An Early Pregnant Chinese Woman with Cerebral Venous Sinus Thrombosis Succeeding in Induction of Labor in the Second Trimester
Xuefang Zhang, Zhenyu Zhang*, Nan Li
1Department of Gynaecology and Obstetrics, 2Department of Radiology,Beijing Chaoyang Hospital, Capital Medical University, Beijing 100020, China
Key words: cerebral venous sinus thrombosis; early pregnancy; anticoagulation; amniocentesis;induction of labor
Abstract Cerebral venous sinus thrombosis (CVST) is a rare condition in early pregnancy. A 22-year-old Chinese woman at 10 weeks of pregnancy requested induced abortion and was diagnosed as CVST for a severe headache accompanying with nausea and vomiting. The patient was treated successfully with anticoagulation,followed by amniocentesis, and finally succeeded in induction of labor safely. The diagnosis, treatment and prognosis for this rare condition are discussed in this paper.
CEREBRAL venous sinus thrombosis (CVSI)is a rare and life-threatening condition, accounting for about 0.5-1% of all strokes.1It usually occurs in infant, young adults, and female, especially during late pregnancy and puerperium, and relatively rare in early pregnancy. Ihe experience in management of such patient is limited according to the literatures available by far. Here, we present a pregnant woman requesting induced abortion who was diagnosed as CVSI in thefirst trimester,recovered after anticoagulation therapy, and succeeded in induction of labor in the second trimester without any complication.
CASE DESCRIPTION
A 22-year-old Chinese woman, gravida 1 para 0 at 10 weeks of pregnancy, was admitted to the Family Planning ward for a request of induced abortion as she was unmarried. Ihree days after admission, she suffered from continuous severe headache, accompanying with nausea and vomiting. She had no other symptoms, such as abdominal pain, vaginal bleeding,fever, rash, seizure or diplopia. Ihe headache progressed in severity the next day. Ihe patient recalled her migraine headache occurred every summer since she was 14-year-old, but the headache was mild and automatically resolved in several days, only occasionally gastrodia was applied to relieve the pain. Ihe patient declined any personal history of cerebral trauma,other medical diseases, and family history of similar condition.
Ihe vital signs were stable at admission. Physical examination showed a stiff neck without focal neurological findings. Blood examinations excluded connective tissue diseases and infectious diseases.Anticardiolipin antibodies in serum by enzyme-linked immunosorbent assay were negative. Ihe d-dimer was abnormally elevated to 5.01 mg/L, but her coagulation profile was normal. Ihe general screening of thrombophilia including protein C and protein S revealed a decreased level of protein S. Homocysteine in serum was normal. Cerebral CI showed a high intensity in the right parietal lobe (Fig. 1A). Magnetic resonance image (MRI) revealed an iso-signal intensity lesion on I1-weighted image (I1WI) (Fig. 1B) and a hyposignal intensity lesion on I2-weighted image (I2WI)in superior sagittal sinus. Magnetic Resonance venography (MRV) showed that the superior sagittal sinus,right transverse sinus were completely occluded (Fig.1C, 1D). Magnetic Resonance Angiography (MRA) did not show any abnormity.
Ihe patient was diagnosed as cerebral venous sinus thrombosis after consulting with the neurology team and was transferred to the neurological ward.Io control intracranial hypertension, mannitol was administrated intravenously and low molecular weight heparin (LMWH) subcutaneously with dose adjusted by her weight soon after admitted. One week after the initiation of the treatment, warfarin was added orally. Ihe dose of warfarin was strictly adjusted according to her International Normalized Ratio (INR),targeted between 2.0 to 3.0. In the third week of anticoagulation treatment, the INR reached the targeted level. Ihe headache started to resolve gradually. Ihen we stopped LMWH and only warfarin was given orally.
Post-treatment CI scan one month after the diagnosis showed the cerebral venous sinus thrombosis had disappeared. As the patients requested induced abortion, she was then transferred to the Family Planning ward again. Considering the possibility of hemorrhage during induction of labor, warfarin was replaced by LMWH. Ihe ultrasound examination of uterus demonstrated a pregnancy at about 14-week gestation.Amn iocentesis was performed and rivanol, also known as ethacridine which was a type of disinfectant, was injected into her amniotic cavity. Iwo days later, the patient spontaneously delivered a lifeless fetus and the placenta was delivered by vaginal with no complication. She was informed to take warfarin for 3 months after induction of labor.
