Ascending aortic dilatation rate after transcatheter aortic valve replacement in patients with bicuspid and tricuspid aortic stenosis: A multidetector computed tomography follow-up study
Yu-xin He, Jia-qi Fan, Qi-feng Zhu, Qi-jing Zhou, Ju-bo Jiang, Li-han Wang, Stella Ng, Xian-bao Liu,Jian-an Wang
1 Department of Cardiology, the Second Aff iliated Hospital, Zhejiang University School of Medicine, Hangzhou 310009,China
2 Department of Radiology, the Second Aff iliated Hospital, Zhejiang University School of Medicine, Hangzhou 310009,China
KEY WORDS: Transcatheter aortic valve replacement; Aortic dilatation; Bicuspid aortic valve
INTRODUCTION
After a fast development, transcatheter aortic valve replacement (TAVR) has become a safe and effective alternative to surgical aortic valve replacement (SAVR)for symptomatic severe aortic stenosis (AS) patients with increased surgical risks.[1,2]However, the indication of TAVR for bicuspid AS is still controversial.[2,3]Nevertheless, satisfactory results are accumulating regarding patients with bicuspid aortic valve (BAV)undergoing TAVR.[4,5]Comparable outcomes have been achieved in BAV patients versus tricuspid aortic valve(TAV) patients, especially with new-generation devices.[5,6]
Given the fact that aortic dilatation is seen more commonly in patients with bicuspid AS,[7]and as TAVR does not provide simultaneous ascending aortic intervention, a concern arises about progressive aortic dilatation in patients with bicuspid AS after TAVR. A series of studies about aortic dilatation after SAVR were reported, but the results were conflicting.[8-10]Limited data suggested that ascending aortic size remained stable after TAVR in TAV patients with mild and moderate dilatation.[11]Data regarding aortic dilatation in BAV patients after TAVR is scarce, especially with midterm to long-term follow-ups. Currently, the development and progression of aortic dilatation in bicuspid patients are believed to be affected by both genetic and hemodynamic factors.[12-16]With abnormal hemodynamics being corrected by TAVR in bicuspid AS patients, whether the progression of aortic dilatation will be decelerated or not is unclear.
This study aims to assess the ascending aortic dilatation rate (mm/year) after TAVR in patients with BAV versus TAV using a multidetector computed tomography (MDCT) follow-up and to determine the predictors of ascending aortic dilatation rate.
METHODS
Study population
Patients undergoing TAVR for symptomatic severe AS were all prospectively included in our single-center TAVR cohort. Those undergoing TAVR from March 2013 to March 2018 were included in this study. Those without MDCT follow-ups or with poor MDCT image quality were excluded. The decision for the TAVR procedure for each patient was carefully evaluated by the dedicated heart team of our hospital. The ethics committee of our center approved the study protocol and written informed consents were obtained in all patients. Patient characteristics,clinical data, transthoracic echocardiography (TTE)measurements, procedural variables, and regular followup data were prospectively collected in our TAVR database. Aortic dissection post-TAVR and reoperation for aortopathy were also recorded, as well as TTE measurements. Baseline grade of aortic regurgitation (AR),and follow-up paravalvular leakage (PVL) were graded as none/trace (0), mild (1), moderate or more (2).
MDCT images acquisition and measurements
Echocardiography is the primary imaging modality used to evaluate aortic valve and aortopathy. However,MDCT can obtain an excellent image of the full length of the aorta with the feature of 3D reconstruction, which makes MDCT a better method to identify ascending aorta diameter than echocardiography. No data was reported before about the ascending aorta diameter after TAVR using midterm to long-term MDCT follow-ups.
