The red cell distribution width to platelet ratio predicts 30-day mortality of acute pulmonary embolism patients
Meliha Findik, Cemil Kavalci, Afsin Emre Kayipmaz, Murat Muratoglu, Elif Kilicli
Baskent University Faculty of Medicine, Department of Emergency, Ankara, Turkey
Keywords:Biochemical markers Emergency treatment Pulmonary thromboembolism
ABSTRACT Objective: To specify the clinical and sociodemographic characteristics, risk factors, factors affecting mortality including hematologic parameters, and red blood cell distribution width to platelet ratio (RPR) in patients with pulmonary thromboembolism, and to reduce the mortality. Methods: The archive records of patients diagnosed with pulmonary embolism were retrospectively examined. The histories, risk factors, physical examination findings, arterial blood gas analysis, X-rays, laboratory, and computed tomography reports of all cases were obtained via the hospital information system. Logistic regression analysis was performed to determine the independent variables affecting early mortality. Results: A total of 146 patients with a definitive diagnosis of pulmonary thromboembolism were included. Thirteen point seven percent (n=20) of the deceased patients died at early term. Ninety percent of patients with early mortality was 65 years or older. There were significantly differences in age, RPR, D-dimer,creatinine, lymphocyte, pH, and body temperature between patients with and without early mortality (P=0.017, P<0.001, P=0.019, P=0.025, P=0.042, P=0.013, P=0.017, respectively).Logistic regression analysis showed that RPR was a statistically significant and independent risk factors of mortality [P=0.026, OR: 0.254., 95% CI (0.326-5.056)]. In addition, there was a significant difference in pulmonary embolism severity index classification between patients with and without early mortality(P<0.034). Conclusions: RPR is an independent risk factor of mortality of pulmonary embolism patients and may help emergency physician to stratify mortality risks of pulmonary embolism patients.
1. Introduction
Acute pulmonary embolism has an essential role among emergency visits due to its morbidity and mortality[1]. Pulmonary embolism occurs due to deep venous thrombosis caused by venous stasis, hypercoagulability and vessel damage[2]. It is known that the clinical properties of the patients with acute pulmonary embolism are related to mortality[3]. It has been reported that acute pulmonary embolism has a higher mortality rate in the elderly than young patients[4]. Early diagnosis and treatment has shown to be the most critical components in reducing the mortality and morbidity of pulmonary embolism[5]. Previous studies showed immobility,tachycardia, hypotension, troponin T elevation, underlying coronary artery disease, cerebrovascular disease, massive-size pulmonary embolism, bilateral pulmonary embolism, possible pulmonary embolism in Wells scoring, and possible pulmonary embolism in Modified Geneva scoring to be related with early mortality[6]. Other studies on this subject showed that the most common symptom was dyspnea and the most critical risk factor was immobility[7].
It has been suggested that red blood cell distribution width to platelet ratio (RPR) is a new biomarker that can be used to demonstrate the severity and mortality of various diseases. For instance, Xie et al.[8] have reported that RPR can be used as a biomarker in describing the activity of systemic lupus erythematosus in their recently published studies. Cetinkaya et al. have also shown that RPR can be used to demonstrate mortality of acute pancreatitis[9]. Chen et al. found that RPR is a strong predictor of the degree of fibrosis and cirrhosis in patients with chronic hepatitis[10].Pusuroglu et al. investigated the 1-year mortality of ST-segment elevation myocardial infarction. The authors showed that high RPR at admission was an independent predictor of this[11].
From these examples, RPR has been shown to be a useful biomarker in demonstrating inflammation in various diseases.However, according to our knowledge, there is currently no published article on the use of RPR to show the early mortality of pulmonary embolism. With this article, we intended to specify the clinical and sociodemographic characteristics, risk factors and the factors affecting mortality including hematologic parameters in patients with pulmonary thromboembolism. Our primary goal was to contribute to the reduction of mortality.
2. Materials and methods
We performed this study after obtaining the ethics committee approval from Baskent University Institutional Review Board for Medicine and Health Sciences (Project Number: KA15/301).
We retrospectively examined the archive records of patients diagnosed with pulmonary embolism between January 2011 and December 2015 in Baskent University Ankara Hospital’s Adult Emergency Department. We obtained the histories, risk factors, physical examination findings, arterial blood gas analysis,conventional X-rays, hematologic & biochemical test results,and computed tomography reports of all cases via the hospital information system. We defined the deaths within the first 30 d after emergency visit as early mortality.