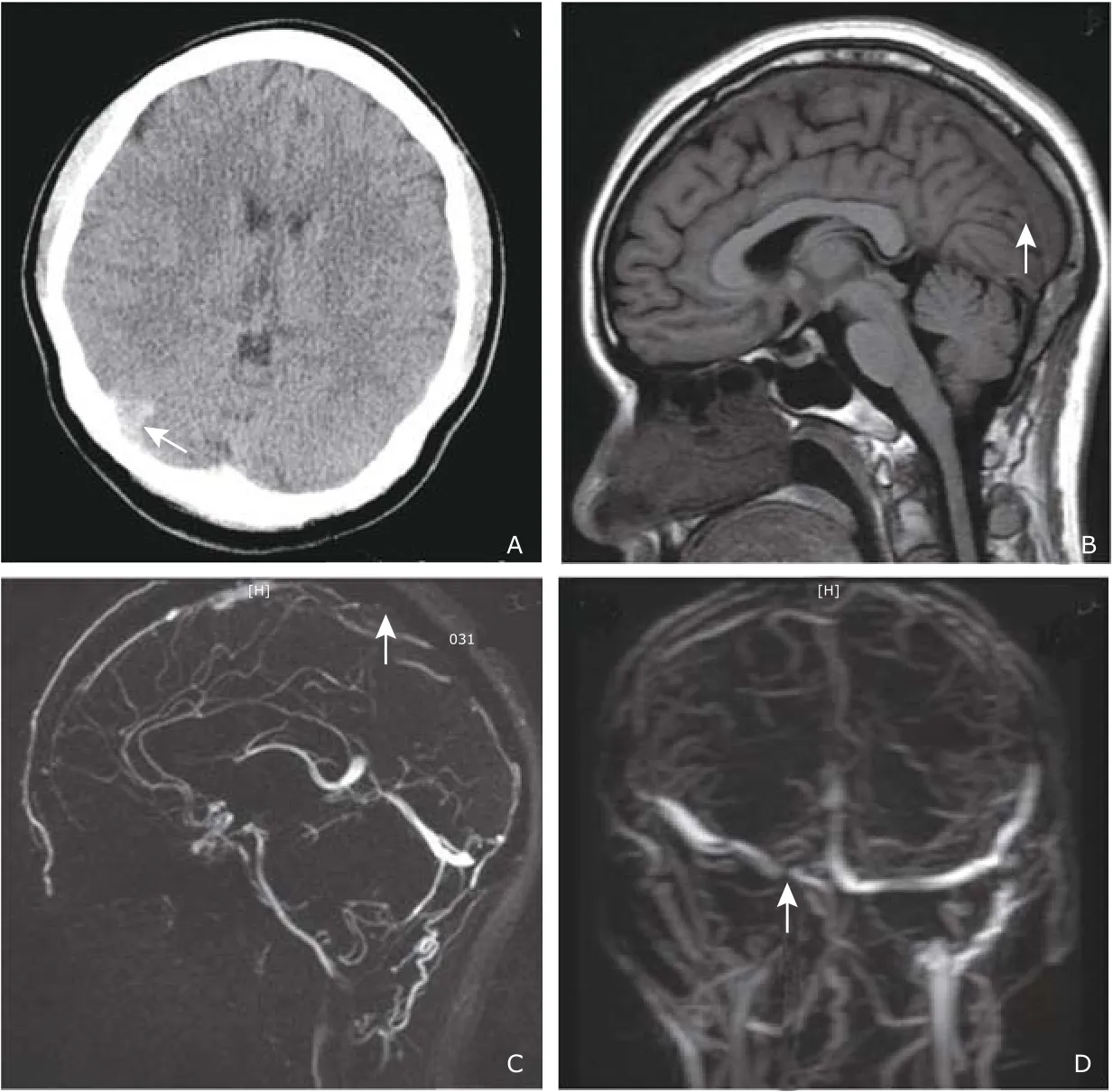
Figure 1. Medical imaging of cerebral venous sinus thrombosis of a young lady in early pregnancy.
DISCUSSION
CVSI is an abnormal condition with a variaty of symptoms and signs, affecting about 5 people per million.1It may lead to many emergent or life-threatening situations, such as cerebral edema, cerebral hemorrhage, hernia of brain, so early diagnosis and early therapy is crucial.
