Shoshin syndrome: report of a treatable disaster
Tommaso Valobra
, Umberto Ceratti, Alessandra Cernuschi
Medical High Dependency Unit, Department of Medicine, Ospedale Niguarda Ca' Granda, Milano, Italy
Keywords:Thiamine Shoshin Beriberi Wernike Alcoholic
ABSTRACT Shoshin syndrome is a rare fulminating heart failure caused by thiamine deficiency. In Japanese “sho” means acute damage and “shin” means heart. It consists of a rare and hyperacute manifestation of beriberi that was first described in polished white rice-eating communities in various locations across Asia including China, Japan and Indonesia. In a totally different context, ‘Shoshin’ is a word from Zen Buddhism meaning "beginner's mind”, which is considered the necessary attitude to approach the Zen practice. This case report is a prime example of clinical manifestations of thiamine deficiency for the presence of both cardiological and neurological disorders, for hyperacute onset of cardiac failure (shoshin syndrome), for the simultaneous involvement of peripheral and central nervous system, and for the dramatic global recovery after thiamine replacement therapy. We therefore explain why the physician should adopt a beginner’s mind in clinical practice.
1. Introduction
Vitamin B1, also known as thiamine, is an essential B vitamin,which must be necessarily ingested because the human body is not capable of producing it. Its storage occurs in liver and its absorption in duodenum. Its conversion to thiamine pyrophosphate, the activated form, is mediated by an enzyme that requires magnesium as a cofactor; this explains why sometimes hypomagnesaemia can manifest clinical features similar to thiamine deficiency[1].
Thiamine pyrophosphate is a cofactor that is required for many biochemical pathways; for example, it is fundamental for the activity of two Krebs cycle enzymes: pyruvate dehydrogenase complex and alpha-ketoglutarate dehydrogenase.
In case of thiamine deficiency, pyruvate dehydrogenase is unable to produce acetyl-CoA from pyruvate, causing an interruption of oxidative reactions in Krebs cycle and a consequent reduction in the production of adenosine triphosphate[2]. This finally results in a reduction of oxygen consumption in various tissues with consequent multiple organ failure. This phenomenon is of particular concern for heart and brain, due to their high mitochondrial content and metabolic demand[3].
Thiamine deficiency is rarely observed in developed countries and is most commonly associated with chronic alcohol abuse.Other predisposing conditions include chronic dietary malnutrition and impaired absorption or intake of dietary nutrients[4]. Prompt clinical detection of thiamine deficiency is a difficult task because symptoms can be vague and nonspecific[1].
2. Case report
A 50-year-old man with no specific medical history was admitted to our Emergency Department (ED) by ambulance. Firefighters’intervention was necessary to have access to his home after a warning from his neighbour who saw him struggling on the terrace of his house. Informed consent was obtained from all individual participants involved in the study.
Upon arrival in our ED, the patient was tachycardic at 155 beats/min, febrile (38.5 ℃), with a blood pressure of 135/85 mmHg,a respiratory rate of 26 breaths/min and an oxygen saturation of 85% with room air and of 98% with a 6 L/min oxygen flow; his fingerstick glucose was 164 mg/dL. The man was apparently awake but unresponsive, the rest of the physical examination was unremarkable except for rhythmic tachycardia; electrocardiography showed sinus tachycardia and no features suggestive of myocardial ischemia (Figure 1). The arterial blood gas did not reveal significant pH disturbance (pH was 7.41 with pCO238 mmHg), but was remarkable for lactate of 3.8 mmol/L.
Laboratory-tests were notable for creatine phosphokinase at 438 U/L (normal range 30 U/L-200 U/L), mean corpuscular volume 104 fL (normal range 82 fL-97 fL), haemoglobin of 13.3 g/dL,platelet count of 60×109/L (reference range 140 to 440), alanine aminotransferase 92 U/L (reference range 3-45). The haemostatic parameters and kidney function tests were normal.
X-ray examination showed congested lung field and a possible basal consolidation like pneumonia (Figure 2). Alcohol levels were undetectable and urine toxicology screen was negative.
