The common complications associated with osteotomy genioplasty:A literature review and meta-analysis
Si-yu-LIU,Chang-sheng-LÜ
Plastic Surgery Hospital,Peking Union Medical College,Chinese Academy of edical Science,Beijing City,100144,ina
ABSTRACT Objective The purpose of this literature review and meta-analysis is to provide an overview of common complications (neurosensory disturbances,infection,hematoma,soft tissue ptosis,secondary surgery)of osteotomy genioplasty and their risk factors to help surgeons fully inform patients of the risks before surgery and minimize the risks associated with osteotomy genioplasty through timely prevention and management during the perioperative period.Methods Multiple electronic databases were retrieved for reviews concerning common complications of osteotomy genioplasty.Randomized clinical trials,controlled clinical trials and cohort studies were considered for inclusion.The extracted data were analyzed by Rev-Man 5.3 software in order to calculate the pooled incidence of these complications and evaluate the related risk factors systematically.Results Seventeen studies were included.The mean incidence for neurosensory disturbances [0.01,95%CI (0.00-0.02)],infection [0.01,95%CI (0.00-0.01)],hematoma [0.04,95%CI (0.01-0.07)],soft tissue ptosis [0.02,95%CI (0.00-0.05)]and secondary surgery [0.02,95%CI (0.00-0.03)]were reported.Regularly reported risk factors for complications were patient's age and gender,general condition,smoking habits and surgical technique.Conclusion In this study,a literature review and meta-analysis were performed to provide an overview of common complications of osteotomy genioplasty and their risk factors.This information may help the surgeon to minimize the risk of these complications and inform the patient about the risks of complications associated with osteotomy genioplasty..
KEY WORDS Osteotomy genioplasty;Microgenia;Complication;Infection;Meta-analysis
INTRODUCTION
Osteotomy genioplasty is an orthognathic surgery for the treatment of chin deformity.It was first described by Hofer[1]in 1942.In 1983,Bell proposed a technique with extensive soft tissue preservation,which can ensure blood circulation of the osteotomy segment and reduce bone resorption.Since then,this well-designed and valuable technique has become a classical operation of maxillofacial surgery,and can be used as an auxiliary technique in combination with other orthognathic surgery[2-5].
Nevertheless,it is associated with several complications such as neurosensory disturbances,infection,hematoma,soft tissue ptosis and secondary surgery.Therefore,preoperative counselling is considered to be of great importance in surgery.The surgeon therefore should know the general incidence of common complications associated with the procedure and should be aware of the possible risk factors for these complications.This allows for patient-specific counselling prior to performing osteotomy genioplasty and enables surgeons to evaluate their work critically and maximize the chance of success.
The aim of this study is to provide an evidence-based overview of the incidence of common complications associated with osteotomy genioplasty and to discuss the risk factors related to these complications.This information could help surgeons to prevent these complications.The main complications included postoperative neurosensory disturbances,infection,hematoma,soft tissue ptosis and secondary recurrence.The impact of common risk factors,such as patient’s age,gender,smoking habits,general condition and surgical operation and duration,were discussed.
MATERIAL AND METHODOLOGY
Literature search strategy and eligibility criteria
An electronic search of Pubmed,Embase,Cochrane Library and World of Science databases was performed.Keywords included:genioplasty,microgenia,complication,horizontal sliding osteotomy,orthodontic surgery,risk factor,neurosensory disturbances,hematoma and infection.
Randomized controlled trials,prospective and retrospective cohort studies and clinical reports describing clinically observed intra-operative or postoperative complications associated with osteotomy genioplasty (neurosensory disturbances,infection,hematoma,soft tissue ptosis,secondary surgery)were included.There is no limit to race,age,gender and nationality in the diagnosis of chin deformity.In vitro studies and animal studies were excluded;studies lack of detail in the description of materials and methods were excluded;articles published before 1980,using little modern techniques,were excluded.Studies in which the number of subjects was less than 25 and the follow-up was less than 1 year were excluded.Furthermore,if the operative technique was not clear,or if different orthognathic operative techniques were analyzed together without identifying the specific outcome of osteotomy genioplasty,the paper was excluded.
Selection of studies and data extraction
The selection process was independently conducted by two researchers.Titles and abstracts were examined,and duplicate studies were eliminated.If the title or abstract mentioned one of the above postoperative complications associated with osteotomy genioplasty,the full-text article was obtained.Studies that met the inclusion criteria were analyzed.The reference lists of the included studies were searched and the references that meet the criteria are included.
