降钙素原对危重症患者合并脓毒症早期诊断及预后预测的意义
麻微微 蒋永泼

[摘要] 目的 探討降钙素原(PCT)在危重症患者合并脓毒症早期诊断及预后预测的意义。 方法 选取2017年2月~2018年2月我院重症监护病房(ICU)收治的82例全身炎症反应综合征(SIRS)患者为研究对象,根据脓毒症的诊断标准分为脓毒症组(n=42)和非脓毒症组(n=40),在入院第1、3、5天分别检测患者PCT水平、白细胞(WBC)计数、C反应蛋白(CRP)水平以及慢性健康状况Ⅱ(APACHEⅡ)评分。以脓毒症患者来评价患者预后,存活32例(存活组)和死亡10例(死亡组),比较两组患者PCT水平、WBC计数、CRP水平、APACHEⅡ评分,通过受试者工作特征曲线(ROC)来评价差异指标对预后的预测价值。 结果 入院第1、3、5天时,脓毒症组PCT水平和APACHE Ⅱ评分均高于非脓毒症组,差异有统计学意义(P<0.05);脓毒症组WBC计数和CRP水平与非脓毒症组比较无显著差异(P>0.05)。脓毒症中死亡组PCT水平和APACHEⅡ评分均高于存活组,差异有统计学意义(P<0.05);死亡组WBC计数和CRP水平与存活组比较无显著性差异(P>0.05)。PCT水平用于预测患者预后的AUC、敏感性、特异性均高于APACHEⅡ评分。 结论 PCT可用于危重症合并脓毒症患者的早期诊断和预后判断,准确性高,值得临床推广应用。
[关键词] PCT;APACHEⅡ评分;脓毒症;早期诊断;预后
[中图分类号] R459.7 [文献标识码] B [文章编号] 1673-9701(2019)07-0133-04
[Abstract] Objective To investigate the significance of procalcitonin (PCT) in early diagnosis and prognosis of critically ill patients with sepsis. Methods 82 patients with systemic inflammatory response syndrome(SIRS) admitted in the intensive care unit (ICU) of our hospital from February 2017 to February 2018 were selected as subjects. According to the diagnostic criteria for sepsis, they were divided into the sepsis group (n=42) and the non-sepsis group(n=40). The PCT level, white blood cell (WBC) count, C-reactive protein and chronic health status Ⅱ(APACHE Ⅱ) score were measured at 1, 3, and 5 days after admission. Patients with sepsis were evaluated for prognosis, and 32 patients survived(survival group), and 10 patients died(death group). The PCT level, WBC count, CRP level, and APACHE Ⅱ score were compared between the two groups. The receiver operating characteristic curve (ROC) was used to evaluate the predictive value of differential indicators for prognosis. Results On the 1st, 3rd, and 5th day after admission, the PCT level and APACHE Ⅱ score of sepsis group were higher than those of non-sepsis group. The difference was statistically significant(P<0.05). There was no significant difference in WBC count and CRP level between non-septic group and sepsis group(P>0.05). The PCT level and APACHE Ⅱ score of dead patients were higher than those of survivors, and the difference was statistically significant(P<0.05). There was no significant difference in WBC count and CRP level between dead patients and survivors(P>0.05). The AUC, sensitivity, and specificity of PCT levels for predicting patient outcome were higher than that of APACHE Ⅱ scores. Conclusion PCT can be used for early diagnosis and prognosis of critically ill patients with sepsis, with high accuracy and is worthy of clinical application.
