The cholera epidemic of 2004 in Douala, Cameroon: A lesson learned
Christoph J. Hemmer, Jürgen Nöske, Stefan Finkbeiner, Günter Kundt, Emil C. Reisinger
1University of Rostock, Faculty of Medicine, Department of Tropical Medicine and Infectious Diseases, Rostock, Germany
2Gesellschaft für Internationale Zusammenarbeit, Yaoundé, Cameroon
3University of Rostock, Faculty of Medicine, Institute of Biostatistics and Informatics in Medicine and Ageing Research, Rostock, Germany
Keywords:Cholera Douala Cameroon Case fatality rate Staff-to-patients ratio
ABSTRACT Objective: To describe the outbreak of 2004 with a view of retrospectively identifying factors that might explain the low case fatality rate.Methods: Outbreak data from 4 915 Cholera patients from registers of the Regional Health Delegation in Douala were analyzed using SPSS. Chi-square test, univariate and multivariate analysis were applied.Results: The outbreak started January 2004, peaking at 187 cases per week in February. After a decrease in April, case numbers rose to 688 cases per week in June. The outbreak was over in September 2004 ( <10 cases per week). The case fatality rate was higher in treatment centers with fewer than one nurse per two patients, than in those with more nursing staff. A temporary staff reduction after the first wave of the epidemic was associated with the increase of the case fatality rate during the second wave. This increase was reversed after re-instating full staffcapacity.Conclusions: Providing sufficient nursing staff helps to lower the case fatality rate of cholera.Besides a lack of staff, age above 40 years is a risk factor for death in this disease.
1. Introduction
Cholera is a disease characterized by watery diarrhea, which may rapidly lead to fatal dehydration. It is caused by Vibrio (V.) cholerae,a Gram-negative comma-shaped bacillus. Six previous cholera pandemics are thought to have been caused by the “classical”biotype of V. cholerae O1, while the biotype V. cholerae O1 “El Tor” is largely responsible for the current seventh pandemic,which appears to have started in 1961 on the island of Sulawesi,Indonesia[1]. Over the years, the pandemic spread westward and reached the Republic of Guinea in West Africa in 1970. While the case fatality rate (CFR) can drop below 1% with adequate therapy,CFRs of up to 15% were seen in Africa[2,3].
In Cameroon, the first cholera outbreak was recorded in 1971.More than 2 000 persons became ill, of which 15% died[4]. In the following years, cholera epidemics occurred in Cameroon in 1986(> 1 000 cases, CFR 9%), in 1991 (> 4 000 cases, CFR 12%), 1996(5 786 reported cases, CFR 6.3%), 2004 (over 8 000 cases), 2005(2 847 cases, CFR 3.86%; 70% of the cases in the Littoral region),and 2009-2011 (22 762 reported cases, CFR 3.5%).
Douala has suffered several cholera epidemics since this disease was first seen in Cameroon in 1971, and the town districts with the least access to clean water are also those with the highest cholera attack rates[5]. Each year, at least 120 000 new inhabitants move in Douala. Many of the new arrivals settle in areas without adequate water supply and without adequate disposal of wastewater,particularly in the Bépanda-Makpèkè town district in the north of the city[5]. In the early 2000s, Douala had approximately 3 million inhabitants, but the national Cameroonian water utility company SNEC (Societé Nationale d’Éaux du Cameroun) counted only 65 000 customers in Douala[5]. The uncontrolled influx of new inhabitants, the poor infrastructure, the lack of safe drinking water,and the inadequacy of wastewater disposal, predispose Douala for cholera epidemics.
Like most cholera epidemics in the south of Cameroon, the 2004 epidemic, caused by V. cholerae O1, Biotype El Tor[5], started during the dry season, when water levels of the rivers were lower than usual,while rain water was not available. Between December 2003 and March 2004, precipitation in southern Cameroon was less than half of the average precipitation observed during these months between 1971 and 2003[6]. This drought appears to have exacerbated the shortage of safe drinking water and may thus have contributed to the cholera outbreak in January 2004. However, the second wave of the epidemic was associated with unusually strong precipitation, and the resulting inundations of streets and houses may have contaminated the water wells during the rainy season[6].
