髋关节外科脱位技术在髋关节手术的临床应用效果及对髋关节功能、预后的影响
唐立群

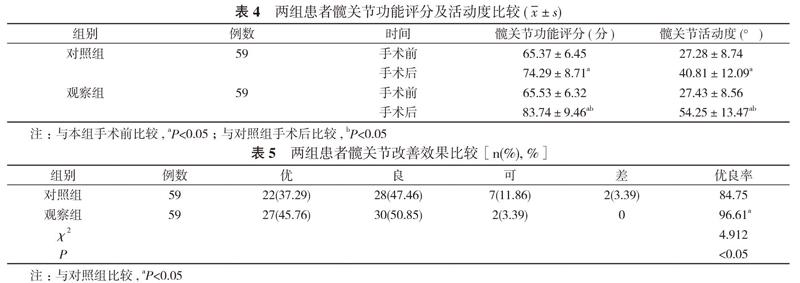
【摘要】 目的 探討髋关节外科脱位技术在髋关节手术中的临床应用效果及对患者髋关节功能、预后的影响。方法 118例行髋关节手术治疗的股骨头坏死患者, 按照随机数字表法分为对照组和观察组, 每组59例。两组患者均实施死骨清理打压植骨治疗, 对照组选择直前入路, 观察组应用髋关节外科脱位技术, 比较两组的术后并发症发生情况、术后疼痛评分、血清炎症因子指标水平、髋关节功能评分、髋关节活动度、髋关节改善效果。结果 观察组术后并发症发生率为1.69%, 低于对照组的11.86%, 差异具有统计学意义(P<0.05)。观察组术后8、12、24、48 h时疼痛评分均低于对照组, 差异具有统计学意义(P<0.05)。手术后, 两组患者C反应蛋白(CRP)、白细胞介素-6(IL-6)、降钙素原(PCT)水平均低于本组手术前, 且观察组CRP、IL-6、PCT水平均低于对照组, 差异具有统计学意义(P<0.05)。手术后, 两组患者髋关节功能评分、髋关节活动度均高于本组手术前, 且观察组的髋关节功能评分、髋关节活动度均高于对照组, 差异具有统计学意义(P<0.05)。观察组患者髋关节改善优良率为96.61%, 高于对照组的84.75%, 差异具有统计学意义(P<0.05)。结论 髋关节外科脱位技术应用于股骨头坏死患者的髋关节手术中, 可有效减少术后并发症, 促进髋关节功能恢复, 改善预后。
【关键词】 髋关节手术;股骨头坏死;髋关节外科脱位技术;创伤骨科;髋关节功能;打压植骨
DOI:10.14163/j.cnki.11-5547/r.2019.01.006
【Abstract】 Objective To discuss the effect of hip surgical dislocation in hip surgery and its influence on hip function and prognosis. Methods A total of 118 femoral head necrosis patients treated by hip joint surgery were divided by random number table into control group and observation group, with 59 cases in each group. Both groups were treated with bone clearance and compression and bone grafting. The control group was treated with direct anterior approach, while the observation group was treated with hip joint surgical dislocation technology. Comparison were made on occurrence of postoperative complications, postoperative pain score, serum inflammatory factor index, hip function score, hip joint activity, hip joint improvement between the two groups. Results The observation group had lower incidence of postoperative complications as 1.69% than 11.86% in the control group, and the difference was statistically significant (P<0.05). The observation group had lower pain score in postoperative 8, 12, 24 and 48 h than the control group, and the difference was statistically significant (P<0.05). After operation, both groups had lower C-reactive protein (CRP), interleukin-6 (IL-6), procalcitonin (PCT) levels than those before operation, and the observation group had lower CRP, IL-6, PCT levels than the control group. Their difference was statistically significant (P<0.05). After operation, both groups had higher hip function score, hip joint activity than those before operation, and the observation group had higher hip function score, hip joint activity than the control group. Their difference was statistically significant (P<0.05). The observation group had higher excellent rate of hip joint improvement as 96.61% than 84.75% in the control group, and the difference was statistically significant (P<0.05). Conclusion Application of hip joint surgical dislocation technology in hip joint surgery of patients with femoral head necrosis, can effectively reduce postoperative complications, promote recovery of hip joint function and improve prognosis.

