Huge primary dedifferentiated pancreatic liposarcoma mimicking carcinosarcoma in a young female: A case report
Zhe Liu, Wu-Feng Fan, Gui-Chen Li, Jin Long, Yuan-Hong Xu, Gang Ma
Abstract
Key words: Pancreatic liposarcoma; Huge tumor; Distal pancreatectomy and splenectomy;Chemotherapy; Case report
INTRODUCTION
Based on molecular morphology, liposarcoma can be divided into well-differentiated/dedifferentiated liposarcoma, myxoid/round cell liposarcoma, and pleomorphic liposarcoma[1-3]. For dedifferentiated liposarcoma, it is thought that a malignant non-fat sarcomatous region exists in the well-differentiated liposarcoma area at the same time. To date, six cases of pancreatic liposarcoma have been reported in the English literature[4-9]. In the present study, a patient with a huge dedifferentiated liposarcoma in the pancreatic tail is reported. Pathology after operation revealed coexisting areas of well-differentiated liposarcoma, dedifferentiated liposarcoma, and the tissue of pancreatic canal. MDM2 gene amplification by fluorescence in situ hybridization showed a dedifferentiated liposarcoma that did not originate from the retroperitoneum.
CASE PRESENTATION
Chief complaints
A 28-year-old female presented with left upper abdominal discomfort with nausea and vomiting for more than 2 mo and fever for 2 wk.
History of present illness
The patient developed left epigastric discomfort with postprandial nausea and vomiting 2 mo previously without obvious predilection, the vomit consisted of stomach contents and abdominal distension was relieved after vomiting. She attended a local hospital for gastroscopy and was diagnosed with chronic atrophic gastritis, but no significant improvement was achieved after symptomatic treatment including acid inhibition and gastric preservation. She also had fever and chills for 2 wk, and as her temperature reached 39 °C, she was sent to the People's Liberation Army 202 Hospital, where an abdominal mass was found during computed tomography (CT)examination. The patient was then transferred to our hospital for further diagnosis and treatment. She was mentally stable, with a poor diet and poor sleep, with no obvious defecation and urinary abnormalities, and her weight loss was approximately 8 kg.
History of past illnessNone.
Personal and family historyNone.
Physical examination upon admission
The sclera showed no yellow staining, and no bleeding spots or petechiae were observed in the skin mucosa. No liver palm or spider mole was present, superficial lymph nodes were not palpable, the left epigastrium was slightly distended,gastrointestinal peristaltic wave was not observed, the abdomen was soft without tenderness, Murphy’s sign was negative, and the liver and spleen were not palpable under the rib. The mass was palpable in the left epigastric region and was approximately 15 cm in diameter. There was no muscle tension or rebound pain, no percussion pain in the liver and spleen area, shifting dullness was negative, and bowel sounds were 3-4 times/min, with no smell, air water sound, or high-pitched bowel sounds.
Laboratory examinations
混凝土表面提浆处理应采用三轴混凝土提浆平整机,以保证桥面均匀、平整、密实,达到较好的施工效果。钢纤维混凝土铺筑的成型与否十分重要,直接影响桥梁工程施工质量,由于钢纤维混凝土含沙量大,粗细骨料和纤维分布很不规则,采用真空吸水方式能够确保钢纤维混凝土施工质量。施工完成后进行混凝土表面抹平的过程中应采取相应措施避免钢纤维外露,确保施工效果。
Carcinoembryonic antigen was 0.76 ng/mL, alpha-fetoprotein was 2.14 ng/mL,cancer antigen 12-5 was 45.40 U/mL, carbohydrate antigen 19-9 was 6.13 U/mL, total bilirubin was 8.80 µmol/L, and direct bilirubin was 4.70 µmol/L.Imaging examinations
The enhanced pancreatic 3D-CT images suggested a huge mass in the left upper abdomen with low density and a maximum cross-sectional area of 14.0 cm × 18.0 cm.The plain CT value was 16-24 HU.