The extracted data included:the demographic data of the patient group (number of patients,gender distribution,their mean age and age range);research topic,author,time of publication,study design,follow-up time and surgical methods and procedures;the incidence of postoperative complications (neurosensory disturbances,infection,hematoma,soft tissue ptosis and secondary operation).
Quality assessment of the studies
The methodological index for non-randomized studies (MINORS)tool was used to assess the quality of the selected studies.Information regarding the methodological items for non-randomized studies was recorded on predesigned forms.There are 12 evaluation indexes.Each item was scored as 0 (not reported),1(reported but inadequate)or 2 (reported and adequate).The maximum MI-NORS score was 16 points for non-comparative studies and 24 points for comparative studies.
Meta-analysis
The extracted data were analyzed by statistical software Review Manager 5.3.A subdivision was made based on the five complications (neurosensory disturbances,infection,hematoma,soft tissue ptosis and secondary operation).Data from the above study groups were pooled to compute a mean pooled incidence for each complication.Forest plots was computed for the incidence of each complication.In addition,the distribution of possible risk factors for each complication (patients’age and gender,general condition,smoking habits and surgical operation and duration)were summarized and analyzed in order to conduct a simple comparison of the distribution of possible risk factors for each complication.
RESULTS
Literature search
The initial database search identified 895 articles.From these papers,836 could be excluded based on the title or abstract.The full-texts of 59 relevant articles were obtained.The reference lists of these papers were searched,and no eligible articles were included.After strict application of the exclusion criteria,a total of 17 articles were included for analysis in our review.These papers were then subdivided based on the five complications.A flowchart summarizing the literature search and the subdivision in terms of each complication is shown in Fig.1.
Description of studies and quality assessment
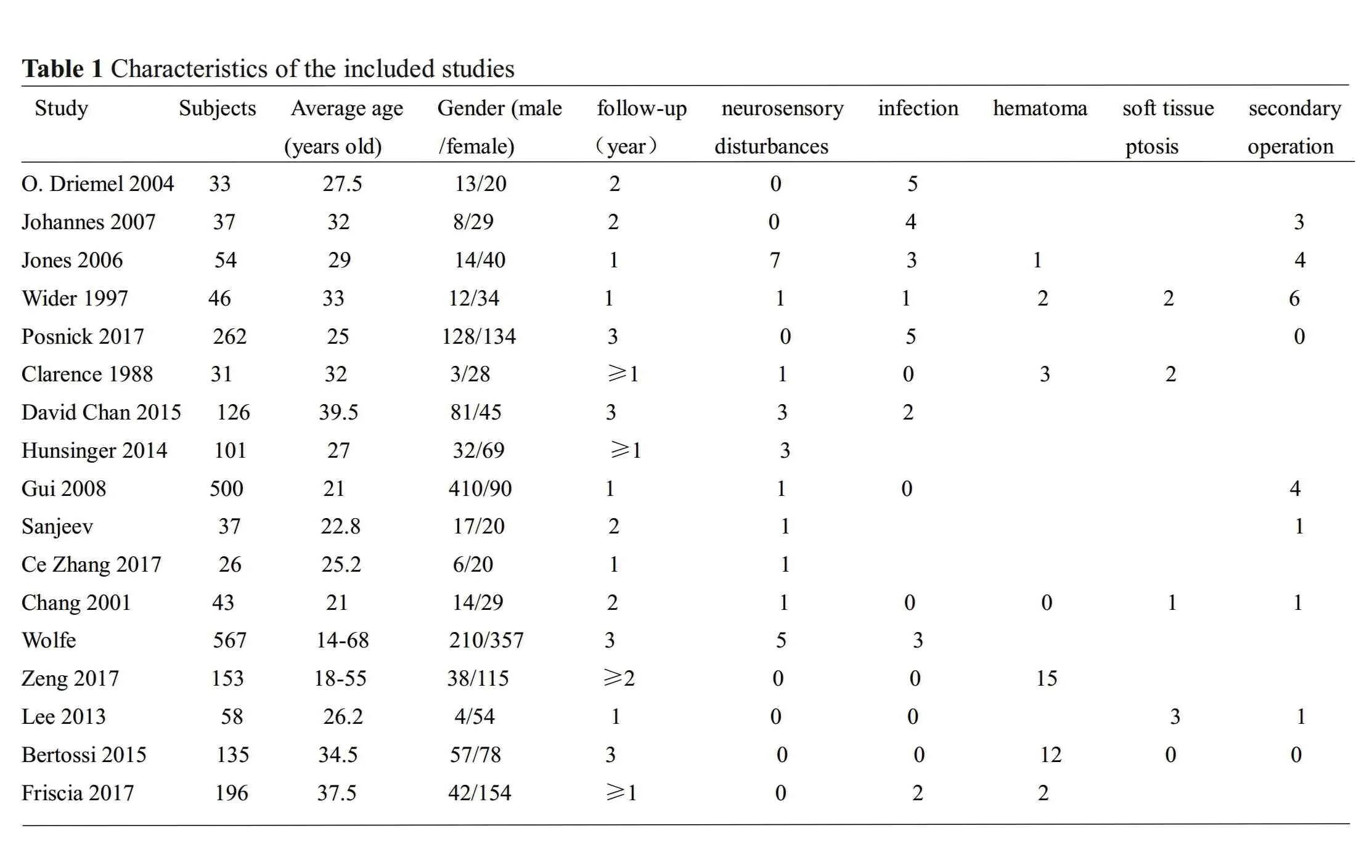
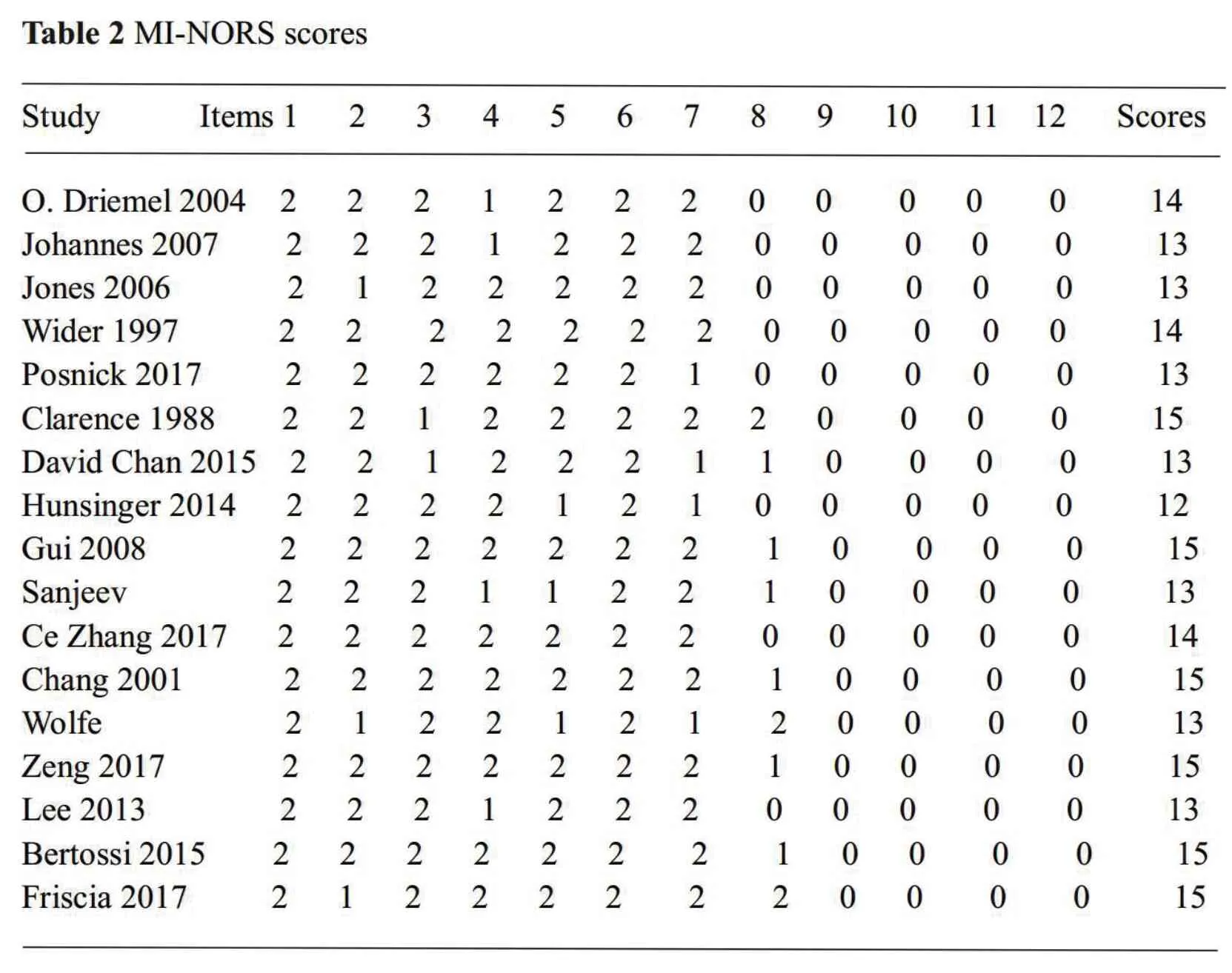
All the 17 articles were retrospective cohort studies and non-comparative studies.The MI-NORS scores of the included studies were assessed.One study scored 12 points,seven studies scored 13 points,three studies scored 14 points and six studies scored 15 points.The range of MI-NORS scores ranged from 12 to 15 points(out of 16 points).Methodological flaws mainly included an incomplete description of the methods used for data collection or evaluation of the outcome.Since there were no important methodological flaws that would relevantly influence the analysis,exclusion of specific studies or a subdivision based on risk-of-bias was found to be unnecessary.Characteristics of the included studies are summarized in Table 1.The quality assessment of the included studies used MI-NORS scores are summarized in Table 2.