Here we analyzed the successful efforts undertaken by the Ministry of Public Health of the Republic of Cameroon and the Health Delegation of the Littoral Region of Cameroon, to contain the cholera outbreak in Douala in 2004 and to limit the overall CFR,which turned out to be 1.28%. These efforts were taken in close cooperation with the German Corporation for Technical Cooperation(“Gesellschaft für Technische Zusammenarbeit”[GTZ], today“Gesellschaft für Internationale Zusammenarbeit”[GIZ]), and the French Cooperation (“Coopération française”, today “Expertise France”). This study tries to identify factors that may have influenced the CFR.
2. Patients and methods
2.1. Patients
In the context of the 2004 cholera epidemic, 4 941 cases have been recorded in the register of the Provincial Health Delegation in Douala between January 19 and August 22. Of these 4 941 cases,sufficient data were available for 4 915 cases, and these cases were included in the present analysis. The remaining 26 cases had to be excluded because missing data rendered a meaningful analysis impossible. Therefore, the retrospective study presented here refers to those 4 915 cases that were treated in the city of Douala between January and August 2004 in 15 treatment centers, and for which sufficient data were available. The treatment centers had reported these cases to the Regional Health Delegation of the Littoral Region of Cameroon. Active cholera surveillance did not exist in Cameroon.Standard cholera reporting forms were introduced at the beginning of the 2004 cholera epidemic. These questionnaires included questions about the age, gender, place of residence, as well as the site where the infection was probably acquired.
Information on the course of the epidemic and on the measures implemented by the public health authorities were obtained from the minutes of the daily meetings of the Coordination Committee for the anti-cholera measures at the “Délégation Provinciale de la Santé Publique du Littoral à Douala” (DPSPL; i.e. Provincial / Regional Public Health Delegation of the Littoral Province), and the Douala City Council. Furthermore, official statements and interviews with health officials in Douala were used. Additional information was obtained from papers describing other aspects of the 2004 cholera epidemic in Douala[5,7,8].
Weeks have been numbered as calendar weeks according to Standard ISO 8601, section 2.2.10 (Calendar Week Numbers),of the International Organization for Standardization, Geneva,Switzerland[9]. According to ISO 8601, the first calendar week of 2004 started on Monday, December 29, 2003.
This retrospective analysis had been authorized by the health authorities of the Littoral Province of the Republic of Cameroon, and the health authorities cooperated in the implementation. Approval by an Ethics Committee was not required as the nature of the study was strictly retrospective.
2.2. Measures taken by the health authorities in Douala, in cooperation with GTZ
2.2.1. Supervision and training
The Coordination Committee established Training and Supervision Teams during March 2004. These teams started supervisory visits of the cholera treatment centers on March 29, observing the work performed in these centers and offering structured feedback. Each week, the teams visited the treatment centers. During some weeks,the teams only managed to visit 10 of the 14 treatment centers, due to time constraints. In addition, 11 of the 14 treatment centers held at least one mortality analysis session during the epidemic, in order to determine what should be learned from fatal cases. These mortality analysis sessions covered 39 of the 63 cholera deaths during the 2004 epidemic.
2.2.2. Providing safe drinking water
The administration of the City of Douala and the “Société Nationale des Eaux du Cameroun” (National Water Company of Cameroon)initiated a campaign of intensified servicing and repairing the water distribution network in Douala. In addition, the National Water Company of Cameroon established ten public distribution points for free drinking water. Seventeen new wells were built (of which 13 were still functioning at the end of the epidemic), and existing wells were chlorinated according to a standard protocol. In addition,stagnant wastewater ditches were cleaned and chlorinated throughout Douala. The purpose of these measures was to decrease the number of new cases.
2.2.3. Antibiotic therapy of patients and contact persons
Of the 4 915 cholera patients, 4 481 received a single oral dose of doxycycline, and 434 received three oral doses of amoxicillin instead, because they were below 8 years of age.
A total of 15 287 direct contact persons (relatives, close friends)were identified at the treatment centers. Of these, 15 154 received a single oral dose of doxycycline, and 133 received three doses of amoxicillin as cholera prophylaxis.
