经导管主动脉瓣膜置换加微创冠状动脉旁路移植术1例报告并文献复习
牛兆倬 邵一兵 孙立新 戴红艳 毕晓磊 池一凡

[摘要]目的总结经导管主动脉瓣膜置换(TAVI)手术结合小切口不停搏冠状动脉旁路移植手术(MID`-CAB)的治疗体会。方法1例主动脉瓣膜重度狭窄老年女性,合并冠状动脉前降支严重钙化狭窄,在杂交手术室全麻下完成经左侧第4肋间小切口的MID`-CAB手术,后经左侧颈总动脉植入TAVI瓣膜。结果病人手术后恢复顺利,因术后并发Ⅲ度房室传导阻滞安装心脏永久起搏器,无其他并发症。结论TAVI+MID`-CAB治疗高危的主动脉瓣膜疾病合并冠心病病人安全有效。
[关键词]人工心脏瓣膜;冠状动脉旁路移植术,非体外循环;主动脉瓣狭窄;冠状动脉疾病;最小侵入性外科手术;病例报告
[ABSTRACT]ObjectiveTo summarize the experience in transcatheter aortic valve implantation (TAVI) combined with minimally invasive direct coronary artery bypass surgery (MID`-CAB). MethodsAn elderly woman with severe aortic valve stenosis and severe calcification and stenosis of the anterior descending coronary artery underwent MID`-CAB via a small incision at the left fourth intercostal space, followed by TAVI via the left common carotid artery. ResultsThe patient recovered well after surgery, and a pacemaker was implanted due to grade Ⅲ atrioventricular block. No other complications were observed. ConclusionTAVI combined with MID`-CAB and TAVI is safe and effective in the treatment of high`-risk aortic valve disease with coronary heart disease.
[KEY WORDS]heart valve prosthesis; coronary artery bypass, off`-pump; aortic valve stenosis; coronary artery disease; minimally invasive surgical procedures; case reports