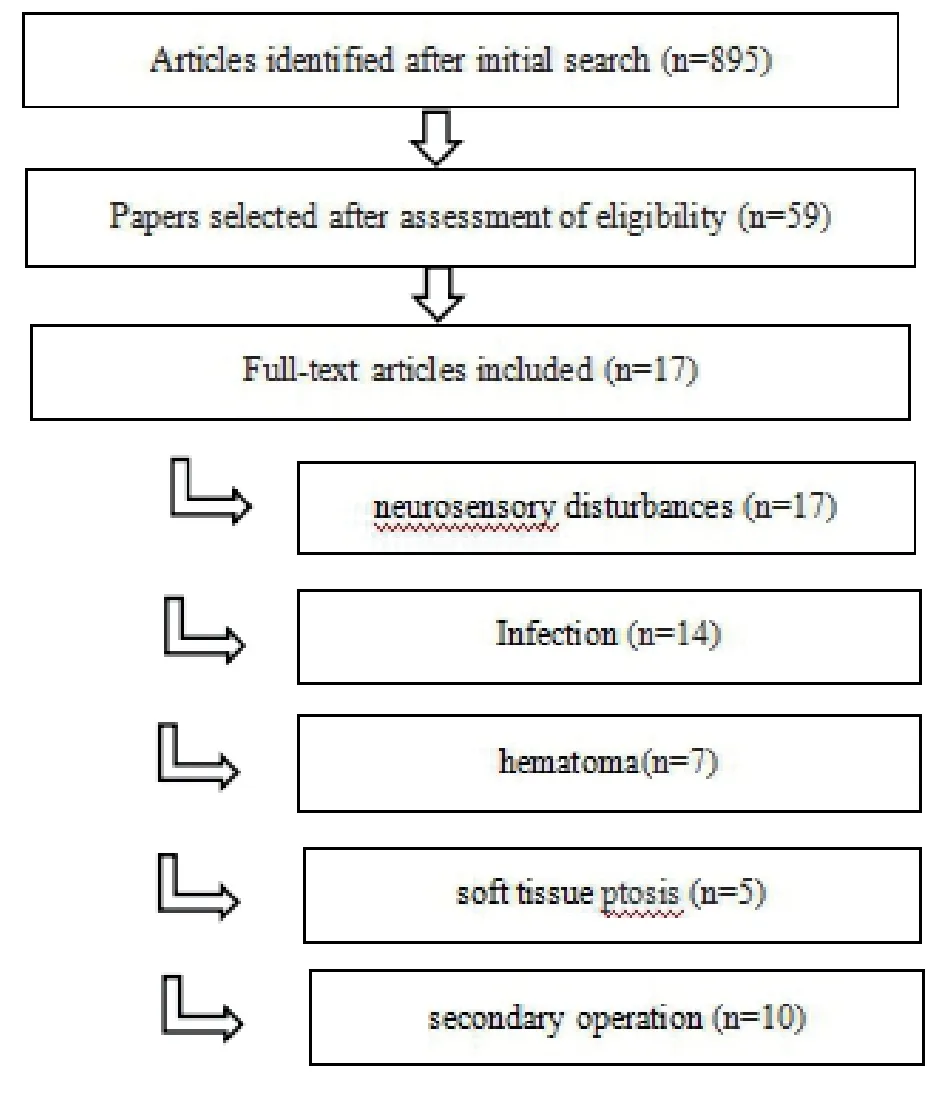
Fig.1 flowchart
META-ANALYSIS RESULTS
Postoperative neurosensory disturbances
All 17 studies describing postoperative neurosensory disturbances were included.The studies reported on 2405 patients that received osteotomy genioplasty.A total of 57 neurosensory disturbances were reported.The results of meta-analysisshowed that the heterogeneity of the study was 73%(P<0.01).The random effect model was used.The pooled incidence of neurosensory disturbances was 1% (Fig.2).