All MDCT examinations were performed with the second generation dual-source CT (SOMATOM Def inition Flash, Siemens Medical Solutions, Germany)as previously reported.[17]End-systolic images of baseline and follow-up MDCT were analyzed using 3mensio 8.0 (3mensio Medical Imaging BV, the Netherlands)[18]as presented in Figure 1. Both maximal and minimal diameters were obtained at the broadest level of ascending aorta. The diameter of the ascending aorta was calculated as: (maximal diameter + minimal diameter)/2.BAV was classified into three types by the number of raphes (type 0, type 1, and type 2) based on pre-TAVR MDCT analysis.[19]Patients with ascending aorta diameter >45 mm were identif ied. Changes of ascending aorta diameter were defined as the differences between follow-up and baseline measurements. Ascending aortic dilatation rates were calculated by dividing the change of ascending aorta diameter by the time interval in years for each patient.
Procedure
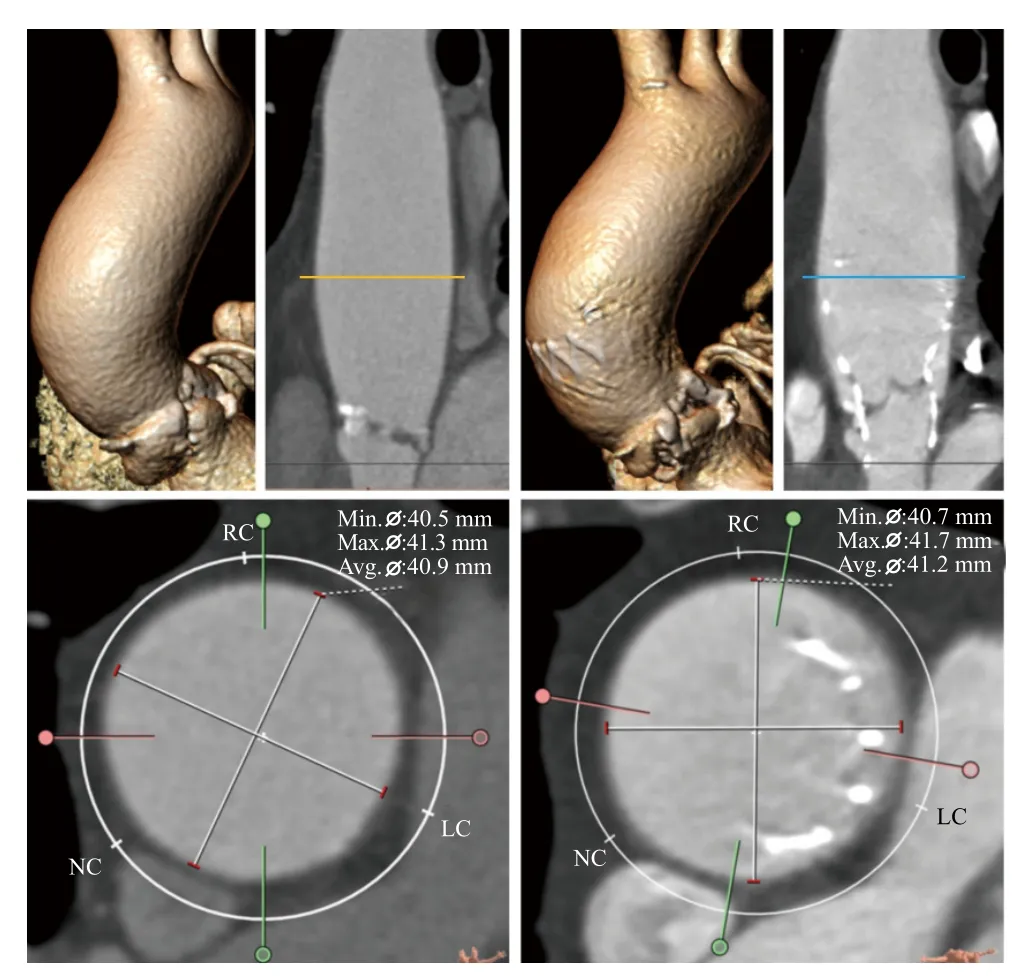
Figure 1. Diagram of ascending aortic diameter measurements of baseline and follow-up. The diameter of ascending aorta was measured at the broadest level of ascending aorta using baseline (left side) and follow-up (right side) multidetector computed tomography images.