符合經皮主动脉瓣膜置换(TAVI)手术指征的病例中冠心病的比例占40%~70%[1`-3]。美国和欧洲心脏病指南要求对于主动脉瓣膜手术中合并严重的冠状动脉病变病例,需要同期接受再血管化治疗,即在TAVI手术前先进行经皮冠状动脉支架介入手术(PCI)[4`-5]。然而,部分冠状动脉病变不适合进行PCI,近10年来多个中心报道了小样本的不停搏冠状动脉旁路移植手术(off`-pump CABG)联合TAVI杂交技术治疗此类疾病,结果理想[6`-9]。其中小切口不停搏冠状动脉旁路移植手术(MID`-CAB)结合TAVI手术的例数不多,但由于该项手术结合了目前最微创的冠状动脉旁路移植技术和TAVI技术,显示了良好的应用前景。我们完成了MID`-CAB联合TAVI杂交技术治疗主动脉瓣膜重度狭窄合并严重冠心病1例,取得了较好的效果,现将手术结果并文献复习报告如下。
1病例报告
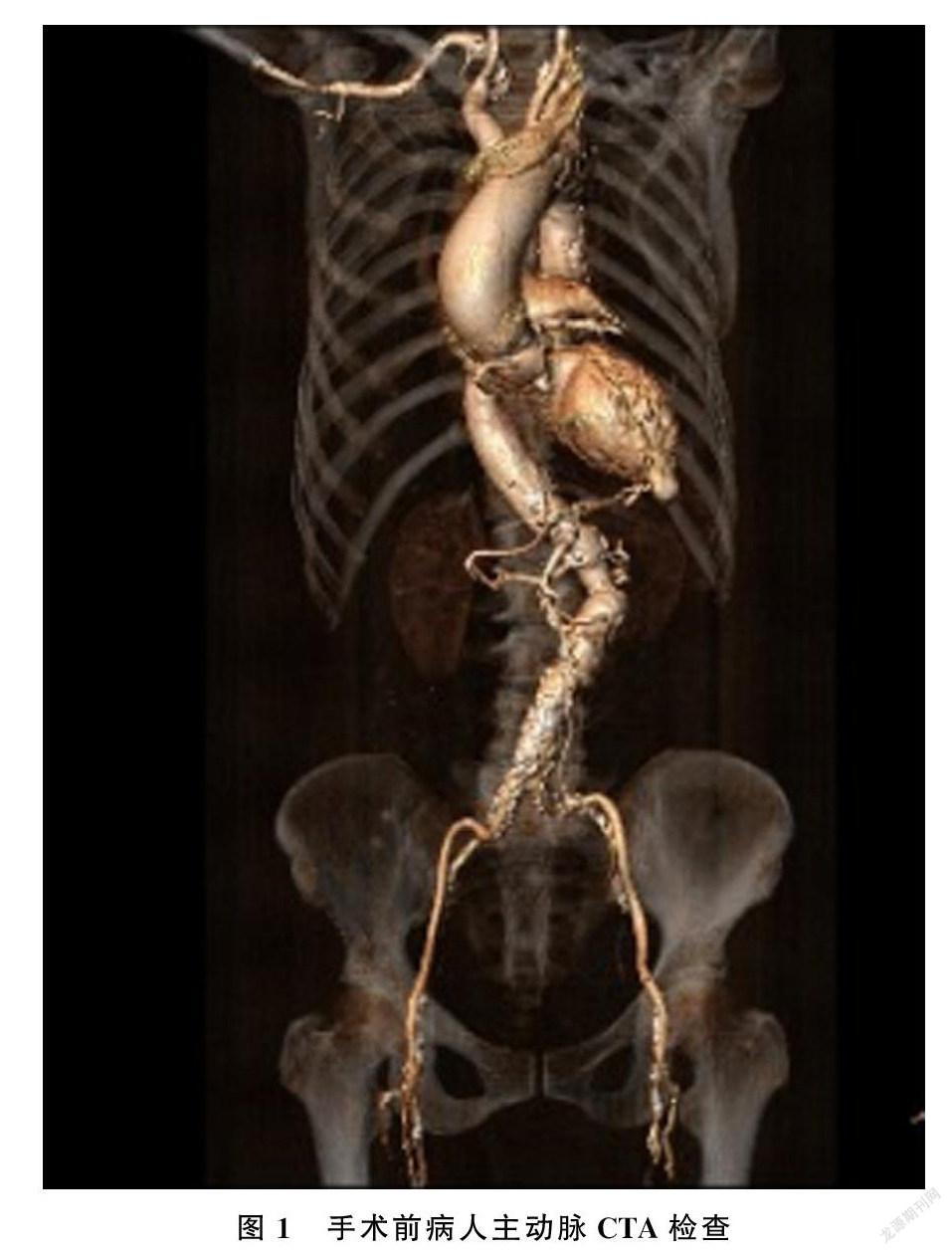
病人为80岁女性,因为反复胸闷不适1月余入院。病人高血压病史30年,否认糖尿病病史和其他疾病病史。入院查体:心率65 min-1,血压16.0/9.3 kPa,神志清,颈静脉轻度充盈,双肺呼吸音清晰,未闻及干湿性啰音,心律齐,主动脉瓣膜第一听诊区可以闻及Ⅲ级收缩期喷射性杂音,向颈部传导,余瓣膜听诊区未闻及有杂音。肝脾肋下未触及,双下肢无水肿。入院血常规和肝肾功能大致正常,肌钙蛋白I正常,B型钠尿肽(BNP)1 100 ng/L(正常范围0~100 ng/L),入院心脏超声提示主动脉瓣膜口面积为0.4 cm2大小,跨主动脉瓣膜平均压差为4.8 kPa,室间隔厚度为13 mm,左心室后壁厚度12 mm,左心室舒张末期内径为54 mm,心脏射血指数(EF)为35%。冠状动脉造影提示前降支近中段弥漫性钙化,近端狭窄80%,右冠状动脉陈旧性闭塞,前降支和后降支侧支循环形成。见图1、2。欧洲心血管病手术危险因素评分(EURO score)为14分,心内科评估前降支近中段严重钙化,不适行PCI。TAVI团队评估病人双侧髂动脉严重狭窄,常规股动脉入路无法通过,拟采用左侧颈总动脉作为手术入路。
TAVI手术常规在杂交手术室进行,手术团队包括了心内科介入医生、心脏外科医生、心脏麻醉师、心脏食管超声人员、放射技师和护理人员等。全麻成功后,左前斜位经左侧第4肋间小切口入胸,切口长8 mm,取左侧乳内动脉作为旁路移植材料,在心脏固定器辅助下,行左侧乳内动脉和前降支中段吻合,7`-0 普理灵(prolene)丝线连续法吻合,吻合完毕后测血流为12 mL/min,搏动指数为2.3。
手术关胸后,左锁骨上3 cm垂直切口游离左侧颈总动脉,注意避免损伤迷走神经,5`-0 prolene线缝荷包以便利操作时控住出血。静脉推注肝素维持活化凝血时间(ACT)在250 s以上。股动脉穿刺送入5 F鞘管,在0.035 J头软导丝导引下送入直头猪尾导管至无冠窦底部,以进行主动脉根部造影和释放标识。经股静脉穿刺送入6 F鞘管,送入临时起搏导线至右心室。经左侧颈总动脉荷包内穿刺送入8 F鞘管,将Amplaz导管送至主动脉瓣膜上3 cm左右,使用260 cm直头加硬超滑导丝穿过主动脉瓣膜送入左心室内,交换送入弯头猪尾导管,测量主动脉根部压力(17.3/8.7 kPa)和左心室压力(22.0/1.3 kPa)。 