We analyzed the data with “SPSS 17.0 for Windows” program,and expressed the demographic data with the number of patients(n) and percentage (%). We used the χ2test to compare categorical groups; Kolmogorov-Smirnov test to check the normal distribution of continuous variables. We compared continuous variables by using the Mann-Whitney U test and Student’s t-test. logistic regression analysis was did to investigate the factors affecting mortality. The value of P<0.05 was considered to be statistically significant.
3. Results
3.1. General information
The universe of our study consisted of 147 719 patients who applied to the adult emergency department of Baskent University Ankara Hospital between January 1st2011 and December 31th2015.Preliminary diagnosis of 2 398 of these patients was pulmonary thromboembolism. We included 146 patients with a definitive diagnosis of pulmonary thromboembolism.
Of the participants, 59.6% were female (n=87). Sixty-five percent(n=95) of the patients were 65 years and over, and the remaining 35% (n=51) were in the 18-64 age group. Thirty-one point five percent (n=46) pulmonary embolism patients died. Accordingly,13.7% (n=20) of the deceased patients died early term. Ninety percent of patients with early mortality was 65 years or older.
Fifty-five percent of the patients with early mortality were male,and the majority of the patients were female (61.9%) in the other group.
3.2. Risk factors of the patients
Immobility, malignancy, smoking and cardiovascular disease were the most common risk factors for pulmonary embolism. We also found significant difference in age and immobility between patients with and without early mortality (P=0.034 and P=0.003,respectively).
3.3. Co-morbidities
There was statistically significant difference in occurrence of arterial oxygen saturation below 90% between patients with and without early mortality (P=0.084) (Table 1).
The most common symptoms in patients with early mortality were dyspnea, change of consciousness and syncope. Hypertension,Alzheimer’s and chronic obstructive pulmonary disease (COPD)were the most common concomitant diseases of pulmonary thromboembolism in this group (Table 2).
Concerning diseases associated with pulmonary embolism, there was statistically significant difference in morbidity of COPD and Alzheimer’s disease between patients with and without early mortality (P=0.033 and P=0.017, respectively). Also, the occurrence of symptoms of chest pain, syncope, back pain and change of consciousness were also significant between patients with and without early mortality (P=0.016, P=0.002, P= 0.025, P<0.001,respectively) (Table 3).
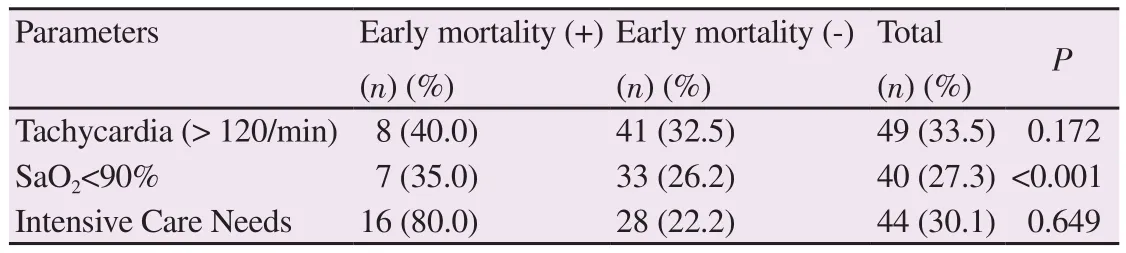
Table 1 Hemodynamic-laboratory parameters and intensive care needs of patients regarding early mortality [n(%)].