Detailed procedures of TAVR were previously reported.[17,20]A large proportion of patients were implanted with self-expanding valves, such as:CoreValve (Medtronic Inc., Minnesota, USA), VenusAValve (Venus Medtech, Hangzhou, China), VitaFlow(Microport, Shanghai, China) and Taurus One-Valve(Peijia Medical, Suzhou, China). The rest of the patients were implanted with the Lotus valve (Boston Scientif ic,Marlborough, MA) or Edwards SAPIEN XT valve(Edwards Lifesciences, Irvine, California).
Statistical analysis
The data were analyzed using SPSS Statistics 22.0(SPSS, Inc., Chicago, IL). Continuous variables were described by mean±SD, and means were compared using t-test for normally distributed variables, or Mann-Whitney U test for skewed distributed variables.Categorical variables were expressed by frequencies and percentages, and they were compared using Chi-Square test or Fisher exact test between two groups. Univariate linear regression models were constructed to identify significant associations. If any univariate associations were identif ied with P value<0.20, they would be included in the multivariate linear regression to identify independent predictors. Age, sex, body surface area (BSA), history of hypertension, history of diabetes mellitus, BAV, types of prosthesis (self-expanding or others), years of follow-up,baseline and follow-up TTE parameters (mean gradient,Max velocity, aortic valve area [AVA] and left ventricular ejection fraction [LVEF], grade of AR and PVL) were evaluated as predictors of ascending aortic dilatation rate.Statistical signif icance was def ined as P<0.05.
RESULTS
Patient characteristics and procedural data
The flowchart of patient inclusion was shown in Figure 2. Two hundred and forty-nine consecutive patients underwent TAVR through transarterial approach for symptomatic severe AS from March 2013 to March 2018 at our center. Twenty-six patients died prior to MDCT follow-ups, 3 patients did not receive MDCT follow-ups due to chronic kidney disease, 10 patients refused MDCT follow-ups, and 2 patients had poor MDCT image quality. Thus, 208 patients with MDCT follow-ups constituted our study population. Baseline patient characteristics are listed in Table 1. The mean age was 76±6 years, the mean BMI was 22.78±3.41 kg/m2, and the mean BSA was 1.63±0.16 m2. Sixtytwo percent of the patients were male. Baseline MDCT classified 86 patients as BAV out of 208 patients (60 patients with no raphe, 26 patients with one raphe).The male and peripheral vascular disease were more common in tricuspid patients than in bicuspid patients.Bicuspid patients were complicated by more severe AS,but more severe AR was found in tricuspid patients.Ascending aorta diameters were signif icantly enlarged in bicuspid patients than tricuspid patients (43.7±4.4 mm vs. 39.1±4.8 mm, P<0.001). Meanwhile, more patients were found with ascending aortic diameter >4.5 cm in the bicuspid group than in the tricuspid group (36.0% vs.10.7%, P<0.001).
Transfemoral access was selected in 205 (98.6%)patients, with 170 patients were implanted with selfexpanding valves. All procedural data were comparable between the bicuspid and the tricuspid groups.
Ascending aortic diameter after TAVR
Table 2 summarizes the ascending aortic diameters and TTE measurements after TAVR. Five, 4, 3, 2, and 1-year MDCT follow-ups were achieved in 7, 9, 30,46, and 116 patients. Follow-up MDCTs showed that ascending aortic diameters were significantly increased in all patients (40.0±5.1 mm vs. 41.5±5.3 mm; P<0.001),in BAV group (43.7±4.4 mm vs. 44.0±4.5 mm; P<0.001)and in TAV group (39.1±4.8 mm vs. 39.7±5.1 mm;P<0.001). Mean change of ascending aortic diameter was 0.5±1.0 mm, and the mean dilatation rate was 0.3±0.8 mm/year in all patients. Diameters of ascending aorta were still larger in BAV group compared with TAV group (44.0±4.5 mm vs. 39.7±5.1 mm, P<0.001) after TAVR, but both change (0.4±0.9 mm/year vs. 0.6±1.1 mm/year, P=0.238) and dilatation rate of ascending aorta(0.2±0.8 mm/year vs. 0.3±0.8 mm/year, P=0.592) were similar between two groups. The frequency distribution of aortic dilatation rates is shown in Figure 3, and no rapid progressions (defined as≥5 mm/year)[21]were found. No signif icant differences of ascending aortic dilatation rate were found between patients with or without baseline ascending aortic diameter ≥ 45 mm in BAV group(0.4±0.7 mm/year vs. 0.1±0.8 mm/year, P=0.105), but a tendency was observed in TAV group (0.8±1.1 mm/year vs. 0.3±0.8 mm/year, P=0.052).