我们选择的是26# 国产VENUS`-A自膨式瓣膜,COOK的超硬导丝头部卷曲后送入左心室内部,在颈动脉穿刺送入20 F的亲水涂层鞘管至主动脉瓣上方4~5 cm处,心室起搏180 min-1,18 mm球囊预扩主动脉瓣膜。期间监测双侧脑氧饱和度。然后退出扩张球囊,送入预先安装好的VENUS主动脉瓣膜至主动脉内部,以左冠窦底部的猪尾导管作为定位参照,同时行主动脉根部造影,明确支架瓣膜的最低位置位于主动脉瓣环平面下5 mm,定位在主动脉瓣环以下,主动脉根部造影予以明确。同时将起搏心率调至180 min-1,缓慢释放瓣膜支架一半至瓣膜完全展开,主动脉根部再次造影观察支架瓣膜位置无误后释放支架。释放后存在中量瓣周漏情况,以22 mm球囊再次扩张1次,瓣周漏显著减少。手术后食管超声提示主动脉瓣膜压力差为0.75 kPa,微量瓣周漏。
病人手术后恢复平稳,术后14 h拔除气管插管。术后当天病人出现Ⅱ度Ⅱ型房室传导阻滞,在手术后第1天出现Ⅲ度房室传导阻滞,观察1周后,仍存在Ⅲ度房室传导阻滞,安装双电极永久起搏器。手术后1周心脏超声提示跨主动脉瓣膜平均压差为1.1 kPa,左心室舒张末期内径为53 mm, EF为55%。手术后14 d治愈出院。
2讨论
TAVI技术是治疗主动脉瓣膜退行性变的新技术,国际上已经得到广泛开展[10`-13],我国的TAVI手术量每年也以几何指数增加。目前部分TAVI手术病例合并冠心病,多采取PCI技术在TAVI手术前进行治疗[4`-5]。但是仍有较多不适合进行PCI治疗的冠状动脉病变,需要通过冠状动脉旁路移植手术方能解决。困难在于,接受TAVI手术的病例大多属于手术高危群体,常规的心脏手术难以耐受,如何将微创的TAVI技术和心脏冠状动脉旁路移植手术结合起来,是目前研究的热点[6`-14]。
TAVI手术的优势在于通过介入的方法将折叠的人工主动脉瓣膜送入体内,在主动脉瓣膜原位释放,利用原钙化瓣膜作为支撑固定在主动脉瓣环上,达到瓣膜置换的目的。由于手术不需要体外循环和心脏停搏,所以大大降低了手术的损伤;对于升主动脉有严重病变病例,在无法行主动脉切开或者阻断的情况下,也可以避免主动脉上操作,降低栓塞和大出血的风险[15`-17]。目前的研究结果表明,对于高危的心脏手术病例,TAVI手术的死亡率和并发症发生率均低于常规的心脏瓣膜手术[18`-20]。同时,off`-pump CABG也可以避免体外循环和心脏停搏,所以对于器官的保护作用优于体外循环下的冠状动脉旁路移植手术[21`-22]。近年来开展的MID`-CAB技术,多选择左侧第4肋间8~10 cm长切口进行,与常规经胸骨正中切口比较,手术创伤更小,输血量显著降低,病人的恢复更快[23`-24]。