[Key words] PCT; APACHE Ⅱ score; Sepsis; Early diagnosis; Prognosis
脓毒症(Sepsis)是指由感染所导致的全身炎症反应综合征(Systemic inflammatory response syndrome,SIRS)[1,2],其发病率较高,全球每年有超过1800万新发脓毒症患者,且随着抗生素的滥用,其发病率不断升高[3,4],是重症监护病房(Intensive care unit,ICU)的主要死因[5],严重威胁危重症患者的生命健康。早期诊断,并及时给予合理的抗感染治療,可改善患者的预后[6,7]。降钙素原(Procalcitonin,PCT)属于蛋白质,当体内严重细菌、寄生虫、真菌感染时,多器官功能衰竭时期水平升高,可反映体内炎症反应的活跃度[8],比传统白细胞(White blood cell,WBC)计数、C反应蛋白(C-reactive protein,CRP)[9]水平具有更高的特异性和敏感性,临床上广泛应用于感染性疾病的诊断中。本研究旨在探讨降钙素原(PCT)在危重症患者合并脓毒症早期诊断及预后预测的意义,现报道如下。
1 资料与方法
1.1 一般资料
选取2017年2月~2018年2月我院重症监护病房(ICU)收治的82例全身炎症反应综合征(SIRS)患者为研究对象,根据脓毒症的诊断标准[10]分为脓毒症组(n=42)和非脓毒症组(n=40)。脓毒症患者入选标准:符合SIRS诊断标准,并通过血、尿、痰培养和/或胸片检查确认有感染,主要为呼吸系统、泌尿系统感染;非脓毒症患者选标准:符合SIRS诊断标准,但没有感染证据,主要为创伤、心脑血管、中毒等疾病。排除标准:①住院时间<24 h者;②入院前1周内有手术史、急性胰腺炎史、外伤史、烧伤史等;③糖尿病者;④肿瘤病史或免疫抑制剂治疗史;⑤中毒史。其中,脓毒症组男24例,女18例,年龄24~71岁,平均(51.5±5.7)岁;非脓毒症组男25例,女17例,年龄23~68岁,平均(50.9±5.5)岁。两组患者在性别、年龄等一般资料上无显著差异(P>0.05),具有可比性。
1.2 方法
所有患者在入院第1、3、5天分别检测患者PCT水平、WBC计数、CRP水平以及慢性健康状况Ⅱ(APACHEⅡ)评分。检测方法:采集静脉3 mL,采用EDTA进行抗凝,3000 r/min的速率离心15 min,取500 μL上清液,利用梅里埃公司VIDAS全采用自动酶联荧光分析仪,通过免疫荧光法测定PCT水平,检测最低浓度范围为(0.06~200.00)ng/L;通过免疫比浊法测定CRP水平;通过自动分析仪检测WBC计数。以PCT≥0.5 ng/mL,CRP>10 mg/mL,WBC>10×109/L作为诊断脓毒症的标准。APACHEⅡ评分根据患者一般资料(性别、年龄、血压、呼吸、体温、心率、血尿常规、电解质水平、肝功能、肾功能、胸片等)以及脓液、血、尿、支气管分泌物、腹水等培养进行评分。比较脓毒症患者和非脓毒症患者,以及脓毒症患者中存活患者和死亡患者PCT水平、WBC计数、CRP水平、APACHEⅡ评分;通过ROC来评价PCT水平与APACHEⅡ评分在判断预后中的价值。