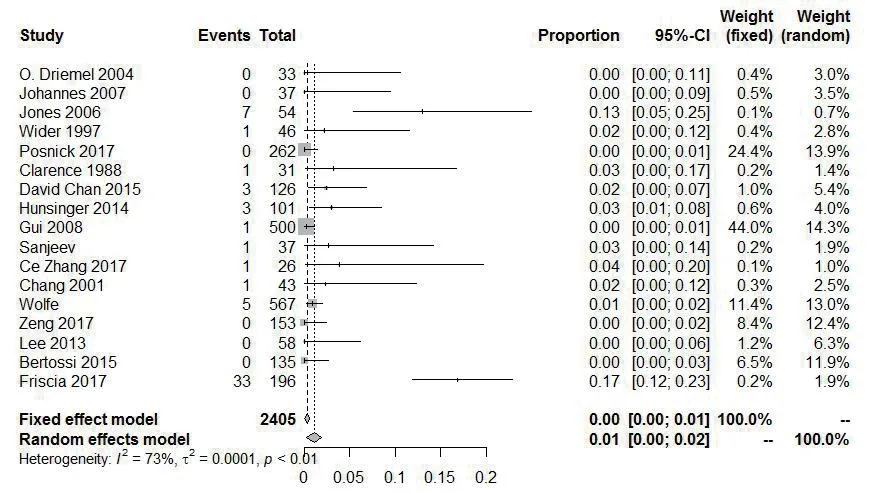
Fig.2 Forest plot for the incidence of neurosensory disturbances
The risk factors of postoperative neurosensory disturbances involved in these studies mainly include age and intraoperative operation.The relationship between age and neurosensory disturbances was reported in 3 articles[2,5-6],and the older the age,the higher the risk factor.The likelihood of permanent nerve injury has been reported to increase with approximately 5% per year.And patients over the age of 30 are thought to be more likely to suffer from temporary or permanent neurosensory disturbances after surgery.The relationship between gender and neurosensory disturbances is not clear,and some scholars[7]have pointed out that male and female patients were reported to be at similar risk of neurosensory disturbances.Surgical procedures are considered to have an important correlation with postoperative nerve injury,such as improper separation of perineural soft tissue and excessive traction of chin nerve[1-3,5,7-10].In 5 articles[3,6,8,11-12],it was suggested that the incidence of iatrogenic nerve injury should be reduced by optimizing intraoperative operation or improved technique,such as better design of osteotomy line and application of ultrasonic osteotome.
Postoperative infection
Fourteen studies[1-6,8-15]describing postoperative infection were included in our review.The studies reported on 2241 patients in total.Postoperative infection occurred in 25 patients.The results of meta-analysis showed that the heterogeneity of the study was 47% (P <0.03).The random effect model was used.The pooled incidence of postoperative infection was 1% (Fig.3).
The risk factors of postoperative infection mentioned in the above studies mainly include age,smoking habits,general condition and operation duration.In four studies[1,3,10,15],the occurrence of postoperative infection after genioplasty was reported to be more likely in smokers compared with non-smokers.The systemic condition of patients,such as poorly controlled diabetes or periodontal disease,had also been reported as a risk factor for postoperative infection [5,15].Diabetics tend to experience delayed wound healing,which in turn increased the risk of infection.Two papers[7,9]found no significant association between gender and infection,but age may be an important risk factor for postoperative infection.Older patients had a higher risk of infection.In addition,a total surgical time of more than 3h had been found to be a risk factor for infection in one study[4].