A total of 158 438 contact persons and exposed persons were identified elsewhere, usually neighbors of cholera patients receiving care at the treatment centers. Of these, 142 877 received a single oral dose of doxycycline in agreement with WHO recommendations[10].Doxycycline was contraindicated in the remaining 15 561 persons who received three oral doses of amoxicillin instead.
2.3. Data analysis and statistical methods
Patient data were extracted from questionnaires used during the epidemic and from handwritten records kept at the Public Health Delegation in Douala. They were entered into a Microsoft Excel®database in an anonymized fashion. Next, data were analyzed by descriptive statistics, and CFRs were calculated. For testing differences between CFRs, Fisher’s Exact Test was used. To test the hypothesis that the overall CFR was not different from 1%,which the WHO considers to be an indicator of adequacy of care for cholera patients, a one-sample t-test was performed. The predictive effect of age, gender, and staff-per-treatment-place (independent variables) on death or survival (dependent variable) was analyzed by univariate and multivariate logistic regression analysis, using the software packages ”Statistical Analysis Systems” and “Statistical Package for the Social Sciences”. Those independent variables,which appeared to have a significant influence (P< 0.05) on the dependent variable (i.e. death risk) in univariate testing, were also included in the multivariate analysis. The resulting relative death risks were indicated by Odds Ratios, 95% confidence intervals, and P values. P values below 0.05 (two-sided testing where applicable)were considered significant.
3. Results
3.1. Description of the epidemic and sequence of events
The first suspected case, probably the index case of the Cholera epidemic, was reported in January 3, 2004, in the “Sable” town district of northern Douala, which belongs to the health district“Cité des Palmiers”[8]. By January 19, twenty-seven cases of watery diarrhea, raising suspicion of cholera, had been identified clinically,and stool samples were sent to the Centre Pasteur de Cameroun in Yaoundé. A cholera outbreak was declared on January 22, after V.cholerae, biotype El Tor, strain O1, had been identified culturally in at least one of these stool samples[11]. As a consequence, 14 official cholera treatment centers were rapidly established in existing hospitals and clinics throughout Douala, and 212 staff members from existing health institutions were trained and reassigned to these treatment centers. The Provincial Health Delegation of the Littoral Province (today: Littoral Region) established a Coordination Committee, consisting of representatives of the Health Delegation,district health officials, the fire department, and members of international cooperation partner institutions, including the German Cooperation, and the French Cooperation (Coopération française).
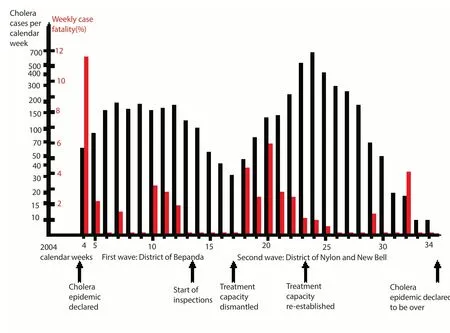
Figure 1. Timeline of the cholera epidemic of 2004 in Douala, Cameroon.
The cholera epidemic reached the first peak with 194 cases during the second week of February 2004 (7th calendar week), and the second peak with 182 cases during the third week of March 2004(12th calendar week). During this phase, over 30% of these cases occurred in the Bepanda town district, which had been known to be particularly susceptible to cholera during previous epidemics. After falling to a low of 31 new cases during the third week of April 2004(17th calendar week), case numbers rose again to a maximum of 688 cases in the second week of June 2014 (24th calendar week). This time, the majority of cases occurred in the town districts of Nylon(279 cases) and New Bell (139 cases). During the third week of August 2004 (34th calendar week), only 10 cases and no deaths were reported. On September 12, 2004, the cholera epidemic was declared to be over. Figure 1 shows the timeline of the epidemic.
In the course of the epidemic, stool samples from 104 (of 4 915)cases had been submitted to the center Pasteur de Cameroun in Yaoundé; information about locally performed stool tests was not available. In 78 of these 104 samples, V. cholerae O1, Biotype El Tor, was identified. In all other patients, clinical criteria were used to diagnose cholera in the context of the epidemic, as recommended by the WHO[12].