1.3 统计学处理
采用SPSS18.0统计学软件进行分析,计数资料以[n(%)]表示,采用χ2检验,计量资料以(x±s)表示,采用t检验;运用ROC曲线来评价观察标判断预后的能力。P<0.05为差异有统计学意义。
2 结果
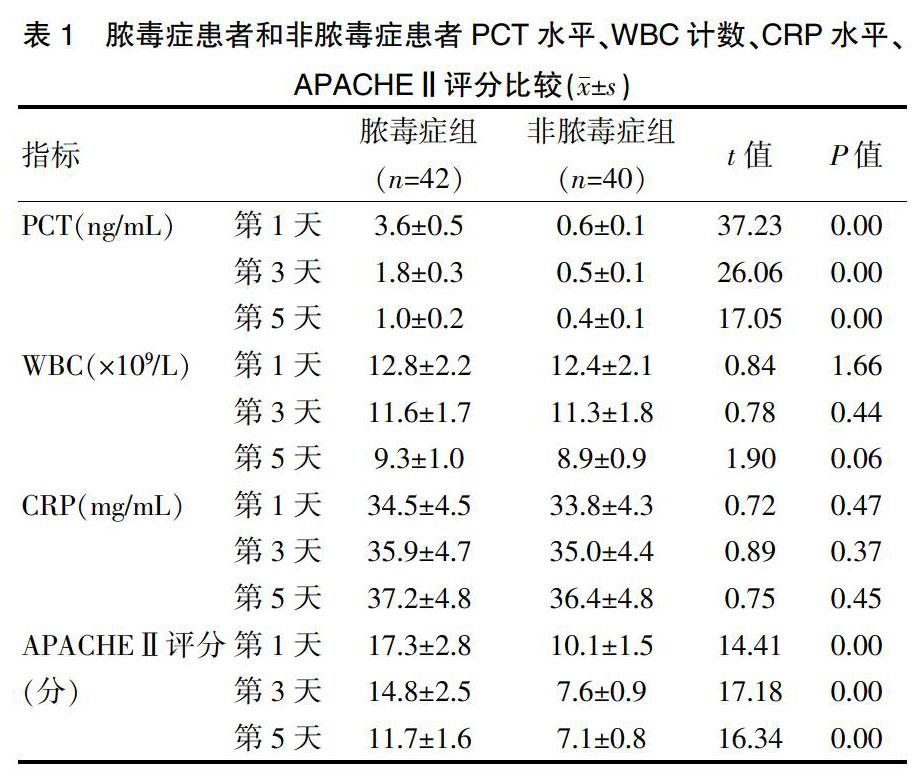
2.1 脓毒症组和非脓毒症组PCT水平、WBC计数、CRP水平、APACHEⅡ评分比较
入院第1、3、5天时,脓毒症组PCT水平和APACHEⅡ评分均高于非脓毒症组,差异有统计学意义(P<0.05);脓毒症组WBC计数和CRP水平与非脓毒症组比较无显著差异(P>0.05),见表1。
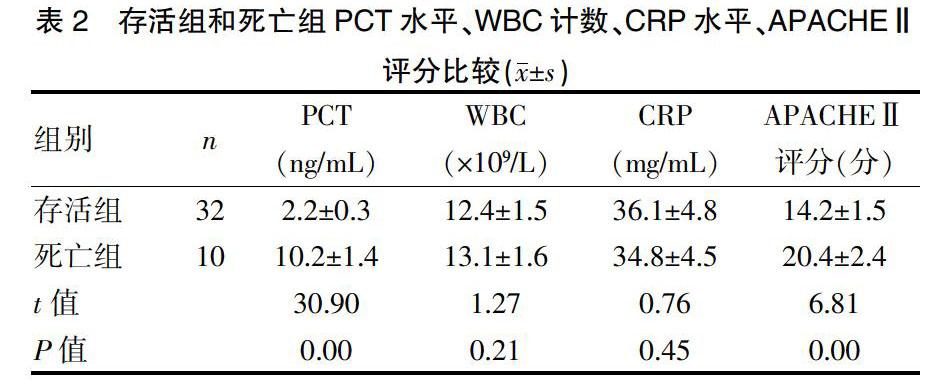
2.2 存活组和死亡组PCT水平、WBC计数、CRP水平、APACHEⅡ评分比较
脓毒症患者出院时,共有32例患者存活,10例患者死亡;其中死亡组PCT水平和APACHEⅡ评分均高于存活组,差异有统计学意义(P<0.05);死亡组WBC计数和CRP水平与存活组比较无显著差异(P>0.05),见表2。
2.3 PCT水平、APACHEⅡ评分在判断预后中的价值
PCT水平、APACHEⅡ评分在存活患者和死亡患者中有显著差异,通过进一步ROC曲线分析,PCT水平用于预测脓毒症患者死亡的AUC为0.872,APACHEⅡ评分用于预测脓毒症患者死亡的AUC为0.758,且PCT水平用于预测患者预后的敏感性和特异性均高于APACHEⅡ评分,见表3。
3 讨论
脓毒症是临床上危重症患者死亡的最常见的原因之一[11,12],近年来,随着医学的发展、细菌耐药性的增加、侵损性操作的增加、放化疗患者以及器官移植术的增加,脓毒症的发病率不断增高,严重威胁患者的生命健康,因此早期诊断、及时介入治疗对提高患者的生存率非常重要[13,14]。临床监测感染的指标主要有体温、血液学检查、病原学检查、细胞因子等[15],但对于脓毒症检测缺乏灵敏性和特异性,临床上难以获取准确信息,导致脓毒症的死亡率高达30%~70%。细菌培养对于诊断脓毒症的准确性较高,但时耗较长,不能给予早期指导治疗,临床疗效较差[16]。因此,寻找一种快速的、灵敏的、特异的诊断指标成为医务人员的当务之急。