Multiple vascular shadows were observed in the arterial phase, and the enhanced CT value was 60-95 HU in the lag period. Compressed and tortuous superior and inferior mesenteric arteries and veins were observed. A pancreatic tumor was considered, and pancreatic carcinosarcoma was not excluded (Figure 1).
Preoperatively, pancreatic carcinosarcoma was suspected, and the patient underwent surgery. Intra-operatively, the transverse colon, stomach, and jejunum were compressed by the huge tumor, which had an irregular shape, an acceptable boundary, and a clear boundary with the retroperitoneum, suggesting that the tumor was originated from the pancreatic tail. Complete resection of the pancreatic tail was performed. A mass with a proximal margin of 1.0 cm of normal pancreatic tissue was removed (Figure 2A). The inside of the mass was fish-like in texture and yellowwhite. The distal pancreatic tissue was normal. Morphology inside the tumor showed no normal tissue (Figure 2B). Thus, a pancreatic source was considered and not retroperitoneal encapsulated pancreas as suggested by visual observation.
Postoperative pathology showed well-differentiated adipose tissue. Various cell sizes and shapes were observed with different trachychromatic atypia nuclei and a coexisting pancreatic canal (Figures 3A, C). Spindle cell hyperplasia was also observed when the coexisting area of undifferentiated liposarcoma and pancreatic canal were examined (Figures 3B, D). The pancreatic source was microscopically verified. Immunohistochemistry results showed the following: CK (-), vimentin (+),CD34 (+), CD117 (±), smooth muscle actin (-), S-100 (±), Dog-1 (±), CD68 (+), Desmin (-), MyoD1 (focus+), Bcl-2 (+), Beta-catenin (-), and Ki-67 (25%+). In order to verify whether the tumor was an undifferentiated liposarcoma, had a pancreatic source, and local infiltration and metastasis were present, MDM2 gene amplification of the mass and adjacent normal retroperitoneal tissue was performed. MDM2 gene amplification of the mass was positive (Figure 4A), while that of adjacent retroperitoneal tissue was negative (Figure 4B). This reconfirmed that the mass was pancreatic in origin and was a dedifferentiated liposarcoma.
FINAL DIAGNOSIS
Primary dedifferentiated pancreatic liposarcoma.
TREATMENT
Surgery.
OUTCOME AND FOLLOW-UP
The patient declined chemotherapy, but was well at her 26-mo follow-up, without relapse.
DISCUSSION
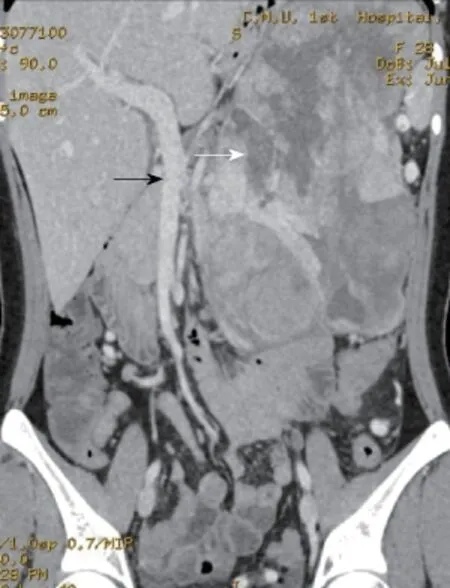
Figure 1 Preoperative computed tomography. Preoperative computed tomography shows a huge cystic-solid mass in the left upper abdomen, which compressed the superior mesenteric vein (Black arrow); necrosis can be seen in the mass (White arrow).