多个心脏中心对于此类病例进行了小样本经验报道,这些病例均采用off`-pump CABG,目的是避免病人体外循环带来的全身炎性反应和器官低灌注状态,降低手术创伤。2010年,CHEUNG等[25]报道了首例off`-pump CABG结合经心尖部TAVI技术治疗此类疾病成功病人,他们采用了常规的off`-pump CABG,并利用正中手术切口选择经心尖部路径进行TAVI手术,手术获得成功,病人顺利康复。KOBAYASHIBA等[6]回顾性分析了12例美国胸外科风险评分(STS score)平均为6.1%的病人,他们接受了off`-pump CABG加TAVI杂交手术,手术为胸骨正中切口完成off`-pump CABG,然后在介入手术室经升主动脉路径完成TAVI手术,无住院死亡情况。AHAD等[7,26]观察了70例TAVI+off`-pump CABG杂交手术病例,其中部分病例采用的是MID`-CAB技术,手术的成功率为94.3%,但是30 d的死亡率為14.3%,这可能和手术前的逻辑欧洲心血管外科手术和风险因素评分高达35.9%以及STS score为12.2%有关。各项报道中均提出了off`-pump CABG结合TAVI手术形成新的杂交技术可以降低手术并发症发生率和死亡率,提高手术安全性。
我们选择的TAVI+MID`-CAB技术,是将两种手术的微创方式结合起来,对此相关的报道尚不多。手术病例为80岁高龄,主动脉瓣严重狭窄,术前EF为35%,术前有反复心衰症状,合并冠状动脉严重病变,术前评估为高风险手术,如果采用常规的体外循环下TAVI加冠状动脉旁路移植手术,手术创伤大,并发症发生率高。由于冠状动脉存在严重钙化,并不适合PCI技术。单纯进行TAVI手术存在严重心肌梗死的风险,经过反复讨论后决定采用MID`-CAB联合TAVI技术,由于病人双侧髂动脉严重狭窄,因此我们选颈动脉入路,术中监测双侧脑氧饱和度。病人首先经左胸第4肋间行小切口off`-pump CABG,再经左侧颈动脉入路行TAVI手术。手术后病人恢复顺利,植入瓣膜后瓣膜功能良好,冠状动脉病变在接受MID`-CAB后无心肌缺血表现,在围术期无相关心、脑、肾或者感染等常见并发症发生。术后出现的Ⅲ度房室传导阻滞属于TAVI手术常见并发症,给予安装心脏永久起搏器。
随着TAVI技术不断成熟和手术指征的进一步放宽,越来越多的主动脉瓣膜病变合并冠心病的病例会面对如何同时解决二者罹患的问题,单纯PCI技术并不能完全解决所有问题,外科冠状动脉旁路移植手术包括使用乳内动脉旁路移植,在手术的安全性和远期通畅率方面具有一定的优势[8]。MID`-CAB属于微创心脏手术,切口小,恢复快,对于主要是前降支病变或者合并对角支病变的冠心病病人有良好的远期效果[27`-31]。所以,MID`-CAB结合TAVI可以扩展目前的手术范围,对于各种复杂心血管疾病,通过术前的全面评估,选择最有利于病人的杂交手术方案,可以有效提高手术的安全性和远期效果。
[参考文献]
[1]DEWEY T M, BROWN D L, HERBERT M A, et al. Effect of concomitant coronary artery disease on procedural and late outcomes of transcatheter aortic valve implantation[J]. Annals of Thoracic Surgery, 2010,89(3):758`-767.