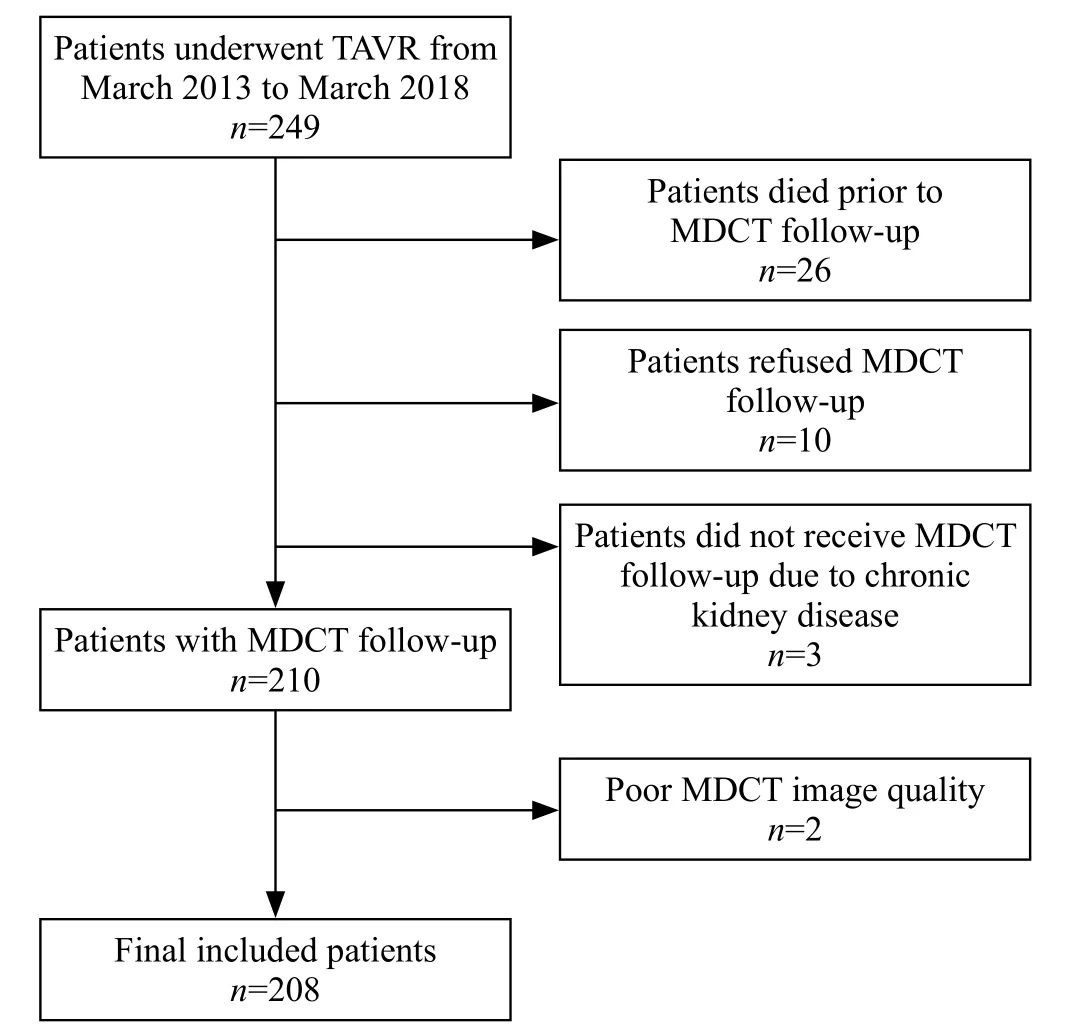
Figure 2. Flow diagram of patients’ inclusion. MDCT: multidetector computed tomography; TAVR: transcatheter aortic valve replacement.