The patient underwent brain computer tomography and computed tomography angiography which were negative for brain injury and arterial occlusion, respectively. A chronic alcohol dependency was suspected on the basis of past hospital admissions for acute alcohol intoxications, therefore intramuscular thiamine 500 mg was empirically administered. Vitamins level was not tested on admission, but it was normal a few days after the treatment beginning.
A 2-L normal saline bolus was initially infused, but in a few hours the patient’s hemodynamic and respiratory status rapidly deteriorated, requiring intensive care unit admission and endotracheal intubation with ventilator support.
A transthoracic echocardiography showed a left ventricular ejection fraction of 15% and moderate mitral incompetence (Figure 3),and the patient required epinephrine infusion for hemodynamic support. However, due to marked hemodynamic instability,anuria, and persistent manifestations of heart failure, an intraortic balloon pump was inserted, and later venoarterial extracorporeal membrane oxygenation was initiated using a 25 French right femoral vein and a 19 French right femoral artery. The patient did not undergo a coronary angiography in consideration of negative electrocardiography without significant increase of the markers of myocardial necrosis; he was in fact suspected to suffer of a dilated cardiomyopathy precipitated by a community-acquired pneumonia.Meanwhile, a detailed clinical history was obtained from a relative.Recent history revealed that the patient was a chronic alcohol abuser,especially he increased alcohol intake in the previous months, for he was separated from his wife, and fired from work.
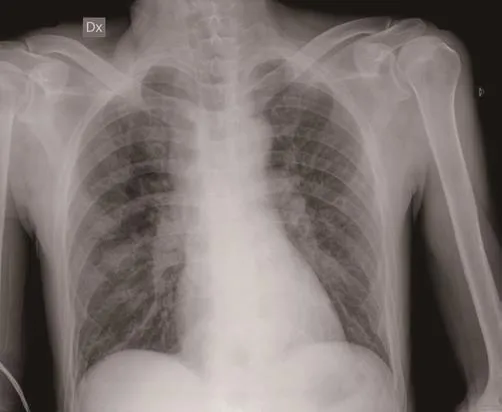
Figure 2. X-ray examination showing congested lung field and a possible basal consolidation as for pneumonia.
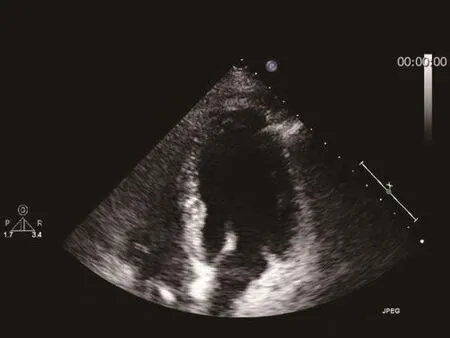
Figure 3. A transthoracic echocardiography exhibited a severe global impairment of left ventricular wall motion.
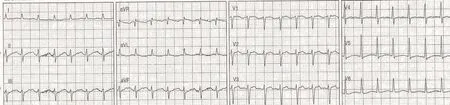
Figure 1. On admission the electrocardiography showed sinus tachycardia and no features suggestive of myocardial ischemia.
Considering the persistent hemodynamic deterioration refractory to extra corporeal membrane oxygenation support and the history that was positive for alcohol abuse, “shoshin beriberi”, the fulminant form of cardiovascular beriberi caused by thiamine deficiency,was suspected. Thus, daily thiamine intravenous administrations were performed and after 72 h from admission his respiratory and haemodynamic state improved. The patient no longer required inotropic support and was weaned off vasopressor and mechanical ventilation. At first, pneumonia was empirically treated with ceftriaxone and azithromycin, and after the isolation of Pseudomonas aeruginosa from bronchoaspiration it was treated efficaciously with meropenem. Different sets of blood coltures resulted negative like the urinary pneumococcal and legionella antigen detection tests.