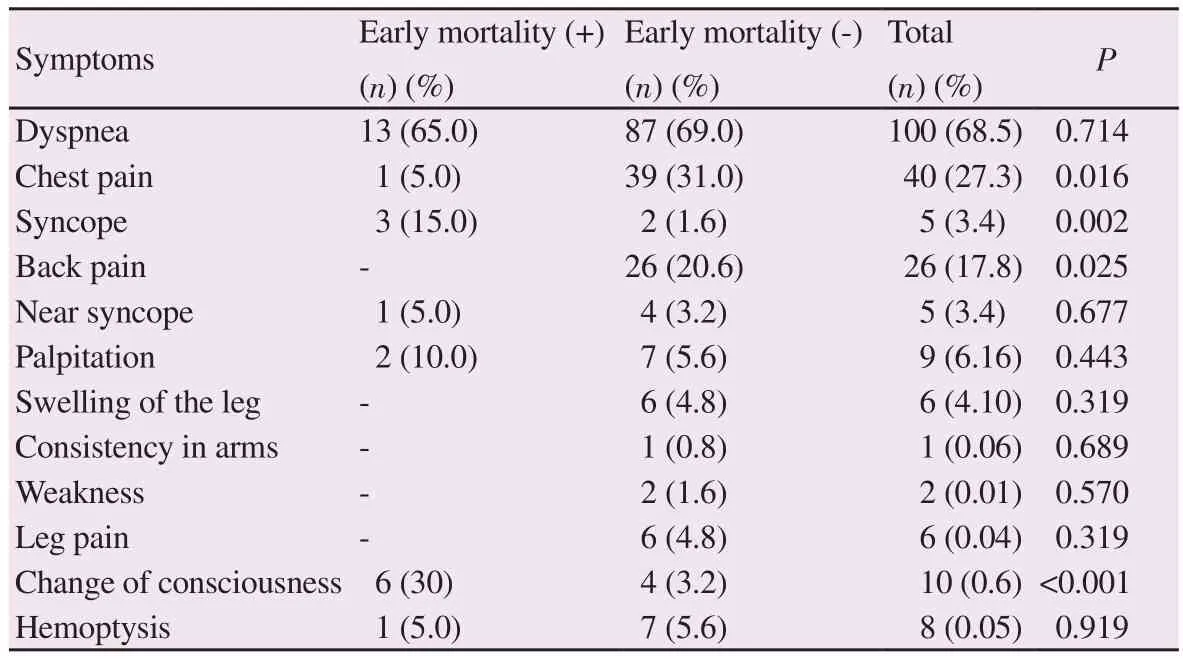
Table 2 Symptoms of patients regarding early mortality [n(%)].
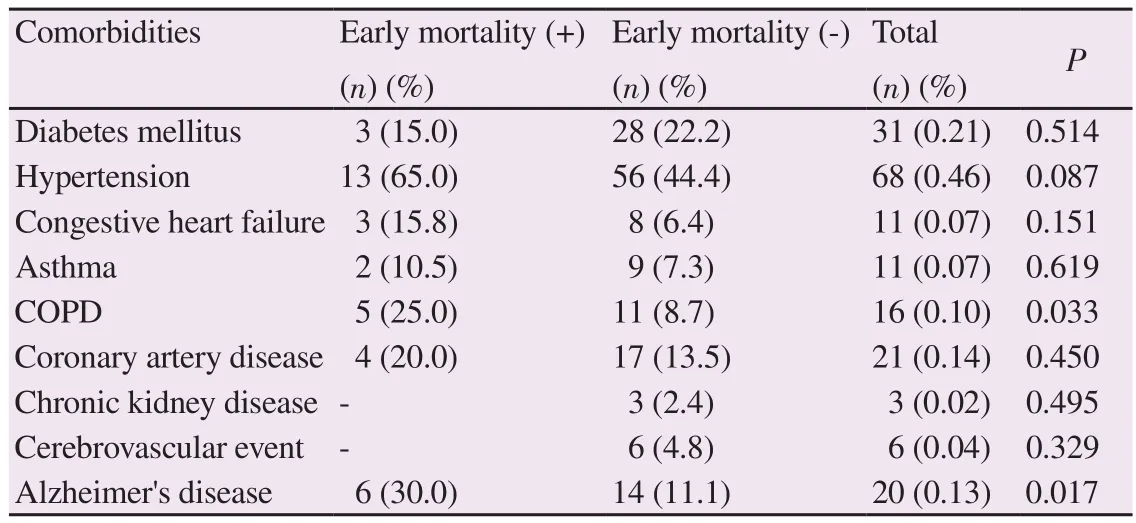
Table 3 Comorbidities of patients regarding early mortality [n(%)].
3.4. Laboratory results
Table 4 showed vital signs, laboratory, and blood gas analysis results of pulmonary embolism patients according to early mortality status. According to this table, there was a significant difference in age, RPR, D-dimer, creatinine, lymphocyte, pH, body temperature between patients with and without early mortality(P=0.017, P<0.001, P=0.019, P=0.025, P=0.042, P=0.013, P=0.017,respectively).
We performed logistic regression analysis (age, RPR, D-dimer,creatinine, lymphocyte, body temperature) to determine the independent variables affecting early mortality. We found that none of them independently affected mortality, except RPR. We found RPR to be an independent predictor of mortality (P=0.022)(Table 5).We compared Wells Scores (low, medium, high-risk groups) of pulmonary embolism patients with early mortality. There was no statistically significant difference between Wells scores of patients(P=0.111) in terms of early mortality.
Table 6 showed pulmonary embolism severity index (PESI) and the simplified PESI (sPESI) classifications of pulmonary embolism patients according to early mortality status. There was a statistically significant difference in risk of PESI classification between patients with and without early mortality (P=0.034). There was no statistically significant difference in sPESI classification (P=0.088).