TTE measurements showed that valve performances were comparable between two groups, except greater LVEF in the BAV group. BAV was not associated withmore PVL. No aortic dissections or reoperations for aortic dilatation were observed post-TAVR during follow-ups.

Table 1. Baseline characteristics and procedural data
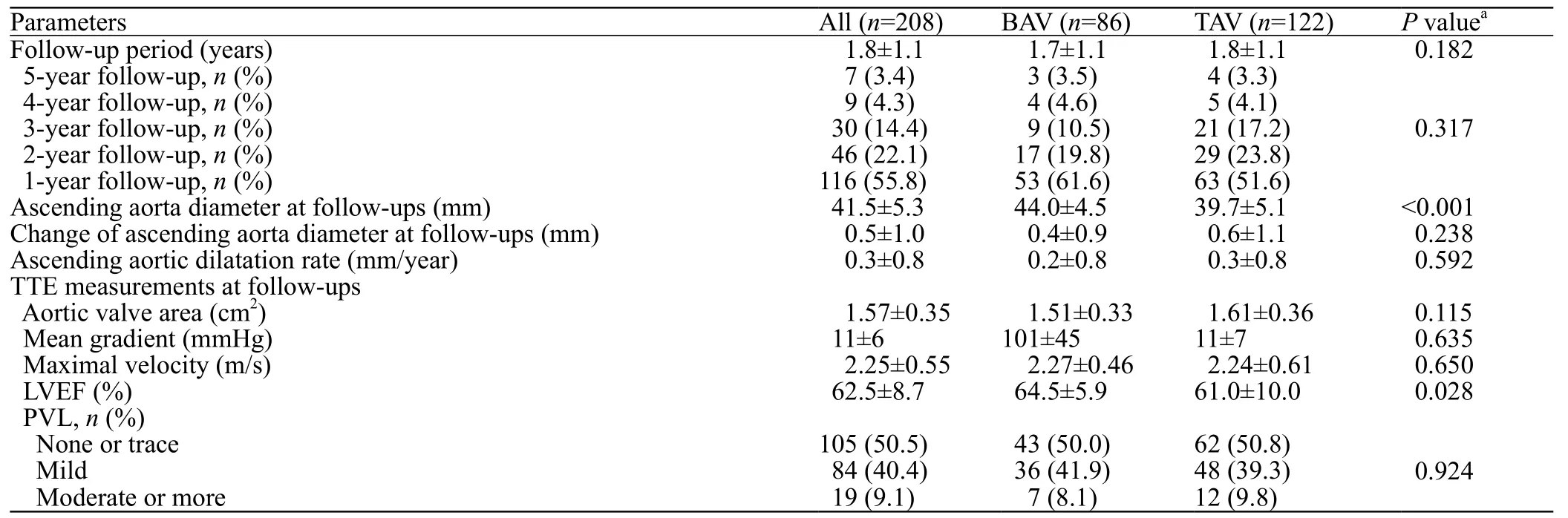
Table 2. Ascending aorta diameters and TTE measurements at follow-ups
Predictors of ascending aorta dilatation rate after TAVR
In the whole population, univariate linear regression revealed that age, sex, BMI, BSA, history of hypertension,history of diabetes mellitus, BAV, baseline ascending aortic diameter, implantation of self-expanding valves,years of follow-up, baseline TTE parameters (mean gradient, Max velocity, AVA and LVEF, grade of AR)and follow-up TTE parameters (mean gradient, Max velocity, AVA and LVEF) were not associated with ascending aortic dilatation rate, except grade of PVL(Coefficient=0.240, standard error=0.082, P=0.004)(Figure 4A). Baseline ascending aorta diameter, baseline AVA, and PVL were included in the multivariate linear regression model, and PVL was revealed as the only independent predictor (Coefficient=0.247,standard error=0.083, P=0.003). Subgroup analysis showed that PVL grade was significantly associated with the ascending aortic dilatation rate in the BAV group (Coefficient=0.482, standard error=0.115,P<0.001) (Figure 4B, Table 3) but not in the TAV group(Coefficient=0.081, standard error=0.112, P=0.470)(Figure 4C). PVL grade was still independently associated with ascending aortic dilatation rate in the multivariate regression model in the BAV group(Coefficient=0.495, standard error=0.117, P<0.001)(Table 3). A weak correlation was found between the ascending aortic dilatation rate at baseline and the ascending aortic diameter in the tricuspid group(Coeff icient=0.031, standard error=0.015, P=0.049).