3.2. Patients and demographics
A total of 63 of the 4 915 cholera patients analyzed in this study died during the Douala epidemic of 2004. This overall CFR of 1.28% is not significantly different from 1% (One-Sample t-Test,95% CI from 0% to 3.598%). According to the WHO, adequate care of cholera patients leads to a CFR that is not different from 1%[2]. Gender information has been recorded for 4 899 of the 4 915 patients. Of these, 2 716 (55.44%) were male, and 2 183 (44.56%)were female.
Of the 2 716 male patients, 1 881 (69.26%) were between 15 and 39 years old, and 1 039 (38.25%) were between 20 and 29 years old. The median age bracket was the 25-29 years age bracket, and the most populated (i.e. modal) age bracket was the 20-24 years age bracket (553 patients or 20.36% of 2 716).
Of the 2 183 female patients, 1 380 (63.22%) were between 15 and 39 years old, and 77 (35.27%) were between 20 and 29 years old. The median age bracket was the 25-29 years age bracket, and the most populated (i.e. modal) age bracket was the 20-24 years age bracket (396 patients or 18.14% of 2 183).
3.3. Treatment centers and measures taken
3.3.1. Treatment Centers
The median number of nurses in all hospitals studied was 0.5 nurses per treatment place. Thus, on the average, one nurse cared for two beds or cots. Six treatment centers (Hôpital Laquintinie, New Bell District Hospital, Centre Médical d’Arondissement Bonnamoussadi,Douala Military Hospital, Centre Médical d’Arondissement Soboum) had fewer than 0.5 nurses per treatment place. In these, 43 of 1 983 cholera patients (2.13%) died. Ten other treatment centers had more than 0.5 nurses per treatment place. In these centers, 20 of 2 931 cholera patients (0.68%) died.
There was no significant age difference between the patients seen in hospitals with less than 0.5 nurses per treatment place (median 25 years old, range between 1 and 93 years old; interquartile range between 19 and 35 years old) and in hospitals with 0.5 or more nurses per treatment places (median 27 years old, range between 1 and 84 years old, interquartile range between 20 and 36 years old).
The number of hygiene specialists (up to 0.25 hygienists per treatment place vs. more than 0.25 hygienists per treatment place)had no significant effect on the CFRs.
A list of the treatment sites and the number of cholera patients is given in Table 1. In the largest cholera treatment center at the Hôpital Laquintinie, 1 128 cholera cases were treated, of which 26 (2.30%)died.
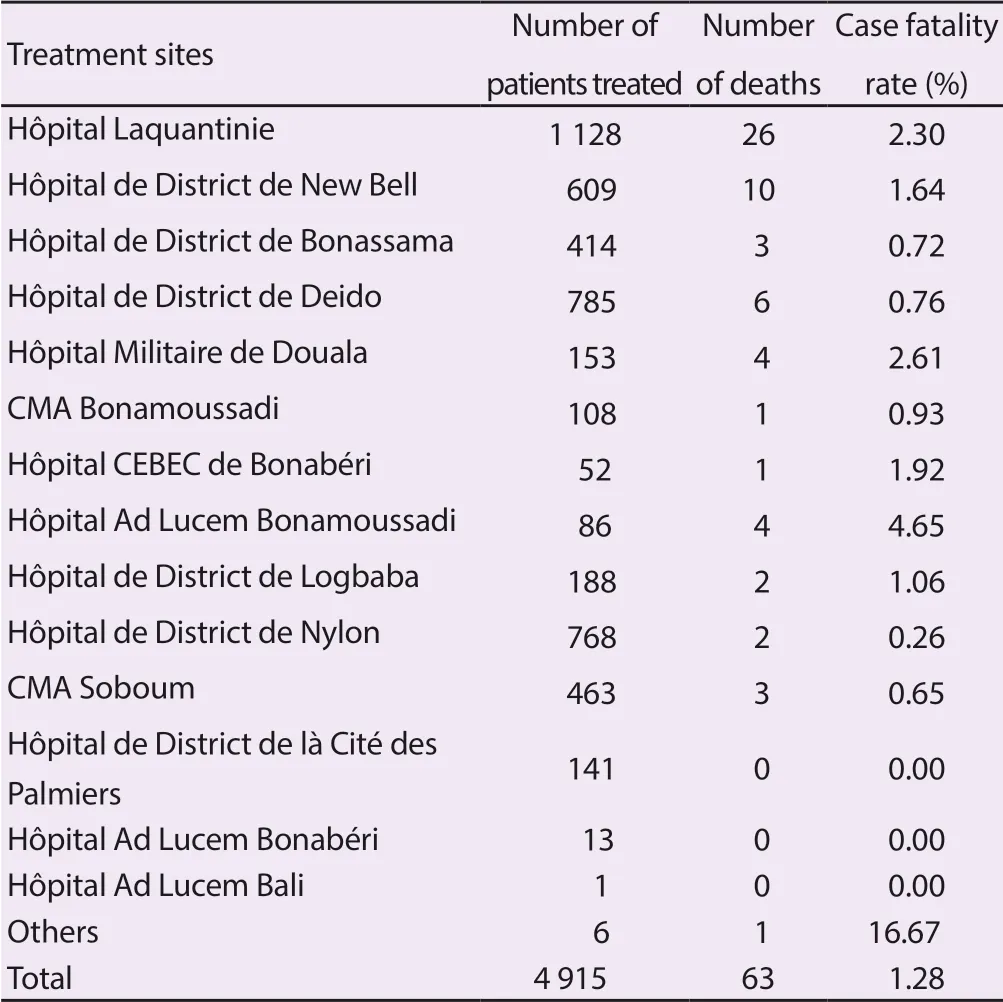
Table 1. List of cholera treatment sites in Douala.
3.3.2. Structured inspections
