Paraneoplastic leukemoid reaction in a patient with sarcomatoid hepatocellular carcinoma: A case report
Bo Hu, Xin-Ting Sang, Xiao-Bo Yang
Abstract
Key words: Paraneoplastic leukemoid reaction; White blood cells; Bone marrow examination; Sarcomatoid hepatocellular carcinoma; Poor prognosis; Case report
INTRODUCTION
Leukemoid reaction is referred to as the condition in which reactive leukocytosis has exceeded 50000/μL, accompanied by a significant increase in the early neutrophil precursors. Typically, leukemoid reaction can serve as a paraneoplastic manifestation of various malignant tumors, including lung, gastrointestinal, genitourinary, ovarian,and head and neck cancers, as well as hepatocellular carcinoma (HCC)[1]. Generally,the most common presentation of the paraneoplastic leukemoid reaction (PLR) is less severe and lacks an increase in the levels of inflammatory markers. It shows no response to antibiotic therapy[2-5]. Moreover, the PLR-induced complications mainly result from increased blood viscosity, and gangrene in the foot has been described in one report[6]. As a result, to manage PLR is indeed to treat the underlying tumor.
Sarcomatoid hepatocellular carcinoma (SHC) is characterized by the proliferation of spindle cells or bizarre giant cells[7]and is usually associated with a dismal prognosis and high risks of recurrence and metastasis. Typically, the hepatocellular markers were negative in the malignant spindle cell component, whereas creatine kinase (CK)and vimentin were positive in most SCC patients[8]. SHC is distinct from nonsarcomatoid liver cancer. However, it can be misdiagnosed as intrahepatic cholangiocarcinoma, making differential diagnosis necessary. PLR is even more rarely seen in SHC patients, which was fatal in our case.
CASE PRESENTATION
Chief complaints
A 75-year-old female patient presented to the hospital as a result of right upper quadrant abdominal pain. Meanwhile, she also complained of anorexia and progressive generalized weakness.
History of present illness
易非喜欢坐火车,她喜欢这种有人陪伴,又可以想自己的心事的交通工具。这趟火车是风城通往外界的最便捷出口,也是她每次出差的主要交通工具。经常是各色人等拥塞其中。这次主任带他们东征省城,本来是带了专驾来的,可车子临时出了点儿小状况,主任突发奇想要忆苦思甜一下,选了这列火车,却正好合了易非的心意。
Patient’s symptoms started two months ago with recurrent episodes of bloating.
History of past illness
The patient had a past history of hypertension and cerebral infarction that caused mild instability in walking.
Physical examination
On the first admission, her temperature was 36.4 °C, blood pressure was 100/63 mmHg, pulse rate was 82 beats/min, and respiratory rate was 16 breaths/min.Physical examination revealed tenderness in her right upper abdomen, with no evidence of any abdominal mass.
Laboratory examination
Laboratory examination showed a white blood cell (WBC) count of 43790/μL, with 87.1% of neutrophils, hemoglobin of 12.7 g/dL, platelets of 36200/mm3, total bilirubin of 0.12 mg/dL, direct bilirubin of 0.05 mg/dL, albumin of 3.7 g/dL, aspartate aminotransferase of 18 U/L, and alanine aminotransferase of 22 U/L. In addition,tests for serum tumor markers revealed no abnormalities in the levels of α-fetoprotein(AFP; 3.4 ng/mL) and carcinoembryonic antigen (1.80 ng/mL) but elevated levels of carbohydrate antigenic determinant (CA19-9; 72.6 U/mL). In addition, the coagulation profile was within normal limits, and the results of the hepatitis panel and human immunodeficiency virus antibody tests were negative. In view of the elevated WBC levels, the patient was discharged to the Hematology Clinic for bone marrow biopsy and other tests to rule out the possibility of blood diseases. Two weeks later, the patient was admitted again, and routine blood examination showed a WBC count of 77050/μL. Subsequently, the patient developed a fever of 38.6 °C, which did not subside after antibiotic infusion, and her blood WBC levels were not significantly lowered. The results of the bone marrow examination showed that the proportion of granulocyte-neutrophil nucleated cells was increased by 40%, and toxic granules could be observed (Figure 1). In addition, a peripheral smear revealed neutrophilia with band forms but no blasts. Subsequently, procalcitonin test was performed, and the result was 0.31 ng/mL, indicating a lower risk of infection. Moreover, repeat blood cultures were negative, but the WBC count was elevated continuously.