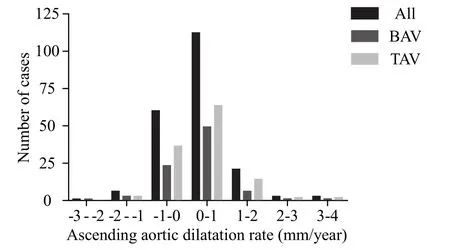
Figure 3. Frequency distribution of ascending aortic dilatation rate after transcatheter aortic valve replacement of the whole population,bicuspid group, and tricuspid group.
DISCUSSION
This present study reveals for the first time that ascending aorta continued to dilate after TAVR in both bicuspid and tricuspid AS patients after a midterm to a long-term MDCT follow-up. However, ascending aortic dilatation rate is similar between two groups.Multivariate regression analysis demonstrates that PVL after TAVR is independently associated with ascending aortic dilatation rate in BAV patients, but not in TAV patients.
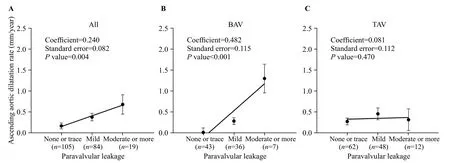
Figure 4. Correlation between paravalvular leakage grade and ascending aortic dilatation rate in the whole population (A), bicuspid group (B) and tricuspid group (C). Data are presented as mean ± standard error. BAV: bicuspid aortic valve; TAV: tricuspid aortic valve.
The size of the ascending aorta is changing throughout the lifetime. The average growth rate of ascending aorta in the population with TAV is found to be 0.15 to 0.20 mm/year.[22-24]In the setting of bicuspid patients, the growth rate of ascending aorta is altered by different phases of bicuspid natural history. In “normally functioning” BAV, the growth rate of ascending aorta is reported to be 0.39 to 0.77 mm/year, which is 2-4 times faster than that in the healthy tricuspid population.[25,26]The faster growth rate may be related to the genetically impaired aortic wall in patients with BAV and altered blood flow generated by normal functioning BAV.[7,15,27]When BAV becomes dysfunctional, ascending aorta seems to dilate faster with a growth rate of 0.6 to 0.9 mm/year.[23,28]As a result, aortic dilatation and aneurysm are more commonly seen in bicuspid AS than tricuspid AS patients,[29]which is consistent with this study. After BAV is removed by SAVR, the growth rate of ascending aorta was reduced to 0.18-0.28 mm/year,[8,30]which appears to be close to that in TAV population. In this study, after TAVR, the mean ascending aortic dilatation rate of BAV group was 0.2 mm/year, which was comparable to that of the TAV group after TAVR, as well as the previously reported average growth rate in normal TAV population (0.15 to 0.20 mm/year).[22-24]These results indicate that after hemodynamic abnormality is corrected, growth rate returns to be normal range, which supports the hemodynamic theory of bicuspid AS related aortic dilatation.