Between the declared beginning of the epidemic in January 2004 and the beginning of the structured inspections of the treatment centers at the end of March 2014, 27 of 1 406 cholera patients(1.9%) died. Between the beginning of the structured inspections and the end of the first phase of the epidemic during the last week of April 2004, two of 327 cholera patients (0.61%) died. Thus, there was a tendency towards decreased CFRs after the beginning of structured inspections, but this difference does not reach significance in the chi-square test (P=0.096).
3.3.3. Dismantling and re-establishment of treatment capacity at the Hôpital Laquintinie
When the case numbers dropped to 31 in the third week of April 2004 (17th calendar week), treatment capacities for cholera patients were partially dismantled at the Hôpital Laquintinie. When case numbers rose again, case fatality increased from 0 of 351 patients(0.00%; calendar weeks 13-17) to 22 of 644 patients (3.41%;calendar weeks 18-22). This increase was significant in the chisquare test (P<0.01 with Yates correction). During the 20th calendar week alone, 8 of 134 cholera patients (5.97%) died in Douala, and 6 of 45 cholera patients (13.33%) died in the Hôpital Laquintinie alone. After full treatment capacities had been re-established at the Hôpital Laquintinie, the CFR dropped to 0.69% (15 of 2 184 patients, calendar weeks 23-27). This drop was significant in the chisquare test (P<0.001 with Yates correction). By the second week of June or 24th calendar week, the CFR dropped to 7 of 688 cholera patients (1.02%), and the CFR remained low until the end of the epidemic.
3.4. Factors influencing mortality
3.4.1. Fisher’s Exact Test
Thirty-two of 4 047 patients (0.79%) aged up to 40, and 22 of 849 patients (2.59%) above the age of 40 died from cholera. The difference between these two groups is significant at P<0.001.Women appeared to have a lower CFR than men (0.87% vs. 1.36%),however this difference was not significant (P=0.107). The difference between the CFRs in centers with 0.5 or more nurses per treatment place and less than 0.5 nurses per treatment place was significant(P<0.009). In contrast, the number of hygiene specialists (up to 0.25 hygienists per treatment place vs. more than 0.25 hygienists per treatment place) had no significant effect on the CFRs.
3.4.2. Univariate regression analysis
The univariate regression analysis is shown in Table 2. Patients above 40 years were over three times more likely to die than patients below 40 years (P<0.001). Men appeared to be more likely to die than women, but this was not significant (P=0.106). Patients treated in centers with fewer than 0.5 nurses per treatment place were almost twice as likely to die than patients treated in centers with at least 0.5 nurses per treatment place (P=0.009).