Imaging examination
Computed tomography (CT) revealed a 9.3-cm focal hepatic mass in the left lobe of the liver, along with dilatation of the intrahepatic bile duct (Figure 2). A chest radiograph suggested no abnormality.
FINAL DIAGNOSIS
Hence, symptoms, signs, and laboratory studies were negative for an infectious etiology. In summary, the elevation in WBC count was believed to be caused by a PLR, which was not a surgical contraindication.
TREATMENT
Hepatectomy for the liver mass was performed 5 d after the second hospitalization.Immediately after tumor removal, her presenting symptoms and laboratory values were improved remarkably. Typically, her WBC count had dropped to the normal level 5 d after surgery (Figure 3). Postoperative pathology examination revealed that the poorly differentiated malignant cells were positive for CD34, Vimentin, human epithelial membrane antigen, and cytokeratin 7 (CK7), while negative for CK19(Figure 4), which was suggestive of SHC.
OUTCOME AND FOLLOW-UP
Unfortunately, the patient died two and a half months after the second discharge.Since the patient’s family did not cooperate with our follow-up work, we are unable to know the specific circumstances of the patient’s death.
DISCUSSION
Generally, leukemoid reaction is conventionally defined as the condition in which the peripheral WBC count has exceeded 50000/μL, with a dominance of mature neutrophils, and it is related to the reactive causes outside the bone marrow, such as severe infection, poisoning, allergic reaction, drugs, or malignant tumors[3,9,10]. After the causes of the leukemoid reaction are removed, the abnormal changes in WBC counts in blood and bone marrow can return to normal levels within a short period of time.
Specifically, a PLR is a cancer-associated leukemoid reaction. Some scholars believe that PLR is more likely to occur in malignant tumor patients at middle-age[11]. At the same time, tumor stage is also related to the occurrence of PLR, which is particularly true for stage III-IV tumors. Notably, the underlying mechanism appears to be the production of growth factors by the tumor cells, such as granulocyte macrophage colony stimulating factor (GM-CSF), granulocyte CSF (G-CSF), and interleukins (IL-3 and IL-6)[11].
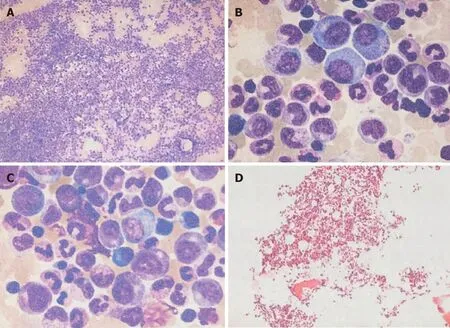
Figure 1 Bone marrow smear and bone marrow biopsy results. A-C: Bone marrow smears showed that hyperplasia was extremely active, the proportion of granulocyte-neutrophil nucleated cells increased, and most of the granules were coarse and numerous; D: Bone marrow biopsy examination showed that the hematopoietic tissue was obviously increased, the adipose tissue was reduced, the ratio of granulocytes to red blood cells was increased, and the megakaryocytes were visible.
PLR is rarely reported in SHC, and both have dismal prognoses. SHC is a rare histological subtype of HCC, which is discovered in 3.9%-9.4% of HCC autopsy cases and 1.8% of patients with surgically resected HCC[12-14]. However, the pathogenesis of SHC has not been fully elucidated yet, which may be associated with chronic hepatitis B, chronic hepatitis C, liver cirrhosis, preoperative radiotherapy or chemotherapy, and interventional therapy. Kim et al[15]believed that mutations in the p53 gene might be related to the occurrence of SHC. In our case, the patient showed no abovementioned predisposing factors and had not received any nonsurgical treatment. Some scholars call it “pure” SHC[16,17]. Typically, SHC is characterized by high malignancy grade,rapid progression, and poor prognosis. Compared with nonsarcomatoid HCC, SHC is characterized by lower levels of bilirubin, liver enzymes, and AFP, as well as a lower FIB-4 score. In addition, central necrosis and hemorrhage can be more frequently seen in SHC than in the ordinary type of HCC[14,18-20]. Our results are in accordance with previous studies reporting that more than 50% patients were negative for both HBsAg and hepatitis C virus antibody and had negative or low serum AFP levels. According to literature reports, some patients may have fever, but the WBC count is generally not high or is slightly elevated, suggesting the presence of noninfectious fever, which may be related to the sarcomatoid components or tumor parenchymal ischemia and necrosis. In our case, the patient developed fever after admission, with a significant increase in WBC count and neutrophil percentage, and her blood culture results were negative, which was suggestive of PLR. The WBC count in our case had dropped rapidly after surgery, which had confirmed our diagnosis.