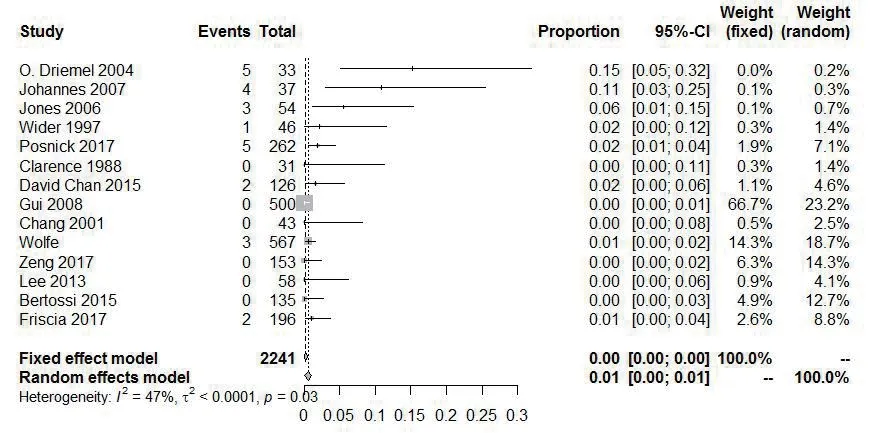
Fig.3 Forest plot for the incidence of infection
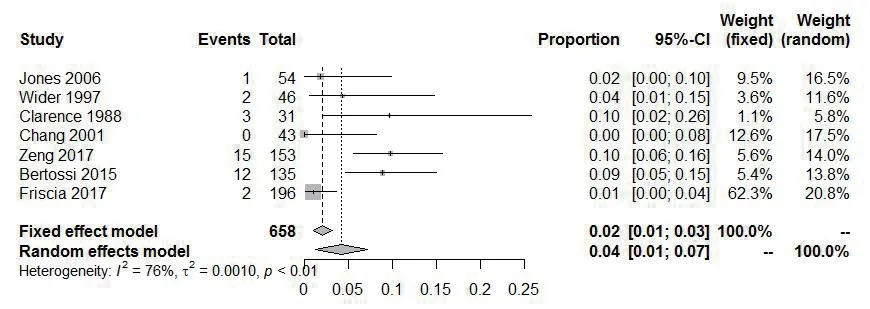
Fig.4 Forest plot for the incidence of postoperative hematomas
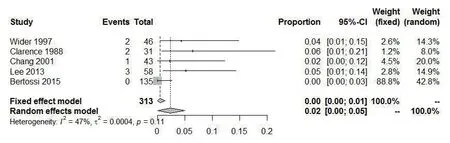
Fig.5 Forest plot for the incidence of postoperative soft tissue ptosis
Postoperative hematomas
Seven studies[1-3,6,10,14,15]described postoperative hematomas.A total of 658 patients were included,and hematomas were found in 35 cases.The results of metaanalysis showed that the heterogeneity was 76% (P <0.01).The random effect model was used.The pooled incidence of postoperative hematomas was 4% (Fig.4).
The risk factors of hematomas mentioned in the above studies include smoking habits,general condition and inappropriate surgical procedures.Similarly,smoking as an important risk factor for postoperative hematomas was mentioned in four studies[1,3,10,15].There was no increased risk of postoperative hematomas relative to gender or age,but two studies[2,10]pointed out that the incidence of postoperative hematomas was higher in women during menstruation and patients with anticoagulant drugs or supplements.In addition,the surgeon’s expertise has also been reported to be of importance.Improper procedures or excessive separation of soft tissue during surgery may cause postoperative hematomas.[1-3,10,15].
Postoperative soft tissue ptosis
Five studies[2,3,6,13,15]included the occurrence of postoperative soft tissue ptosis.The studies reported on 313 patients in total,and soft tissue ptosis occurred in 8 patients.The results of meta-analysis showed that the heterogeneity was 47% (P <0.11).The random effect model was used.The pooled incidence of postoperative soft tissue ptosis was 2% (Fig.5).
The risk factors of soft tissue ptosis mentioned in the studies mainly include inappropriate surgical procedures.Two articles[3,6]pointed that intraoperative injury to chin muscle such as genioglossus was an important factorfor soft tissue ptosis.In addition,one study[3]reported that extensive soft tissue dissection may also lead to postoperative soft tissue ptosis and glossocoma,so it is recommended that the range of intraoperative dissection meet the need for osteotomy.There were no reports about the effects of age,gender and smoking on postoperative soft tissue ptosis.