When the death rates of the other treatment centers were compared with those of the largest cholera treatment center, the Hôpital Laquintinie, in univariate logistic regression analysis, the death risk was higher for patients treated at the Hôpital Laquintinie, compared to all patients treated elsewhere (P=0.001).
When the District Hospital of Nylon was compared with all other treatment centers in univariate logistic regression analysis, the death risk appeared to be lower for patients treated at the District Hospital of Nylon, compared to all patients treated elsewhere, but this was not significant (P=0.07).
3.4.3. Multivariate analysis
Because the parameters “age group” (up to 40 years old vs. older than 40 years old), “nurses per treatment place”, had a significant statistical effect on CFRs in univariate analysis, they were analyzed together by multivariate analysis. Their effect was also significant in multivariate analysis (age over 40 years old: OR=2.62; 95%CI: 1.55 -4.43; P=0.001; less than 0.5 nurses per treatment place:OR=1.95; 95% CI: 1.18-.21; P=0.009), which indicated that“age group” and “nurses per treatment place” were independent prognostic risk factors of dying from cholera in this epidemic.However, the effect of “being treated at Hôpital Laquintinie” on death vs. survival was not independent of the effect of “nurses per treatment place”, it was only independent of the effect of “age group”.
4. Discussion
The most remarkable result of this study is the observation that the overall CFR of the 2004 cholera epidemic in Douala was only 1.28%, which was below the CFRs seen in previous and subsequent cholera epidemics in Cameroon. It was not significantly different from 1%, which is used by the World Health organization as a marker of adequate care for cholera patients. In contrast, later cholera outbreaks in Cameroon were associated with CFRs of 6.1%in 2010 and 3.7% in 2011, respectively[13].
Since a structured multimodal approach was used to combat the 2004 epidemic of Douala, it is difficult to analyze the effect of individual measure taken. At the onset of the epidemic, the coordination committee had opted to set up several local cholera treatment centers in different parts of Douala, rather than one central treatment facility, as it had been done in earlier epidemics. This was done in order to avoid transporting patients all the way across Douala, which would have exposed even more inhabitants to the disease. Decentralized treatment centers probably have facilitated access to treatment.
Nevertheless, certain conclusions can be drawn. While structured feedback and supervision may help to improve survival of cholera patients, the data presented here suggest that one influence factor on death vs. survival in cholera is the staff-per-treatment-place ratio.A staffing rate of 0.5 nurses per patient bed or more was associated with a better survival rate than a staffing rate of fewer than 0.5 nurses per patient bed. In contrast, the influence of the number of hygienists failed to show a significant influence on the CFRs in the present study. This is expected, because the role of hygienists is not to improve the survival rate of cholera patients, but to prevent new cases of cholera.
Unfortunately, data on staff-per-treatment-place ratios in other cholera epidemics in Cameroon were not available to the authors.In later cholera outbreaks, other factors besides insufficient staff-per-treatment-place may have contributed to higher CFRs, including increased virulence and decreased antibiotic sensitivity of V.cholerae. A recent Chinese study has demonstrated that different cholera outbreaks tend to be associated with different genetically distinct clusters of V. cholerae which may also help to explain clinical differences between different outbreaks[14]. In Bangladesh and Moçambique, strains of V. cholerae El Tor with toxins characteristic of the more virulent classical biotype have emerged[15]. In 2004, the strains isolated in Douala were sensitive to doxycycline, ampicillin,and quinolones[16]. In 2005, ampicillin resistant V. cholerae emerged.In a more recent study conducted in the New Bell district of Douala, 92% of the V. cholerae isolates showed resistance against ampicillin, 88% against amoxicillin, 68% against tetracycline, and 64% against co-trimoxazole[17]. In addition, the change in the case definition of cholera in Cameroon in 2010, when clinical severity was de-emphasized, hampered comparison with later epidemics[13].However, this change in the case definition should increase the case numbers, and thus reduce the reported CFRs.
