Pancreatogastrostomy vs pancreatojejunostomy after pancreaticoduodenectomy:An updated meta-analysis of RCTs and our experience
Yun Jin,Yang-Yang Feng,Xiao-Gang Qi,Geng Hao,Yuan-Quan Yu,Jiang-Tao Li,Shu-You Peng
Yun Jin,Yang-Yang Feng,Xiao-Gang Qi,Geng Hao,Yuan-Quan Yu,Jiang-Tao Li,Shu-You Peng,Department of General Surgery,the Second Affiliated Hospital,College of Medicine,Zhejiang University,Hangzhou 310009,Zhejiang Province,China
Abstract
Key words:Pancreaticojejunostomy; Pancreaticogastrostomy; Systematic review; Metaanalysis
INTRODUCTION
Pancreatoduodenectomy (PD) is the main treatment procedure for benign and malignant tumors of the pancreatic head,lower common bile duct,and ampulla[1]. The incidence of complications after PD is still high,with some large pancreatic centers reporting an incidence of approximately 10-45%[2-7]. The incidence of pancreatic fistula(PF),delayed gastric emptying (DGE),and gastrointestinal or abdominal hemorrhage has been reported to be 3-45%[8],5%-61%[9,10],and 1%-8%[11],respectively. Other complications include abdominal empyema,incision infection,and pulmonary infection[12].
Since the establishment of PD,pancreatico-digestive tract reconstruction has been a highly valued research area,which is considered to be closely related to the success/failure of the surgery[13]. In general,pancreatico-digestive tract reconstruction includes pancreaticojejunostomy (PJ) and pancreaticogastrostomy (PG). Unlike gastrointestinal anastomosis,these two types of reconstruction after pancreatic surgery are diverse,with different results and evaluations. Therefore,there is still room for improvement in PJ and PG,and these procedures are still the focus of future research in PD.
This systematic review and meta-analysis aimed to further evaluate the role and importance of pancreatico-digestive tract anastomosis. Further,the advantages and disadvantages of PJ and PG were compared to provide a valuable reference for a more reasonable and safe choice of pancreatico-digestive tract reconstruction in the future.
MATERIALS AND METHODS
Eligibility criteria
All clinical randomized controlled trials,in which patients underwent PD with pancreatico-digestive tract reconstructionviaPJ or PG,were included.
手术后,周启明的情绪一直不好。他很容易焦虑很容易生气,她理解他。曾经的周启明,是这个家的山,现在他觉得自己不是家人最强大的依靠了。所以才会有一种特别强烈的挫败感吧。
Information sources
Studies were identified by searching electronic databases and scanning reference lists of articles. No limits were applied for languages and foreign papers were translated to English. The search was applied to Medline,Wanfang Data,EMBASE,Science Citation Index Expanded,and the Cochrane Library. The last search was run on March 15,2019.
Search
We used the following search terms to search all trial registers and databases: Pancreatoduodenectomy or Pancreatoduodenectomies or Duodenopancreatectomy or Duodenopancreatectomies or Pancreaticoduodenectomy or Whipple or PD or Whipple procedure or Pancreatoduodenal resection or Pancreaticoduodenal resection,Pancreaticojejunostomy or Pancreaticojejunostomies or Pancreatojejunostomy or Pancreatojejunostomies or Pancreaticoenteric anastomosis or Pancreatoenteric anastomosis or Pancreaticojejunal anastomosis or Pancreatojejunal anastomosis or PJ,or Pancreaticogastrostomy or PG.
Study selection
Eligibility assessment was performed independently in an unblinded standardized manner by two reviewers. Disagreements between reviewers were resolved by discussion.
Data collection process
One review author extracted the following data from the included studies and the second author checked the extracted data. Disagreements were resolved by discussion between the two review authors; if no agreement could be reached,a third author would take the decision.
Data items
Data were extracted from each included trial on: (1) Characteristics of trial participants including age,disease,and number of patients; (2) Intervention with PGvsPJ; (3) Type of outcome measures including the definition and occurrence of PF,DGE,and other postoperative complications.
Risk of bias in individual studies
To ascertain the validity of eligible randomized trials,two independent reviewers with adequate reliability determined the adequacy of randomization,concealment of allocation,blinding of patients,healthcare providers,data collectors,and outcome assessors.
Statistical analysis
The meta-analysis was performed using Review Manager 5.3. The Chi-square test was used to test heterogeneity among studies. The heterogeneity level was judged according toI2. Relative risk (RR),weighted mean difference (WMD),standardized mean difference (SMD),and 95%CI (confidence interval) were used.