In our case, SHC combined with a PLR was fatal, reflecting that such condition was aggressive. Shin et al reported a 71-year-old patient diagnosed with SHC, whose leukocyte count increased to 147800/μL and died on the 10thday of hospitalization,which also suggested the danger of this state. Unlike our case, the patient did not undergo surgery, and the pathological results were obtained by fine needle aspiration biopsy. We hypothesized that timely surgical treatment may be beneficial to such patient to some extent, but overall the prognosis is still poor. For malignant tumor patients with persistently unexplained elevated WBC count, PLR should be considered once infection is excluded. With regard to the relationship between PLR and sarcomatoid carcinoma, some scholars have reported cases of renal cell carcinoma and lung cancer with sarcomatous changes, accompanying PLR; however, it has not been specifically reported whether PLR is more common in sarcomatoid cancer[21,22]. It is likely that the progression and necrosis of SHC may be associated with an increase in inflammatory cytokine response, which may thereby result in leukemoid reaction.In an article examining the relationship between PLR and solid tumors, Chakraborty et al[10]reported a case of SHC with PLR who died 10 d after admission, which is earlier than most other types of tumors (such as cervical cancer, HCC, and gastric cancer). In terms of treatment, liver resection or liver transplantation is the therapeutic gold standard for such patients[23], but the effect is still unclear. On the other hand,
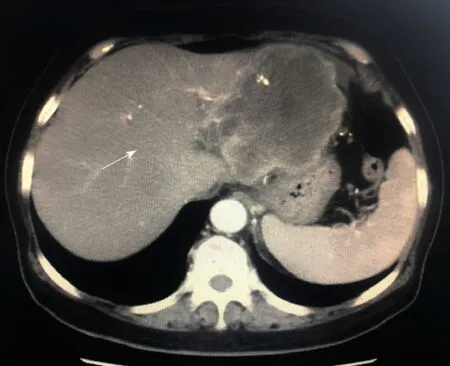
Figure 2 Computerized tomography image showing a 9.3-cm focal hepatic mass in the left lobe of the liver and dilatation of intrahepatic bile duct, as indicated by the arrow.
Figure 2 with actively evolving tumor treatment modalities and concepts, and knowing that optimal efficacy can rarely be achieved by a single treatment regimen, surgerycentered multidisciplinary team as a collaborative health care model has been increasingly recognized[24], which may also benefit patients in this situation. In short,different factors that influence leukocyte elevation and tumor progression should be considered to understand their pathogenesis and to devise effective strategies for their clinical management.
As evidenced by our case, patients with malignant tumors should consider the possibility of PLR in the presence of persistently unexplained elevated levels of WBC.Nonetheless, the association of SHC with leukemoid reaction could not be concluded due to the limited data and care reports, but a prompt diagnostic approach to identify the underlying cause and early application of the most effective treatment might result in a better prognosis for such patients.
CONCLUSION
This is a rare case of SHC combined with PLR, both of which had carried an extremely poor prognosis and had been associated with shorter postoperative survival periods.
ACKNOWLEDGMENTS
We would like to express our gratitude to the participants of the study, and to Dr.Hai-Tao Zhao for his contributions in preparing the manuscript.

Figure 3 lllustration of the clinical course of body temperature and white blood cell counts during the second hospitalization.

Figure 4 Microscopic image of the tumor showing poorly differentiated malignant cells suggestive of SHC.
 World Journal of Clinical Cases2019年11期
World Journal of Clinical Cases2019年11期
- World Journal of Clinical Cases的其它文章
- Huge primary dedifferentiated pancreatic liposarcoma mimicking carcinosarcoma in a young female: A case report
- Multiple synchronous anorectal melanomas with different colors: A case report
- Development of a biliary multi-hole self-expandable metallic stent for bile tract diseases: A case report
- Lupus enteritis as the only active manifestation of systemic lupus erythematosus: A case report
- Application of pulse index continuous cardiac output system in elderly patients with acute myocardial infarction complicated by cardiogenic shock: A prospective randomized study
- Clinical features of syphilitic myelitis with longitudinally extensive myelopathy on spinal magnetic resonance imaging