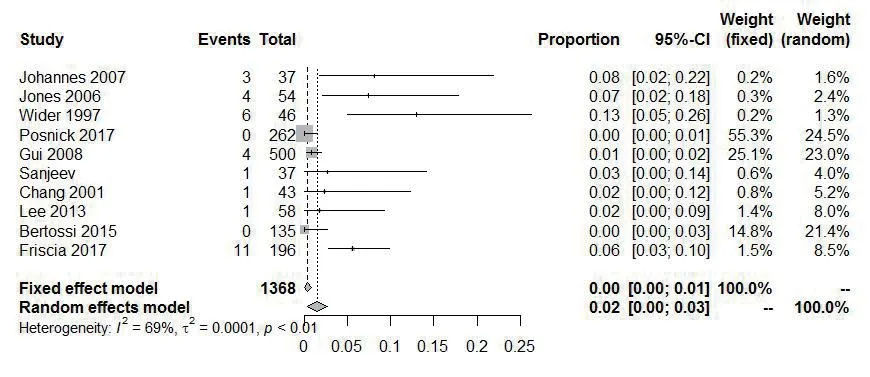
Fig.6 Forest plot for the incidence of secondary surgery
Secondary surgery
Ten studies[1-5,9-10,13,15-16]reported the situation of patients who underwent secondary surgery.A total of 1368 patients were included and 31 of them underwent secondary surgery.The results of meta-analysis showed that the heterogeneity was 69% (P <0.01).The random effect model was used.The pooled incidence of secondary operation was 2% (Fig.6).
Five studies[3,9-10,15-16]reported that most of the patients undergoing secondary surgery were due to the overprotruding chin,which made the appearance unnatural.One article [5]pointed out that after osteotomy genioplasty,the osteotomy block was easily pulled back by chin and mouth floor muscles,resulting in the retraction of osteotomy block and postoperative recurrence.The application of stable rigid internal fixation can effectively avoid this phenomenon.In addition,the scar formation of soft tissue after operation is also an important factor of recurrence.
DISCUSSIONS
This systematic literature review and meta-analysis aimed to provide a mean complication incidence that summarizes the current literature regarding common complications associated with osteotomy genioplasty,such as neurosensory disturbances,infection,hematoma,soft tissue ptosis and secondary surgery.
Postoperative neurosensory disturbances
Neurosensory disturbances are very common after osteotomy genioplasty,mainly manifested by numbness of lower lip or chin area and hypoesthesia or disappearance of sensation.However,the vast majority of patients with neurosensory disorders are temporary,mostly returned to normal within 12 months.If any type of altered sensation is present one year after osteotomy genioplasty,it is considered to be permanent.
In previous literature review,lacking of standardized assessment procedures complicated the comparison between studies,resulted in a wide variation in the reported incidence of chin nerve injury.This review provides a patient-focused approach to complications associated with osteotomy genioplasty by reporting subjective neurosensory disturbances.Based on the literature,improper operation is an important factor of nerve injury.Some important factors could help the surgeon in an attempt to prevent neurosensory disturbances after osteotomy genioplasty.Manipulation of the nerve during the surgical procedure generally increases the risk of nerve injury and should therefore be prevented.In order to avoid intraoperative injury,it is necessary to accurately identify the chin nerve and avoid excessive traction of the nerve.Previous studies[17]suggested that in order to avoid intraoperative injury of chin nerve,the osteotomy line should be 4-5mm from the inferior edge of the chin foramen.Some scholars[14]reported that changing the osteotomy design such as oblique or sagittal osteotomy can effectively reduce the incidence of neurosensory disturbances.In addition,age is probably the most important patient-related risk factor for neurosensory disturbances.Older patients have higher risk of postoperative temporary or permanent nerve injury.Other characteristics of patients were rarely mentioned in the previous papers.
Postoperative infection
Postoperative infection is a common complication after any form of surgery.The incidence of incision infection is high after orthognathic surgery.Intra-oral wound is considered to be“clean-contaminated”wound,and the potential infection rate is as high as 15%[17].The risk factors of infection after osteotomy genioplasty mainly include age,smoking habits,poorly controlled periodontal disease or diabetes,operation time,oral hygiene after surgery,postoperative physical activity and diet[17-18].Long-term antibiotic prophylaxis (before/during surgery and more than 1 day after surgery)probably decreases the risk of infection at the surgical site,particularly in patients undergoing a surgical procedure that exceeds 3h and in patients who smoke.There is no definite conclusion on the exact preferred amount and type of prophylactic antibiotic[10].When postoperative infection dose occur,it is practically always effectively treated using a regiment of amoxicillin-clavulanate or clindamycin.Furthermore,possible precautions can be taken to prevent infection.Smoking is considered as a statistically significant risk factor,with an infection rate of 9%[4].Patients should be encouraged to stop smoking.In addition,preoperative detailed medical history inquiry and physical examination is particularly important,especially for the patient’s general condition and dental occlusion.The occurrence of infection could also be further reduced by specific surgical precautions,such as using fibrin glue in the wound.