Dedifferentiated liposarcoma is a frequent type of liposarcoma that can occur in any part of the body[10]. It mainly occurs in the head, neck, limbs, and retroperitoneum[11-14].Studies have shown that it amplifies to the 12q13-15 area[15]. Genes such as MDM2 and CDK4 are included in this area, with MDM2 the most constantly expressed gene[16-19].Therefore, high expression of MDM2 plays a vital role in diagnosing dedifferentiated liposarcoma. Although liposarcoma is a common tumor, pancreatic liposarcoma is rare. To date, there are only six cases of primary pancreatic liposarcoma reported in the English literature[4-9](Table 1). According to a review of the existing literature, it is essential to confirm whether the tumor is a differentiated liposarcoma and to assess whether it originates from the pancreas. We suggest that this tumor can be diagnosed according to the following aspects: (1) Preoperative CT revealed pancreatic occupancy with an iconographic “interspace” in the retroperitoneum, stomach, colon, and small intestine; (2) A mass located in the pancreas or a pancreatic source was found during surgery, which could be completely cut out by blunt and sharp dissection; (3) Postoperative microscopic examination detected the co-existing area of the pancreatic canal, a well-differentiated liposarcoma, and undifferentiated liposarcoma; (4) MDM2 gene amplification by fluorescence in situ hybridization examination confirmed that the mass had a positive amplification, and the retroperitoneum or other control tissues had a negative amplification; and (5)There was no evidence of liposarcoma at the other sites.
CONCLUSION
Most cases are diagnosed via surgery combined with pathology. One of the cases in the literature was diagnosed by positive amplification of MDM2. However, from the comprehensive review, the diagnosis lacked evidence, which is the key in diagnosing this disease. In addition, we did not exclude the pancreatic source according to preoperative CT, and the first histological report revealed a pancreatic liposarcoma.We revised the diagnosis following MDM2 detection and re-evaluated the microscopic hematoxylin and eosin staining. In all seven cases, it was found that the tumor may be derived from the pancreatic matrix, and evidence of a pancreatic