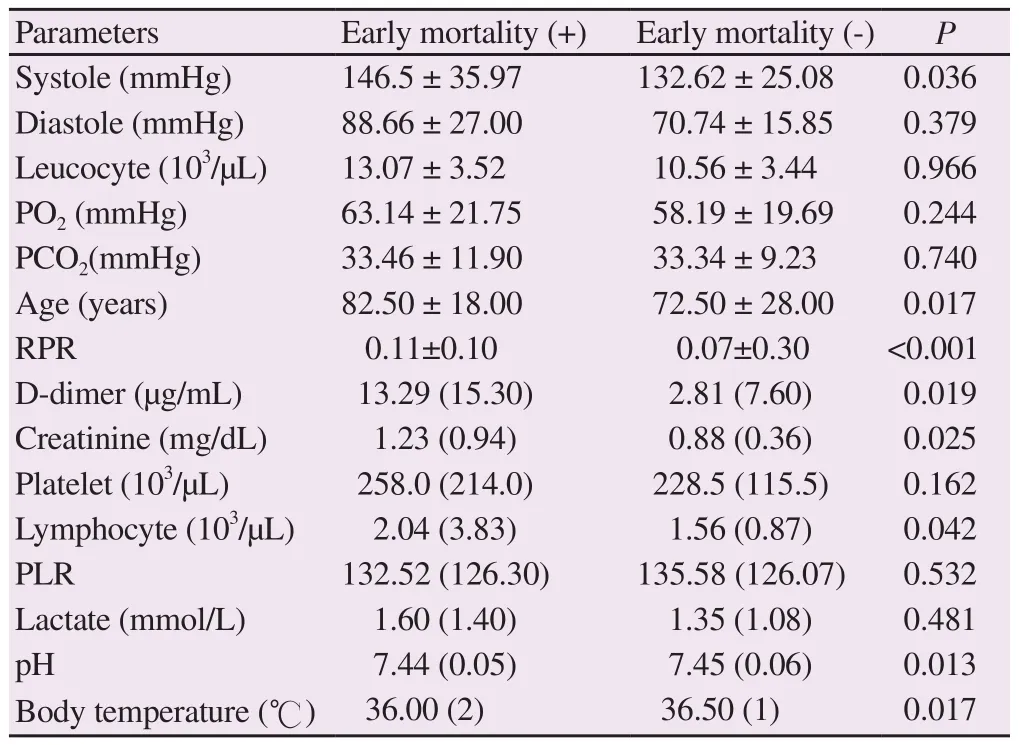
Table 4 Vital signs, laboratory, and blood gas analysis results of pulmonary embolism patients according to early mortality status.

Table 5 Logistic regression analysis of variables affecting early mortality.
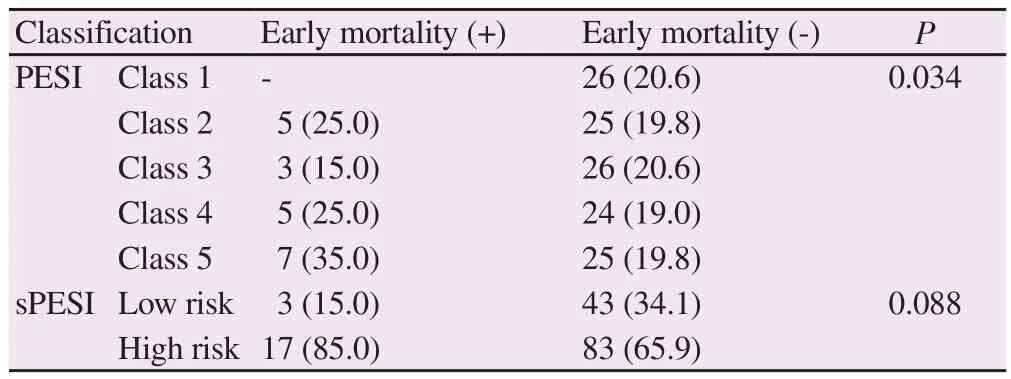
Table 6PESI and sPESI classifications of pulmonary embolism patients according to early mortality status [n(%)].
4. Discussion
The results of our study revealed that 90% of patients with early mortality were 65 years or older. Male gender was higher in patients with early mortality and women in the other group. Cugno et al.reported that the number of male patients (M/F=15/12) was higher in the mortality group. In the same study, the average age of the patients in the early mortality group [73.0 (13.5)] was higher than the other group [69.2 (15.5)][12]. The results of our study are consistent with the literature in terms of more upper mean age in the group with early mortality, and more frequently observed in the male gender.