[2]DANSON E, HANSEN P, SEN S Y, et al. Assessment, treatment, and prognostic implications of CAD in patients undergoing TAVI [J]. Nature Reviews Cardiology, 2016,13(5):276`-285.
[3]FUSINI L, MIREA O, TAMBORINI G, et al. Incidence and severity of atherosclerotic cardiovascular artery disease in patients undergoing TAVI [J]. The International Journal of Cardiovascular Imaging[J]. 2015,31(5):975`-85.
[4]NISHIMURA R A, OTTO C M, BONOW R O, et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease a report of the American college of cardiology/American heart association task force on clinical practice guidelines[J]. Circulation, 2017,135(25): E1159`-1195.
[5]RAMEE S, ANWARUDDIN S, KUMAR G, et al. The ra`-tionale for performance of coronary angiography and stenting before transcatheter aortic valve replacement from the interventional section leadership council of the American college of cardiology[J]. JACC-Cardiovascular Interventions, 2016,9(23):2371`-2375.
[6]KOBAYASHI K J, WILLIAMS J A, NWAKANMAL L, et al. Aortic valve replacement and concomitant coronary artery bypass: assessing the impact of multiple grafts[J]. Annals of Thoracic Surgery, 2007,83(3):969`-78.
[7]AHAD S, WACHTER K, RUSTENBACH C, et al. Conco`-mitant therapy:off`-pump coronary revascularization and trans`-catheter aortic valve implantation[J]. Interactive Cardiovascular and Thoracic Surgery, 2017,25(1):12`-17.
[8]KOBAYASHI J, SHIMAHARA Y, FUJITA T, et al. Early results of simultaneous transaortic transcatheter aortic valve implantation and total arterial off`-pump coronary artery revascularization in high`-risk patients[J]. Circulation Journal, 2016,80(9):1946`-1950.
[9]DELLIS S L, AKUJUO A C, BENNETT E J, et al. Off`-pump coronary ar`-tery bypass grafting and transaortic transcatheter aortic valve replacement[J]. Journal of Cardiac Surgery, 2016,31(7):435`-438.
[10]CRIBIER A, ELTCHANINOFF H, BASH A, et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case description[J]. Circulation, 2002,106:3006`-3008
[11]GRUBE E, LABORDE J C, GERCKENS U, et al. Percuta`-neous implantation of the CoreValve self`-expanding valve prosthesis in high`-risk patients with aortic valve disease: the Siegburg first`-in`-man study[J]. Circulation, 2006,114:1616`-1624.
[12]NKOMO V T, GARDIN J M, SKELTON T N, et al. Burden of valvular heart diseases: a population`-based study[J]. Lancet, 2006,368:1005`-1011.
[13]TURINBA J, HESS O, SEPULCRI F, et al. Spontaneous course of aortic valve disease[J]. Eur Heart J, 1987,8:471`-483.
[14]CAO D, CHIARITO M, PAGNOTTA P, et al. Coronary revascularisation in transcatheter aortic valve implantation candidates: why, who, when[J]? Journal of Interventional Cardiology. 2018,13(2):69`-76.
