]both reported successful use of f iberoptic bronchoscopy to conduct tube exchange from laryngeal mask airway to ET tube, which at least in theory requires bronchoscopic conf irmation of the initial tube placement. Craske et al[22]describes bronchoscopy in confirmation of a tracheostomy tube in which they thread the bronchoscopy through the tracheostomy tube in order to confirm placement. A similar approach of threading the bronchoscope through the tube is also considered the gold standard in confirmation of double lumen endotracheal tubes used by thoracic surgeons in single lung ventilation.[23,24]
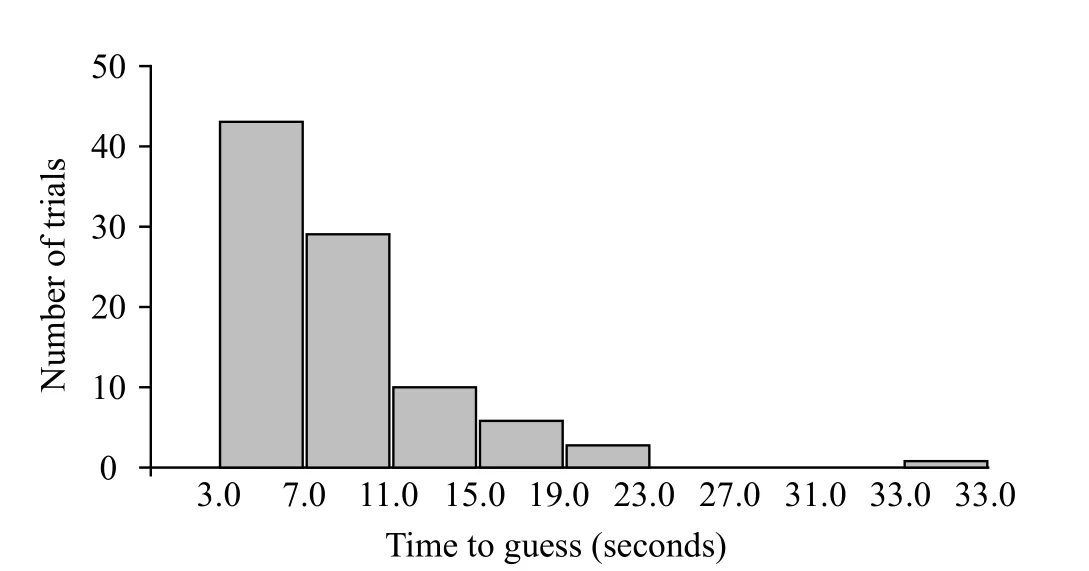
Figure 1. Time distributions among the participants.
Adjunct approaches such as listening for bilateral breath sounds are useful but challenging in the loud, chaotic initial stages of patient arrival, and are made much more difficult by active compressions. Likewise, chest X-ray,pulse oximetry, fogging of the ET tube and visualization of chest rise provide useful data, but are “not sufficiently reliable to confirm endotracheal tube placement”,according to current policy standards.[4]Ultrasound of the trachea has more recently been proposed as an alternative method for ET tube confirmation, with mostly positive outcomes. The approach, however, does not provide direct visualization but instead uses artifactual ultrasound findings to confirm placement.[25,26]The speed of this approach can also be hindered by the inherent space and time required to set up and use the ultrasound device. As discussed earlier, capnography is exceptionally useful in situations where adequate tissue perfusion is present.However, it does not offer direct visualization and may be unpredictable in situations where tissue perfusion is compromised.
We believe our data, although not directly compared to adjunct methods above, strongly support our hypothesis that fiberoptic bronchoscopy as described herein allows for a quick and accurate method for directly determining ET tube placement. Theoretically, it also offers the added benef it of suctioning secretions, blood or small foreign bodies that may be lodged in the tube at the same time. While there is no established gold standard for ET tube confirmation in the emergent setting, and no established rates of accuracy for the various current practices, our study found a 95.7% accuracy rate with this approach. Furthermore, all esophageal placements were correctly identif ied.