近年来,在脓毒症的诊断方面,发现PCT是一个有潜力的生物学指标[17]。PCT是一种无激素活性的蛋白质,属于降钙素前肽物质,由2800个碱基、116个氨基酸对组成,其相对分子质量为13 000,半衰期为22~29 h,稳定性较高,不易降解,且PCT的检测不易受治疗的影响[18]。PCT在健康人血清中含量极少,在细菌感染时,血清中的PCT水平明显升高,诊断脓毒症的界值为>0.5 ng/mL,严重脓毒症患者PCT浓度可达到(5~50)ng/mL[19]。当机体处于严重细菌感染状态时,患者体内PCT浓度可明显升高,且感染的严重程度与PCT升高程度呈正相关,而CRP的浓度不会升高[20,21]。与CRP、WBC相比,PCT在细菌感染的鉴别和诊断上具有较高的临床价值。在本研究中,入院第1、3、5天时,脓毒症患者PCT水平和APACHEⅡ评分均高于非脓毒症患者,差异有统计学意义(P<0.05);脓毒症患者WBC计数和CRP水平与非脓毒症患者比较无显著差异(P>0.05)。脓毒症中死亡患者PCT水平和APACHEⅡ评分均高于存活患者,差异有统计学意义(P<0.05);死亡患者WBC计数和CRP水平与存活患者比较无显著差异(P>0.05)。通过ROC分析,PCT水平用于预测患者预后的AUC、敏感性、特异性均高于APACHEⅡ评分。
本研究仍然有不足之处:①由于是单中心研究,入选病例有限,在今后的研究中,可通过多中心合作,加大样本量,进一步验证本研究结论;②PCT、WBC、CRP水平的检测都是收集病例后进行,血液通过低温保存,可能会影响检测结果。但研究结果显示,PCT是一个高特异性、高敏感性的脓毒症早期诊断指标,可通过与WBC、CRP、APACHEⅡ评分联合检测,提高早期诊断的准确性;PCT与APACHEⅡ评分联合检测,有利于脓毒症预后的判断。
综上所述,PCT可用于危重症合并脓毒症患者的早期诊断和预后判断,准确性高,值得临床推广应用。
[参考文献]
[1] Cobussen M,Havenith T,Posthouwer D,et al. Short course of empirical Gentamicin in patients with severe sepsis and septic shock in the ICU:A benefit or a burden?[J]. Clin Infect Dis,2017,65(5): 873-874.
[2] Fang X,Wang Z,Yang J,et al. Clinical evaluation of sepsis-1 and sepsis-3 in the ICU[J]. Chest,2018,153(5):1169-1176.
[3] Goulden R,Hoyle MC,Monis J,et al. qSOFA,SIRS and NEWS for predicting in hospital mortality and ICU admission in emergency admissions treated as sepsis[J]. Emerg Med J, 2018,35(6):345-349.