For data with clinical heterogeneity,it is not easy to merge effect quantities. First,we tested heterogeneity among studies. Then subgroup analysis or meta-regression analysis was conducted according to heterogeneity. If data were insufficient or heterogeneity cannot be found,a random-effects model was used. The homogeneity of data was tested by the χ2test,and the homogeneity was quantitatively analyzed by theI2test. If there was no statistical heterogeneity,a fixed-effects model was used.When statistical analysis showed heterogeneity,a random-effects model was used.The significance level of the hypothesis test was set atP< 0.05.
To assess the risk of bias across studies,we plotted the effect by the inverse of its standard error for each trial. The symmetry was assessed both visually,and formally by the Egger's test.
RESULTS
A total of 11 studies involving 11 trials were identified for inclusion in the review[14-24].The search of PubMed,Wanfang Data,Embase,and the Cochrane Library provided 125 citations. Of the total 125 citations,29 studies were discarded because they did not meet the inclusion criteria. Nine additional studies were discarded because full texts for these were not available. The full texts of the remaining 65 citations were examined in further detail. Following this,51 studies were found not to meet the inclusion criteria as described,and three were repeat studies from the same institute at different time points (we chose the latest study in this case). Finally,11 studies met the inclusion criteria and were included in the systematic review. Figure1 shows the flow diagram of study selection (Figure1).
From 1995 to 2016,11 trials were included from nine counties. In all,909 patients underwent PG and 856 underwent PJ. PF was defined and classified following the International Study Group on Pancreatic Fistula (ISGPF) consensus guidelines in seven trials[15,17-22](Table1). The quality of these 11 trials is presented in Figure2.

Figure1 Study flow diagram.
PF data were available for all 11 trials randomizing 1765 patients and reporting data for them. In the meta-analysis,there was no significant hetero-geneity between these studies (I2= 20%); therefore,a fixed-effects model was applied. PF showed a significantly lower morbidity in the PG group than in the PJ group (odds ratio [OR] =0.67,95%CI: 0.53-0.86,P= 0.002) (Figure3). Grade A PF did not affect the disease outcome; therefore,we further analyzed the incidence of grades B and C PF. Seven trials with 603 PG and 581 PJ patients were included. In the meta-analysis,there was a significant difference in heterogeneity between these studies (I2= 61%); accordingly,a random-effects model was applied. Grades B and C PF was not significantly different between the two groups (OR = 0.61,95%CI: 0.34-1.09,P= 0.09) (Figure4).
Nine trials with 788 PG and 734 PJ patients were included for analyzing postoperative hemorrhage. In the meta-analysis,there was no significant heterogeneity between these studies (I2= 0%); accordingly,a fixed-effects model was applied. Postoperative hemorrhage showed a significantly lower morbidity in the PJ group than in the PG group (OR = 1.47,95%CI: 1.05-2.06,P= 0.03) (Figure5).
Nine trials including 780 PG and 738 PJ patients were included for the analysis of DGE. In the meta-analysis,there was no significant heterogeneity between these studies (I2= 47%),and therefore a fixed-effects model was applied. DGE was not significantly different between the two groups (OR = 1.09,95%CI: 0.83-1.41,P= 0.54)(Figure6).
DISCUSSION
PF is one of the most common complications after PD. PF not only causes serious complications such as abdominal bleeding but also increases the length of hospital stay and cost for patients. Our study showed that PG anastomosis can reduce the incidence of all grades of PF than PJ anastomosis. In 2005,the ISGPF defined PF and divided it into three levels[25]. In 2016,the group adjusted the classification of PF and defined grade A PF as a biochemical fistula[8]. Therefore,in this study,we considered the incidence of grades B/C PF in subgroup analysis. We believe that this statistical analysis has more clinical value and significance. We found no statistical difference in grades B/C PF between the two groups (PJ and PG). However,our result showed that PG anastomosis may increase the incidence of bleeding compared with PJ anastomosis.