source is not enough. This tumor has a poor prognosis when the onset site is the pancreatic tail. Therefore, post-operative chemotherapy was suggested for the patient in the present study with gemcitabine and cis-platinum, but it was declined. The patient was well at the 26-mo follow-up, without relapse. We conclude that this tumor has a low incidence. When a patient is diagnosed with liposarcoma, chemotherapy should be included in the treatment regimen. Complete resection is the only effective treatment.
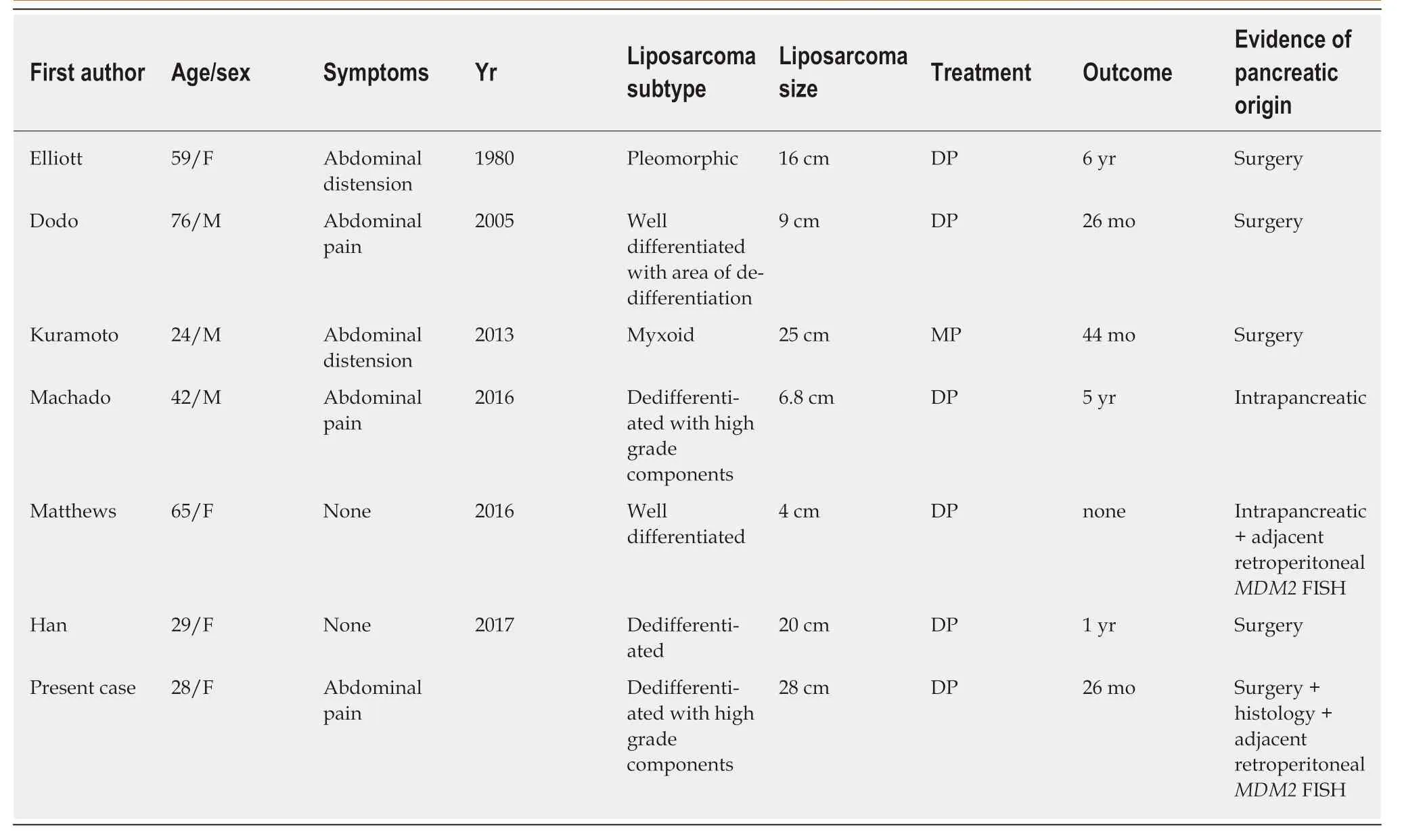
Table 1 Previously reported cases of pancreatic liposarcoma

Figure 2 Surgical procedure. The pancreatic tail was removed. A: The giant mass in the pancreatic tail was approximately 28.0 cm × 19.0 cm × 8.0 cm. The black arrow shows the normal pancreatic tissue; B: The mass was longitudinally opened. The gray-white and fish-like incisal surface can be seen. The spleen is shown by the white arrow.
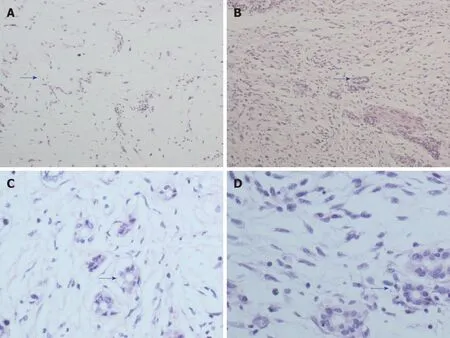
Figure 3 Histopathology. A: Coexisting areas of well-differentiated liposarcoma and the pancreatic canal (H and E × 100); B: Coexisting areas of dedifferentiatedliposarcoma and the pancreatic canal (H and E × 100); C: Coexisting areas of well-differentiated liposarcoma and the pancreatic canal (H and E × 400); D: Coexisting areas of dedifferentiated liposarcoma and the pancreatic canal (H and E × 400). Blue arrows show areas containing the pancreatic canal. H and E: Hematoxylin and eosin.
 World Journal of Clinical Cases2019年11期
World Journal of Clinical Cases2019年11期
- World Journal of Clinical Cases的其它文章
- Multiple synchronous anorectal melanomas with different colors: A case report
- Paraneoplastic leukemoid reaction in a patient with sarcomatoid hepatocellular carcinoma: A case report
- Development of a biliary multi-hole self-expandable metallic stent for bile tract diseases: A case report
- Lupus enteritis as the only active manifestation of systemic lupus erythematosus: A case report
- Application of pulse index continuous cardiac output system in elderly patients with acute myocardial infarction complicated by cardiogenic shock: A prospective randomized study
- Clinical features of syphilitic myelitis with longitudinally extensive myelopathy on spinal magnetic resonance imaging