In our study, the most common comorbidities in patients with pulmonary thromboembolism were hypertension, Alzheimer’s disease, and COPD. Ciftci et al. also showed that 38.9% of patients with pulmonary embolism had hypertension and 8.5%had COPD[13]. Likewise, the most common comorbidities in the study of Aydogdu et al. are hypertension, COPD, Alzheimer’s disease, diabetes mellitus, coronary artery disease, malignancy,cerebrovascular disease, and congestive heart failure[14]. Similar to our study, Friz et al. found a relationship between chronic cardiopulmonary disease and 30-day mortality[4]. In the light of this information, the results of our study were compatible with the literature regarding comorbidities.
Altinsoy et al. reported no significant association between 30-day mortality and syncope in patients diagnosed with pulmonary embolism[15]. In our study, 15% of the group with early mortality had syncope, and 30% of them had consciousness changes. We think that this difference may be due to the inadequacy of the clinically more serious patient to express the symptoms.
Akgullu et al. found that D-dimer and creatinine levels were significantly higher in the mortality group compared to the survival group[16]. Similarly, in our study, these two values were high in the mortality group. In the study of Labyk et al., systolic blood pressure was lower in the mortality group[17]. Conversely, in our study,systolic blood pressure was higher in the early mortality group.We think that this difference is due to the investigation of 30-day mortality rather than instant mortality in our study.
In our study, there was a statistically significant difference in risk of PESI classification between patients with and without early mortality(P=0.034). Similarly, in the study of Batt et al., The PESI risk classes(I to V) were significantly correlated with mortality rates of 3, 7, 30 and 90 d. Besides, sPESI has no less predictive features compared to PESI. Based on this, the authors concluded that the simplified version of the PESI might be of high benefit in daily clinical use[18].In this study, early mortality was not observed in the sPESI low-risk group, whereas in our study, in the group with early mortality, the sPESI classification of 3 patients was low risk. We think that this difference is due to the underlying comorbidities of the patient.
Red cell distribution width has been shown as a biomarker in Zorlu et al.’s study to show early mortality and hemodynamic deterioration in acute pulmonary thromboembolism[19]. Mirdania et al. found that the degree of chronic liver fibrosis was significantly related to the RPR found by dividing red cell distribution width into platelets[20].Bekmez et al. showed that RPR could be used in the diagnosis and follow-up of patent ductus arteriosus[21]. Besides, Hira et al. found no significant difference in RPR values in osteoarthritis patients compared to the control group[22].
Qiu et al. found that elevated levels of RPR on Day 3 and Day 7 were associated with 90-day mortality in burn patients. They also showed that RPR is an independent risk factor on mortality[23].Bilgin et al. showed that RPR could be used as a biomarker for colorectal cancers, especially right-sided[24].
Based on the results of our study, we suggest that RPR can be used safely in demonstrating early mortality in patients with pulmonary embolism without any additional cost. The emergency physicians always need rapid laboratory tests, which do not cause patient discomfort. Since RPR has these characteristics, it can provide the emergency physicians with the idea of predicting the mortality of pulmonary embolism. Considering that the most critical step in preventing the mortality and morbidity of pulmonary embolism is early diagnosis and treatment, this idea will lead to significant contributions.
In conclusion, pulmonary embolism is a preventable disease with early diagnosis and appropriate treatment. The results of our study showed that RPR is an independent risk factor for predicting mortality due to pulmonary embolism. We believe that this rate measured in the complete blood count within minutes can provide essential clues to the emergency physicians.
Conflict of interest statement
The authors report no conflict of interest.
 Journal of Acute Disease2019年2期
Journal of Acute Disease2019年2期
- Journal of Acute Disease的其它文章
- Tardive phenomenon presenting as isolated dysarthria: A rare entity mimicking stroke
- Shoshin syndrome: report of a treatable disaster
- Long-term diabetes-related severe complications among individuals with T2DM in Jazan, Saudi Arabia
- Polymorphism of hypoxia-inducible factor-1α gene in pediatric acute respiratory distress syndrome
- Characterization and frequency of antibiotic resistance related to membrane porin and efflux pump genes among Acinetobacter baumannii strains obtained from burn patients in Tehran, Iran
- Distribution of extended-spectrum β-lactamase genes in antibioticresistant strains of Pseudomonas aeruginosa obtained from burn patients in Ahvaz, Iran