相对“S城”“鲁镇”来说,“未庄”是鲁迅在《阿Q正传》中所展示的另一个重要的越文化空间和场域。它不是一座城,也不是一个镇(尽管鲁迅还将它称作为“村镇”),而是一个既具有典型的越文化风俗,又具有典型的“老中国”衰败特征的村庄。鲁迅对“未庄”是这样描写的:
Our group has studied the anastomosis of the pancreas and digestive tract for more than 20 years,and has accumulated some experiences[7,26,27]. In 1996,we established the binding pancreaticojejunostomy (BPJ). The main feature of this surgery is that the anastomosis between the jejunum and pancreas is mainly made with a binding line. It avoids the needle hole penetrating the intestinal cavity on the surface of theanastomotic site,thus preventing the leakage of pancreatic juice from the pinholes,to fundamentally eliminate the possibility of PF. At present,BPJ has been applied in more than a thousand of cases,which has a significant effect on the prevention of PF after surgery[7]. In 2010,Buc,a French scholar,named BPJ procedure as Peng's PJ and reported that BPJ was a safe and secure technique[28]. In 2008,Peng created the binding pancreaticogastrostomy (BPG),which simplified the operation steps of the previous pancreas-stomach anastomosis[29]. After continuous improvement,only the bundled method was used in the posterior wall of the stomach,avoiding the suture of pancreas parenchyma and thus greatly shortening the surgical time and preventing anasto-
motic leakage. BPG not only solves the problem of excessive pancreatic stump but also reduces the harm of bile leakage because the biliary-enteric anastomosis is not in the same channel as PG anastomosis[27]. The mid-term results of the randomized controlled study showed that the incidence of PF in BPG and BPJ was acceptable[17].

Table1 Characteristic of included trials

Figure2 Quality of the included trials.
In recent years,with the continuous development of laparoscopic technology,laparoscopic PD has gradually become an alternative method,used as a routine treatment in some pancreatic surgeries[30-32]. Thus,laparoscopic pancreaticogastrointestinal anastomosis has become a new focus for research. Owing to the limitation of the laparoscopic visual field,pancreatic duct to mucosa anastomosis is the first choice of procedure under laparoscopy[30].