[4] Huda AQ,Karim MR,Mahmud MA,et al. Use of acute physiology and chronic health evaluation (APACHE)-Ⅱ and red cell distribution width (RDW) for assessment of mortality of patients with sepsis in ICU[J]. Mymensingh Med J,2017,26(3): 585-591.
[5] Burrell A, Huckson S,Pilcher DV. ICU admissions for sepsis or pneumonia in Australia and New Zealand in 2017[J]. N Engl J Med,2018,378(22):2138-2139.
[6] Layios N,Delierneux C,Hego A,et al. Sepsis prediction in critically ill patients by platelet activation markers on ICU admission:A prospective pilot study[J]. Intensive Care Med Exp,2017,5(1):32.
[7] Mao Q,Jay M,Hoffman JL,et al. Multicentre validation of a sepsis prediction algorithm using only vital sign data in the emergency department,general ward and ICU[J]. BMJ Open,2018,8(1):e017833.
[8] Verma N,Kapoor S,Rao D,et al. PCT as a prognostic marker in cardiac patients with neutropenic sepsis:Two case reports[J]. Indian J Clin Biochem,2014,29(1):107-110.
[9] Shabuj KH, Hossain J, Moni SC, et al. C-reactive protein (CRP) as a single biomarker for diagnosis of neonatal sepsis: A comprehensive meta-analysis[J]. Mymensingh Med J,2017,26(2):364-371.
[10] 范遠华,朱华勇,张敏,等. 脓毒症患者血清降钙素原测定对诊断和病情评估临床研究[J]. 现代诊断与治疗,2014,25(24):5662-5663.
[11] Nakayama I,Izawa J,Mouri H,et al. Mortality and detailed characteristics of pre-ICU qSOFA-negative patients with suspected sepsis:An observational study[J]. Ann Intensive Care,2018,8(1): 44.
[12] Nemati S,Holder A,Razmi F, et al. An interpretable machine learning model for accurate prediction of sepsis in the ICU[J]. Crit Care Med,2018,46(4):547-553.
[13] Papp M. Response to low L-Ficolin associated with disease severity during sepsis in adult ICU patients[J]. Liver Int,2017,37(9):1410.
[14] Umemura Y, Ogura H, Gando S, et al. Assessment of mortality by qSOFA in patients with sepsis outside ICU:A posthoc subgroup analysis by the Japanese Association for Acute Medicine Sepsis Registry Study Group[J]. J Infect Chemother,2017, 23(11): 757-762.
[15] Zorio V,Venet F,Delwarde B,et al. Assessment of sepsis-induced immunosuppression at ICU discharge and 6 months after ICU discharge[J]. Ann Intensive Care,2017, 7(1):80.
[16] Scicluna BP,Wiewel MA,van Vught LA,et al. Molecular biomarker to assist in diagnosing abdominal sepsis upon ICU admission[J]. Am J Respir Crit Care Med,2018,197(8):1070-1073.
[17] Liu Y,Yang W,Wei J. Guiding effect of serum procalcitonin(PCT) on the antibiotic application to patients with sepsis[J]. Iran J Public Health,2017,46(11):1535-1539.
[18] Cabral L,Afreixo V,Almeida L,et al. The use of procalcitonin (PCT) for diagnosis of sepsis in burn patients: A meta-analysis[J]. PLoS One,2016,11(12): e0168475.
[19] Yang AP,Liu J,Yue LH,et al. Neutrophil CD64 combined with PCT, CRP and WBC improves the sensitivity for the early diagnosis of neonatal sepsis[J]. Clin Chem Lab Med,2016,54(2):345-351.
[20] Elliott TS,Casey AL,Karpanen TJ,et al. Addition of PLA2 to CRP enhances sepsis diagnosis[J]. J Infect,2016, 73(4): 386-388.
[21] Ganesan P,Shanmugam P,Sattar SB,et al. Evaluation of IL-6,CRP and hs-CRP as early markers of neonatal sepsis[J]. J Clin Diagn Res,2016,10(5):DC13-DC17.
(收稿日期:2018-07-06)