[15]KELLY T A, ROTHBART R M, COOPER C M, et al. Comparison of outcome of asymptomatic to symptomatic patients older than 20 years of age with valvular aortic stenosis[J]. Am J Cardiol, 1988,61:123`-130.
[16]IUNG B, CACHIER A, BARON G, et al. Decision`-making in elderly patients with severe aortic stenosis: why are so many denied surgery[J]? Eur Heart J, 2005,26:2714`-2720.
[17]ZEGDI R, CIOBOTARU V, NOGHIN M, et al. Is it reaso`-nable to treat all calcified stenotic aortic valves with a valved stent? Results from a human anatomic study in adults[J]. J Am Coll Cardiol, 2008,51:579`-584.
[18]HIMBERT D, PONTNAU F, MESSIKA`-ZEITOUN D, et al. Feasibility and outcomes of transcatheter aortic valve implantation in high`-risk patients with stenotic bicuspid aortic valves[J]. Am J Cardiol, 2012,110:877`-883.
[19]WIJESINGHE N, YE J, RODES`-CABAU J, et al. Transca`-theter aortic valve implantation in patients with bicuspid aortic valve stenosis[J]. JACC-Cardiovascular Interventions, 2010,3(11):1122`-1125.
[20]HAYASHIDA K, BOUVIER E, LEFEVRE T, et al. Transcatheter aortic valve implantation for patients with severe bicuspid aortic valve stenosis[J]. Circ Cardiovasc Interv, 2013,6:284`-291.
[21]高長青,李伯君,肖苍松,等. 70 岁以上非体外循环与常规冠状动脉旁路移植术比较[J]. 中华心胸血管外科学杂志, 2002,18(3):150`-151.
[22]赵强. 微创冠状动脉搭桥术历史现状和前景[J]. 现代心血管外科, 2001,1(3):8.
[23]凌云鹏,鲍黎明,杨威. 左胸小切口非体外循环冠状动脉旁路移植术[J]. 中华胸心血管外科杂志, 2014,30(1):45`-46.
[24]胡盛寿. 复合技术——心血管疾病治疗的一种新模式[J]. 临床外科杂志, 2014,22(1):1`-4.
[25]CHEUNG A, HON J K, YE J, et al. Combined off`-pump transapical trans`-catheter aortic valve implantation and minimally invasive direct coronary artery bypass[J]. Journal of Cardiac Surgery, 2010(25):660`-662.
[26]AHAD S, BAUMBACH H, HILL S, et al. Transapical valve implantation and minimally invasive off`-pump bypass surgery[J]. Interact Cardiovasc Thoracic Surgery, 2014,18(2):248`-249.
[27]BAUMBACH H, ADILI S, URSULESU A, FRANKE U F,
2期牛兆倬,等. 经导管主动脉瓣膜置换加微创冠状动脉旁路移植术1例报告并文献复习205
et al. Concomitant transapical transcatheter aortic valve im`-plantation and minimallyinvasive direct coronary artery bypass [J]. Innovations (Phila), 2011,6(6):389`-390.
[28]MANOLY I, HASAN R, BRAZIER A, et al. Feasibility of hybrid off pump artery bypass grafting and transaortic transcatheter aortic valve implantation: a case series [J]. Catheter Cardiovasc Interv, 2017,89(7):1273`-1279.
[29]FINN M T, NAZIFf T M, FRIED J, et al. Coronary revascularization in patients undergoing transcatheter aortic valve replacement [J]. Canadian Journal of Cardiology, 2017,33(9):1099`-1109.
[30]STEFANINI G G, STORTECKY S, WENAWESER P, et al. Coronary artery disease in patients undergoing TAVI: why, what, when and how to treat[J]. Euro Intervention, 2014,10(10 Suppl): U69`-75.
[31]MYLOTTE D, OBADIA J F, SUDRE A, et al. Transcarotid transcatheter aortic valve replacement: feasibility and safety[J]. Journal of the American College of Cardiology, 2015,66(15, S): B285.