The attempt of various methods makes the technique of PJ dazzling. However,the basic content cannot be separated from pancreas-jejunum (stomach) anastomosis or pancreatic duct-jejunum (stomach) anastomosis. The objective of evaluation should be as simple as possible. Moreover,the lower the incidence of pancreatic leakage compared with classical anastomosis,the better. As long as these principles are followed,sample enlargement and randomized controlled trials should be conducted to find the best method.

Figure3 Forest plot of the incidence of all grades of postoperative pancreatic fistula. PG:Pancreaticogastrostomy; PJ:Pancreaticojejunostomy; PF:Postoperative pancreatic fistula.
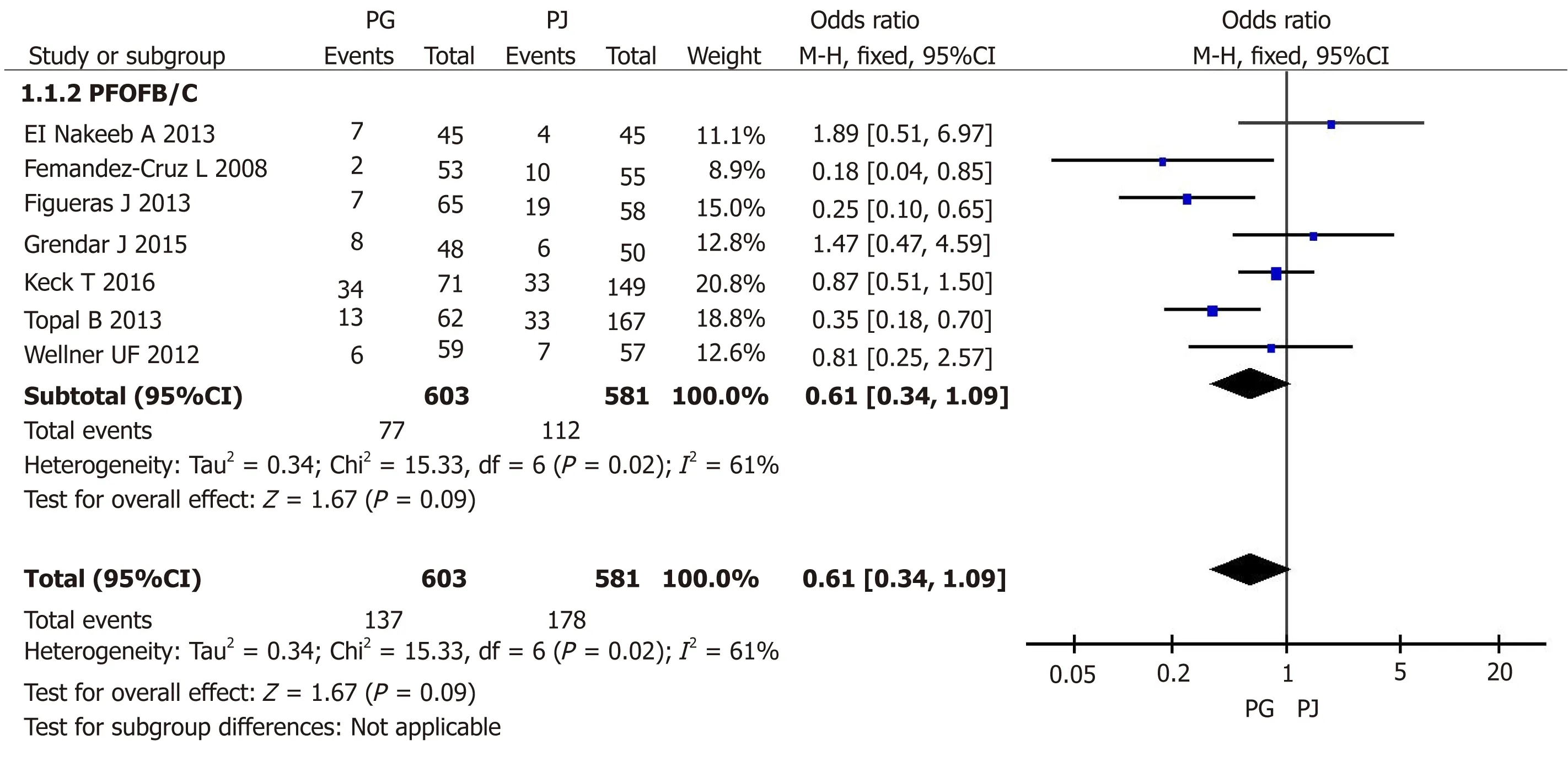
Figure4 Forest plot of the incidence of grade B/C postoperative pancreatic fistula. PG:Pancreaticogastrostomy; PJ:Pancreaticojejunostomy; PF:Postoperative pancreatic fistula.
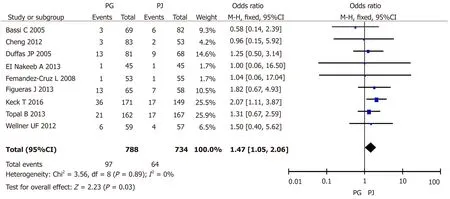
Figure5 Forest plot of the incidence of postoperative hemorrhage. PG:Pancreaticogastrostomy; PJ:Pancreaticojejunostomy.
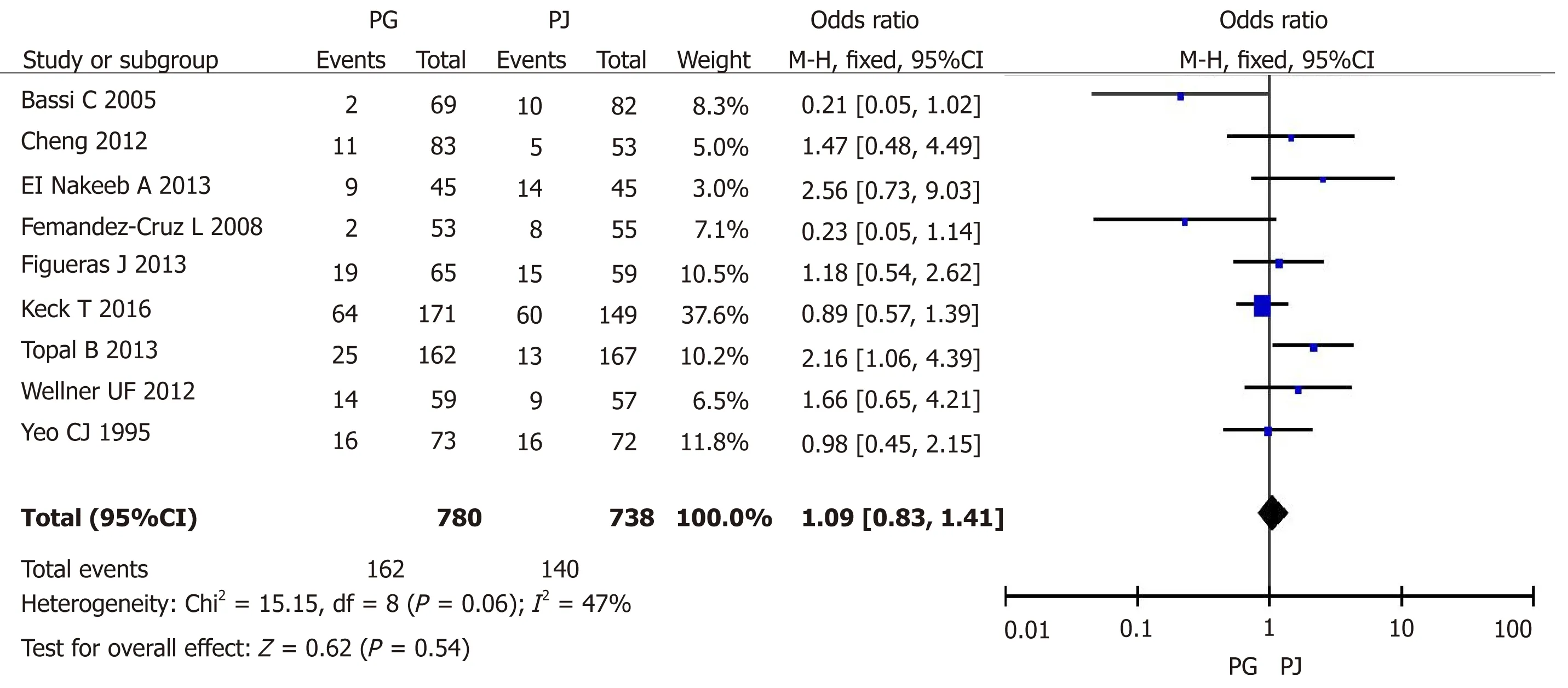
Figure6 Forest plot of the incidence of delayed gastric emptying. PG:Pancreaticogastrostomy; PJ:Pancreaticojejunostomy; PF:Postoperative pancreatic fistula.
ARTICLE HIGHLIGHTS
Research background
Pancreatoduodenectomy (PD) is one of the most important operations in hepatobiliary and pancreatic surgery. Pancreatico-digestive tract reconstruction includes pancreaticojejunostomy(PJ) and pancreaticogastrostomy (PG). Unlike gastrointestinal anastomosis,these two types of reconstruction after pancreatic surgery are diverse,with different results and evaluations.Therefore,there is still room for improvement in PJ and PG,and these procedures are still the focus of future research in PD.
Research motivation and objectives