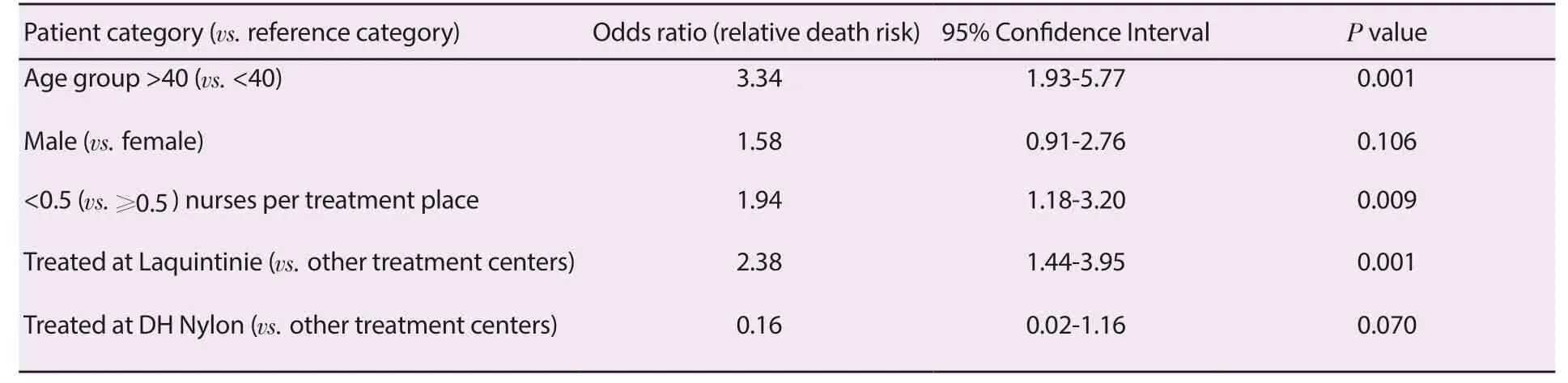
Table 2. Univariate analysis of relative death risks.
Even though comparison with other cholera outbreaks in Cameroon is difficult, this study underscores the need for sufficient nursing staff in cholera epidemics. Sudden blood pressure drops and other dangerous complications may be more frequent in the future, if the virulence of V. cholerae increases further. Management of these complications requires continuous observation of patients and immediate administration of additional i.v. fluids. In the second phase of the 2004 Douala cholera epidemic, most deaths occurred in the Laquintinie Hospital at a time of staff shortage, before a dismantled cholera treatment unit had been fully re-activated, and the staff had been called back. Without the data from Laquintinie Hospital, which was the largest treatment center in the 2004 epidemic, the CFR of the epidemic would have been 0.94% (3 825 cases, 36 deaths). The observed effect of the staffing ratios was not explained by age differences (advanced age is a known risk factor for a poor outcome in cholera). The age structures were similar in treatment centers with 0.5 or more nurses per treatment place and in those with fewer than 0.5 nurses per treatment place.
In summary, sufficient nursing staff (at least 0.5 nurses per patient bed in this study) is likely to help optimizing survival of cholera patients. This can have consequences for planning health care interventions in cholera epidemics. However, the characteristics of the prevalent strains of V. cholerae (e.g. toxin characteristics,antibiotic resistance) need to be taken into account as well.
Conflict of interest statement
The authors declare that they have no conflict of interest.
 Asian Pacific Journal of Tropical Medicine2019年8期
Asian Pacific Journal of Tropical Medicine2019年8期
- Asian Pacific Journal of Tropical Medicine的其它文章
- Chlamydoconidium-producing Trichophyton tonsurans: Atypical morphological features of strains causing tinea capitis in Ceará, Brazil
- Molecular identification of hemoplasmas in free ranging non-human primates in Thailand
- Tioxolone niosomes exert antileishmanial effects on Leishmania tropica by promoting promastigote apoptosis and immunomodulation
- Evaluation of in vitro and in vivo immunostimulatory activities of poly (lactic-co-glycolic acid) nanoparticles loaded with soluble and autoclaved Leishmania infantum antigens: A novel vaccine candidate against visceral leishmaniasis
- Pharmacological and analytical aspects of artemisinin for malaria:Advances and challenges