It is important to note two potential logistical disadvantages of the bronchoscopic approach. Timeto-guess reported in this study did not include time required to access or setup the equipment. Depending on such logistics such as storage, access and/or technical diff iculties, setup time could prolong total time required to confirm ET tube placement. However, strategies to optimize access and setup could easily be implemented such that additional time required would be negligible.In regards to set up, the ET tube must be disconnected from the ambu bag or ventilator while bronchoscopy is being performed. We found that the median time to an assessment was 7.0 seconds, IQR (5.0-10.0); in our clinical experience, an apneic time of 7.0 seconds is acceptable in the emergent setting, and with more practice, providers will likely decrease the time taken.Apneic pauses of these lengths are common during suctioning, transfer and other times during emergent care. Again, using the bronchoscope with its incorporated suctioning ability allows the advantage of providing inline suction and ET tube clearance during this period.
In addition to speed and accuracy, it is important that emergency providers feel comfortable using a new piece of equipment and a new approach. We showed that most residents found using a bronchoscope in the manner described to be “very easy” or “somewhat easy”, and no residents found the approach to be “somewhat diff icult”or “very difficult”. The average comfort level comfort was between “very” and “somewhat” easy. Moreover,this was after no more than 5 minutes of practice, with all but one of our 23 residents never having used a bronchoscope before. Our data lend support to the notion that even with minimal practice and in the hands of relative novices, our approach to ET tube conf irmation is intuitive and requires little procedural skill or experience with bronchoscopy.
Limitations
This study suffers from several limitations. The size of the study was small as it was limited to 23 residents performing 92 trials. Future studies involving more participants as well as more experienced physicians are warranted. Additionally, this study does not compare accuracy or speed with some of the more common approaches to ET tube conf irmation such as glidescope,direct laryngoscopy, listening for breath sounds or capnography. The purpose of this study however was rather to simply establish feasibility of a previously unstudied approach for tube confirmation. Our goal was to determine if Emergency Medicine residents who are relatively new to bronchoscopy could in fact utilize this approach with any degree of accuracy, and if so whether it could be done in an acceptably quick speed. We believe our data indicate that this heretofore unstudied approach is in fact feasible for emergency medicine providers and therefore further head to head studies comparing our bronchoscopic approach with other approaches are warranted.
A second limitation was use of a SIM patient rather than real patients. SIM anatomy attempts to recreate real anatomy but certainly does not contain the variation with which real patients present. Real patients are often moving or being moved, and real situations are more stressful and chaotic than those we create in the SIM lab.In addition, SIM anatomy is relatively pristine compared to real patients who often have copious secretions, f luid,blood or vomitus in the airway, thereby making anatomic identif ication more challenging. While we acknowledge these limitations, issues of consent with patients in acute decompensated states made working with a SIM patient more practical for an initial study on an unvalidated procedural approach. Future studies involving real patients who have been intubated in the prehospital setting are warranted.
CONCLUSIONS
The utility of fiberoptic flexible bronchoscopy in intubations has been well studied; its efficacy in conf irmation of already placed endotracheal tubes has yet to be assessed. Our study demonstrates that disposable fiberoptic bronchoscopy can be an accurate, quick and relatively easy approach to ET tube confirmation, even when utilized by providers who are early in their training and have little to no prior experience with bronchoscopy.We therefore encourage more study into a bronchoscopic approach to ET tube conf irmation as another feasible and legitimate option amongst the various options currently available to emergency physicians.
Funding:None.
Ethical approval:Not needed.
Conflicts of interest:The authors have no competing interests relevant to the present study.
Contributors:AM proposed and wrote the paper. All authors edited the f inal version of the paper.
 World journal of emergency medicine2019年4期
World journal of emergency medicine2019年4期
- World journal of emergency medicine的其它文章
- Ascending aortic dilatation rate after transcatheter aortic valve replacement in patients with bicuspid and tricuspid aortic stenosis: A multidetector computed tomography follow-up study
- Can emergency physicians perform extended compression ultrasound for the diagnosis of lower extremity deep vein thrombosis?
- Comparison between Emergency Severity Index and Heart Failure Triage Scale in heart failure patients: A randomized clinical trial
- A survey of ventilation strategies during cardiopulmonary resuscitation
- Characteristics of non-conveyance ambulance runs: A retrospective study in the Netherlands
- Empyema and mediastinal abscess in pyriform sinus f istula: A case report