After sedative drugs were stopped, the patient presented an acute delirium with agitation, confusion and confabulation that continued during his recovery in the internal medicine unit where he was transferred after clinical stabilization. Psychomotor agitation was particularly difficult to treat with antipsychotic drugs, requiring sedation therapy and physical contention in order to guarantee the patient’s safety. Oral thiamine was administered daily and after about one month from admission the patient began to improve his neuropsychiatric condition. He gradually appeared calmer, more compliant, and improved his phatic and cognitive functions; however,he presented retrograde amnesia since the day of his sudden illness at home. He was therefore transferred to the rehabilitation care unit for physical and logopaedic therapy in a good general health conditions. In this setting, a foot drop with typical steppage gait was observed as result of peroneal neuropathy, then confirmed by electrophysiological tests.
3. Discussion
Thiamine deficiency has various clinical manifestations which have been described in the literature since 17thcentury. The term “beriberi”was initially chosen to describe the sheep-like walk of malnourished southeast Asian inhabitants whose diet was based on polished rice,which is deficient in vitamin B1. This syndrome, characterized by peripheral neuropathy, muscle weakness, and anorexia, is also called “dry” beriberi to differentiate it from “wet” beriberi, which is essentially a cardiovascular manifestation[5]. Nutritional amblyopia and gastrointestinal tract symptoms related to delayed emptying are other conditions described in adult thiamine deficiency[6].
The main cardiovascular signs of acute thiamine deficiency are high-output heart failure, marked peripheral oedema, raised jugular venous pressure, and severe lactic acidosis, because the accumulation of pyruvate causes intense vasodilatation due to peripheral arteriovenous shunts in the skeletal musculature[4]. A less common clinical presentation consist of a fulminating heart failure with evidence of a low cardiac output; this form has been given the name “shoshin” beriberi or shoshin syndrome[7]. It has previously been described as “a rapidly curable hemodynamic disaster” that,if not timely recognized and promptly treated, can result in rapid hemodynamic collapse and death[8].
Thiamine deficiency also leads to brain lesions, which usually occur in selected and vulnerable regions with high thiamine turnover causing Wernicke’s encephalopathy (WE), an acute,neuropsychiatric syndrome that is a common relative of other neurological disorders[9]. The patients with WE can manifest a classical triad: ophthalmologic disturbances, ataxic gait, and altered mental status. Approximately 80%-90% of alcoholics with WE who are treated with inappropriately low parenteral doses of thiamine develop irreversible Korsakoff’s psychosis, a long-lasting debilitating condition characterised by confabulation and short-term memory loss[10]. A decrease in blood concentration of vitamin B1could be a key to diagnose beriberi. However, in some cases, patients can suffer from beriberi despite no exceedingly low (and sometimes even normal) levels of thiamine measured on whole blood[11].
Blood contains only about 0.8% of the total body thiamine, and the concentration is too low to allow precise extrapolation of the global thiamine status[6]. At present the only reasonable way to establish the diagnosis of beriberi in the emergency department includes taking a good history, looking out for causes of thiamine deficiency, making a thorough physical examination searching for expected signs, and monitoring the response to therapy[12].
We reported a likely case of shoshin syndrome with WE and peripheral neuropathy, which was probably precipitated by an acute community-acquired pneumonia and promptly considered and treated for high clinical suspicion. Upon admission, patient’s extremities were perfused and oedema was absent, but marked congestive heart failure, sinus tachycardia and severe lactic acidosis were detected. Systemic vascular resistance was noted to be low,which is an unexpected finding in a cardiogenic shock; this aspect can be attributed to the direct effects of thiamine deficiency on vasomotor tone as in previously reported[13].
The hypothesis of alcoholic cardiomyopathy seemed unlikely because in this case the dramatic improvement of left ventricular function is significant usually after 6 months of treatment[14].
In our patient, WE appeared as delirious agitation, confusion and confabulation, which continued for several days.