Postoperative hematoma
We found that smoking habits is regularly reported as a risk factor for postoperative hematoma,possibly in combination with the general condition of patients.The improper operation also plays an important role in this association.Lee[13]reported that severe wound swelling and ecchymosis were associated with irregular menstrual cycles in female undergoing orthognathic surgery.Multiple surgical procedures or low body mass index (BMI)may also increase the risk of hematoma[19].In order to avoid hematomas as much as possible,it is necessary to fully understand the drug application history and the function of coagulation and anticoagulation before surgery,especially the use of anticoagulants and the history of excessive bleeding after minor trauma.Anticoagulants such as aspirin,warfarin and vitamin E should be banned 10 days before operation.Appropriate surgical procedures are also of great significance to reduce intraoperative bleeding and postoperative hematoma.The occurrence of hematoma could also be further reduced by using bone wax or absorbable hemostatic material.If necessary,the indwelling drainage tube for 24-48 hours after operation is also a choice worthy of consideration.
Postoperative soft tissue ptosis
The shape of chin is composed of bone tissue and soft tissue.In order to achieve the ideal aesthetic state after osteotomy genioplasty,the morphology of soft tissue should not be neglected.The causes of soft tissue ptosis and lower lip insufficiency are not completely clear,but most scholars believe that the chin muscle plays an important role.Failure to properly handle this muscle during surgery will lead to the ptosis of soft tissue and lower lip,salivation and exposure of the lower teeth [20].Accurate suture of chin muscle with absorbable thread after genioplasty can prevent its occurrence.Extensive muscle and soft tissue dissection may also result in soft tissue ptosis and glossocoma,as well as the risk of bone resorption and osteonecrosis.Therefore,when dealing with the osteotomy segment during surgery,it is suggested to preserve the attachment of soft tissue and periosteum as much as possible,especially the genioglossus[15].
Secondary surgery
The causes of re-operation after osteotomy genioplasty mainly include unsatisfactory morphology of chin (such as over-protruding chin or unnatural mentolabial sulcus),postoperative recurrence and abnormal chin morphology and function caused by complications.Using stable rigid internal fixation can reduce the retraction caused by chin and mouth floor muscles,reducing the possibility of postoperative recurrence.In addition,postoperative soft tissue scar is also an important cause for recurrence.
The satisfaction of chin morphology is often greatly affected by the subjective factors of patients and surgeons,so effective communication and adequate psychological counseling may reduce the willingness of patients to receive secondary surgery.Some studies have pointed out that the living quality of patients receiving orthognathic surgery have been improved to some certain extent psychologically and socially[18].In addition,patients suffering from mental illness,such as depression,should undergo systematic examination before operation and receive treatment for depression if necessary[14].
CONCLUSION
In conclusion,this systematic literature review and metaanalysis provides an overview of important common complications associated with osteotomy genioplasty.Pooled mean incidences of each complication were computed and the risk factors of complications were summarized and analyzed.The results of this study can help surgeons to better understand the occurrence of complications after osteotomy genioplasty,so as to achieve better surgical results and improve doctor-patient satisfaction.
 Chinese Journal of Plastic and Reconstructive Surgery2019年2期
Chinese Journal of Plastic and Reconstructive Surgery2019年2期
- Chinese Journal of Plastic and Reconstructive Surgery的其它文章
- Experience of VSD in the treatment of foot tophi rupture with severe infection wounds
- Clinical Observation of Anesthesia Effect of 2% Lidocaine by Air Pressure Injection in Facial Skin Aesthetic Treatment
- Implantation Instrument on the Expression of Collagen-I and Cell Proliferation Markers in Pathological Scar
- Inhibitory Effect of Photodynamic Therapy on Keloids
- Experimental Effect of Umbilical Cord Mesenchymal Stem Cells on Stress Urinary Incontinence Rats Model and Efficient Tracking in vivo with MRI
- Advances in Evaluation of Facial Asymmetry