Despite advanced age, there are several reported predictors of ascending aortic dilatation, such as sex,BSA, hypertension, and hemodynamic parameters.[16,31,32]In our study, no correlation is found between ascending aortic dilatation rate and demographic variables or hemodynamic measurements at baseline. Interestingly,more serious PVL grades are strongly associated with faster ascending aortic dilatation. Thanassoulis et al[32]and Keane et al[33]reported AR as a predictor of aortic dilatation. Kinoshita et al[34]found that AR at the time of surgery was a significant predictor of dilatation of the aorta after SAVR. However, to the best of our knowledge, no study has reported before about the relationship between PVL and ascending aortic dilatation rate after SAVR or TAVR, probably due to the low incidences of PVL after SAVR and limited studies about aortic dilatation after TAVR. Theoretically, PVL might result in altered hemodynamics and increased stroke volume that places increased wall stress on the aorta and lead to faster aortic dilation. This result, again, indicates the hemodynamic impact on aortic dilatation.
Furthermore, subgroup analysis shows that PVL grade is associated with ascending aortic dilatation rate in BAV group, but not in the TAV group. The aortic wall of BAV patients seemed more vulnerable to PVL regardless of similar PVL grades between BAV and TAV group. These results imply that genetically triggered aortic wall abnormality of BAV patients still plays a role in progressive aortic dilatation after TAVR. Therefore,it is reasonable to assume that the interactions of both hemodynamics and genetics lead to aortic dilatation in bicuspid AS patients but not merely due to any single factor. Unfortunately, this study was unable to fully explain the mechanism of the relationship between PVL and progressive aortic dilatation after TAVR. With newer generation devices[35]available in mainland China mainland shortly, which can significantly decrease the severity of PVL, it is worth finding out whether newer generation devices affect slowing down the aortic dilatation rate in BAV patients by minimizing PVL grade.
The risks of aortic dissection in bicuspid patients with aortic dilatation are well established.[7,36]For patients with BAV undergoing SAVR, maximal ascending aorta≥45 mm is indicated for concomitant surgery for aortic dilatation.[2,37]However, these suggestions are mainly experience-based, and the reported i ncidences of aortic dissection are rare (0.1%-0.45% per patient-year).[25,38]Ascending aortic diameter ≥45 mm was found in 36.0%BAV patients in the present study, but no faster aortic dilatation was observed in patients with larger ascending aortic diameter prior to TAVR. Moreover, no aortic events were observed post-TAVR in our current study,which suggest that a conservative approach to mild-tomoderate ascending aortic dilatation is reasonable in bicuspid AS patients such as isolated SAVR or TAVR.However, a larger cohort and more extended follow-up period are needed to fully answer this question.