In the differential diagnosis of acute delirium in an alcoholic malnourished critically ill patient, physician must consider sedative withdrawal, delirium tremens, hepatic encephalopathy,hypophosphatemia related to refeeding syndrome and anoxic brain injury[10].
Nevertheless, intramuscular thiamine was given to the patient at the time of admission to the emergency room because the benefit-risk balance of treatment is definitely positive considering that a missed diagnosis of WE has a high morbidity and mortality rate[12].
Thiamine must be administered before or concomitantly with intravenous administration of glucose, because the vitamin itself can precipitate the disorder in thiamine-deficient individuals such as alcoholics who are frequently calorically deficient and are hypoglycemic on initial evaluation[5,9]. Some evidence suggests, therefore, that magnesium could be helpful in thiamine utilization, and empirical supplementation of magnesium may be indicated[4]. Even short-term use of loop diuretics could induce thiamine deficiency via inhibiting its reabsorption[2]; furthermore,in high output states associated with decreased peripheral vascular resistance, like beriberi, the use of vasodilator therapy and positive inotropic for treatment of congestion may aggravate the problem.
This case is a prime example of clinical manifestations of thiamine deficiency for the presence of both cardiological and neurological disorders, for hyperacute onset of cardiac failure (shoshin syndrome),for the simultaneous involvement of the peripheral and central nervous system, and for dramatic global recovery after thiamine replacement therapy.
We observed that recovery can occur with different timing for reversable injury in the central nervous system and cardiovascular apparatus, and in our experience unexpected neurological recovery after some weeks of severe cognitive impairment seemed to be prodigious. When the patient was able to walk, his gait showed a clinical manifestation of dry beriberi, characterized even by a progressive axonal sensorimotor peripheral neuropathy.
4. Conclusion
Thiamine deficiency can cause acute and severe clinical illness like beriberi, shoshin syndrome and WE. Despite the difficulty of rapidly ensuring diagnosis for the variety of non-specific clinical manifestations and the lack of useful diagnostic tool, the physician must have a high index of clinical suspicion considering the predisposing factors and the conditions associated with thiamine deficiency. He must therefore monitor the response to therapy. Adequate doses of parenteral thiamine must be promptly administered considering morbidity and mortality of a missed diagnosis. Magnesium supplementation can be required, as well.
In the present case, thiamine supplementation remarkably reversed both profound cardiovascular collapse and neurological impairment although with different timing.
Finally, it’s interesting to note that, in a totally different context,‘shoshin’ is a word from Zen Buddhism meaning “beginner’s mind”,considered the necessary attitude to approach the zen practice. “In the beginner’s mind, an empty and ready mind, there are many possibilities”. “The beginner’s mind is the mind of compassion, too.When our mind is compassionate, it is boundless.”[15]. This state of mind is the same for a physician who has a high clinical suspicion and considers every eventuality, avoiding stigmatizing attitudes.
This concept even reminds the physician of the importance of empathetic care for these patients who frequently experience,in addition to illness, difficult social or familial situations. A compassionate approach, caring for human dignity and integrity,promotes health and well-being despite the illness.
Conflict of interest statement
The authors report no conflict of interest.
Acknowledgement
We gratefully thank Dr. Chiara Piagnani for performing language editing and proofreading.
 Journal of Acute Disease2019年2期
Journal of Acute Disease2019年2期
- Journal of Acute Disease的其它文章
- Tardive phenomenon presenting as isolated dysarthria: A rare entity mimicking stroke
- Long-term diabetes-related severe complications among individuals with T2DM in Jazan, Saudi Arabia
- Polymorphism of hypoxia-inducible factor-1α gene in pediatric acute respiratory distress syndrome
- Characterization and frequency of antibiotic resistance related to membrane porin and efflux pump genes among Acinetobacter baumannii strains obtained from burn patients in Tehran, Iran
- The red cell distribution width to platelet ratio predicts 30-day mortality of acute pulmonary embolism patients
- Distribution of extended-spectrum β-lactamase genes in antibioticresistant strains of Pseudomonas aeruginosa obtained from burn patients in Ahvaz, Iran