This systematic and meta-analysis aimed to evaluate the role and importance of pancreaticodigestive tract anastomosis. Advantages and disadvantages of PJ and PG were compared to provide a valuable reference and safe choice in the future.
Research methods
This search was applied to Medline,Wanfang Data,Embase,Science Citation Index Expanded,and the Cochrane Library. The last search was run on March 15,2019. All clinical randomized controlled trials,in which patients underwent PD with pancreatico-digestive tract reconstructionviaPJ or PG,were included. The Chi-square test was used to test heterogeneity among studies.The heterogeneity level was judged according toI2. Relative risk (RR),weighted mean difference(WMD),standardized mean difference (SMD),and 95%CI were used.
Research results
In the meta-analysis of postoperative hemorrhage,there was no significant heterogeneity between these studies (I2= 0%); accordingly,a fixed-effect model was applied. Postoperative hemorrhage showed a significantly lower morbidity in the PJ group than in the PG group (OR =1.47,95%CI: 1.05-2.06,P= 0.03). In the meta-analysis of DGE,there was no significant heterogeneity between these studies (I2= 47%),and therefore a fixed-effects model was applied.DGE was not significantly different between the two groups (OR = 1.09,95%CI: 0.83-1.41,P=0.54).
Research conclusions
Our group has studied the anastomosis of the pancreas and digestive tract for more than 20 years,and has accumulated some experiences. We established the binding pancreaticojejunostomy (BPJ) and binding pancreaticogastrostomy (BPG). The mid-term results of the randomized controlled study showed that the incidence of PF in BPG and BPJ was acceptable.
Research perspectives
Laparoscopic pancreaticogastrointestinal anastomosis has become a new focus for research. The objective of evaluation should be as simple as possible. Moreover,the lower the incidence of pancreatic leakage compared with classical anastomosis,the better. As long as these principles are followed,sample enlargement and randomized controlled trials should be conducted to find the best method.