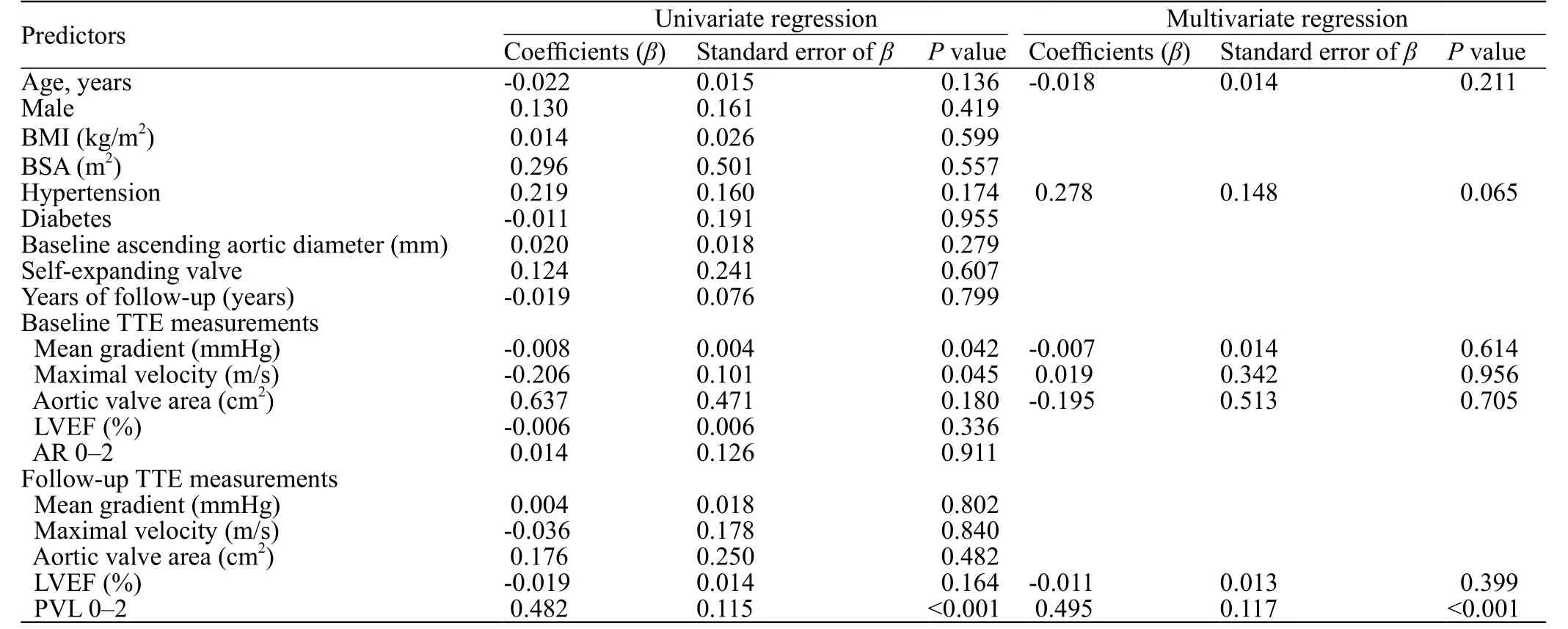
Table 3. Predictors of ascending aortic dilatation rate after TAVR in bicuspid group
Limitations
Our study is limited by the fact that it was a singlecenter study with a limited number of cases and selection bias. MDCT follow-ups were obtained in 83.5% (208/249)patients, which was incomplete. Different types of THVs were used in this study, which was a confounding factor when interpreting the results. Furthermore, PVL has been identified as an independent predictor of aortic dilatation rate in BAV patients who underwent TAVR, but our study failed to explain or verify this finding. Considering the slow rate of aortic dilatation progression after TAVR and low incidence of aortic events in the real-world practice,studies with a more significant number of cases and a longer follow-up are needed.
CONCLUSIONS
The current study demonstrates that ascending aorta continues to dilate after TAVR in both bicuspid and tricuspid AS patients after TAVR based on MDCT follow-up. However, aortic dilatation rate is similar between two groups. Aortic events are rare in realworld practice post-TAVR. PVL grade is associated with ascending aortic dilatation rate after TAVR.
ACKNOWLEDGMENTS
The authors thank all the members of the heart team of the Second Affiliated Hospital, School of Medicine,Zhejiang University, for their persevering work.
Funding:This study was supported by the Advanced Technique Research of Valvular Heart Disease Treatment Project(2015C03028); Role of TPP1 in anti-senescence and functional optimization of aged mesenchymal stem cells (81570233);Zhejiang Clinical Research Center for Cardiovascular and Cerebrovascular Disease (2018E50002); Role of FAIM in survival and functional improvement for aged mesenchymal stem cells(81770253); Zhejiang Clinical Research Center for Cardiovascular and Cerebrovascular Disease (2018E50002).
Ethical approval:The ethics committee of our center approved the study protocol and written informed consents were obtained in all patients.
Conflicts of interests:The authors declare that they have no competing interests. The funders had no role in the design, conduct,analysis, or interpretation of data or in writing the manuscript.
Contributors:All authors of this paper have read and approved the f inal version of the submitted manuscript.
 World journal of emergency medicine2019年4期
World journal of emergency medicine2019年4期
- World journal of emergency medicine的其它文章
- Information for Readers
- The utility of point-of-care ultrasound in the assessment of volume status in acute and critically ill patients
- Application of 4% formaldehyde under electronic colonoscope as a minimally invasive treatment of chronic hemorrhagic radiation proctitis
- Instructions for Authors
- My mother is looking blue
- Continuous B scan ultrasound guided post-traumatic sub-periosteal orbital hematoma drainage: An advantage over routine needle drainage procedure