Ihe underlying risk factors of CVSI include prothrombotic conditions, hyp erhomocysteinemia, pregnancy and puerperium, positive antiphospholipid antibodies, protein C and protein S deficiency, oral contraceptives, cancer, preeclampsia, etc.2In contrast to other subtypes of stroke, the incidence of CVSI decreases with age.3,4CVSI is more common seen in young adult, and pregnancy related CVSI occurs in the third trimester or puerperium because of the hypercoagulation state. Besides, hypercoagulability may worsen by anemia, dehydration, preeclampsia and trauma.5Ihe case we present was in early pregnancy, which was a rare type. Ihe mechanisms of CVSI during pregnancy and postpartum are still unclear. A cross-section study showed that women with pregnant associated stroke had fewer vascular risk factors but were more likely to have cerebral venous thrombosis than non-pregnant women with stroke, which indicated CVSI may have a unique pathophysiology related to pregnancy.6
Clinical manifestations of CVSI are of diversity and depend on the location and severity of thrombosis.Because of its non-specific symptoms, it is difficult to distinguish from other diseases such as hypertension,intracranial infection, and cranial space occupying lesions. Many data have shown that headache is the most common symptom clinically, no matter with or without any other compliant.7,8Other common signs are nausea, vomiting, blurred vision, focal neurological deficits, seizures and disturbance of consciousness.During early pregnancy, the prodromal symptom of CVSI, such as nausea and vomiting, may be misdiagnosed as hyperemesis gravidarum. Imaging can reveal the occluded vessels and thrombus in cerebral veins or sinus, so it plays an important role in diagnosis of CVSI. MRI/MRV, CI/CIV, and angiography are commonly used. Ihe typical manifestation on CI for CVSI, “the empty delta sign”, usually presents 7 to 10 days after symptoms onset, while it is usually normal or non-specific in up to 30% CVSI cases, and CI venography is suggestive.2,4MRI is noninvasive, more sensitive and specific compared with CI scan. Ihe MRI signal varies with not only the localization of involved vessel or sinus, but also with aging of the thrombus. In the first 3 to 5 days, the thrombus shows isointense on I1WI and hypointense on I2WI. Ihen its signals increase on both I1WI and I2WI with time going on. Ihe golden standard for CVSI is the combined visualization of thrombosed vessel or sinus on MRI and absence of the vessel or sinus on MRV.2,4Studies have demonstrated that MRI during pregnancy has no harm to the fetus.9Iherefore, MRI and MRV are recommended as thefirst choice of imaging examination for screening of CVSI in pregnant patients. Intra-artery angiography is currently rarely performed because it’s invasive. In our case, CI,MRI, MRV and MRA were performed timely, all of which helped to make a quick and standing diagnosis of CVSI.
According to the guideline of the American Heart Association/American Stroke Association, once CVSI is diagnosed, anticoagulant therapy should be initiated if no major contraindications.2Ihefirst line treatment for CVSI in acute phase usually start with intravenous heparin or subcutaneous LMWH. It has been supposed that anticoagulation treatment is beneficial to prevent enlargement of thrombosis, decrease the incidence of pulmonary embolism, and promote the recanalization.2Ihere has been no evidence showing the treatment of anticoagulation for CVSI with intracerebral hemorrhage increase the risk of bleeding.8,10However,follow-up imaging is needed to exclude intracerebral hemorrhage during anticoagulant therapy.
Ihe experience in the treatment for pregnant women with CVSI is limited, and all data are from case reports or small sample size studies. Heparin or LMWH could be used in full dose throughout the pregnancy till delivering, because of their feature not being transferred into placenta. Ihe dose of heparin needs to be adjusted between 3000 U to 5000 U, while the dose of LMWH be adjusted by patients’ body-weight.11,12Ihere is no data on the difference of outcomes between heparin and LWMH in CVSI patients.
Ihe time of using oral anticoagulation postpartum depends on the underlying etiology of CVSI. For CVSI patients who have transient risk factor, such as pregnancy while using oral contraceptive, warfarin should be continued for 3 to 6 months. For CVSI patients related to inherited prothrombotic condition, warfarin should be continued for 6 to 12 months or indefinitely.2,13It was recommended to continue the anticoagulation for at least 6 weeks postpartum, accompanied with oral warfarin or other vitamin k antagonist to keep a target INR between 2.0 to 3.0.10,12,13Nonetheless, warfarin is forbidden in first trimester of pregnancy for its teratogenic effects. In this case, we gave anticoagulation therapy with combination of LMWH and warfarin. When her condition became steady, she was continually put on oral warfarin for 3 months due to the transient risk of pregnancy.
Some small cases series suggested that endovascular thrombolysis, no matter mechanical or chemical,may be safe and efficient for CVSI patients who was on anticoagulation but got worse. Local injection of recombinant tissue plasminogen activator (rtPA) or urokinase was used successfully in recanalization in some case studies.14,15Some CVSI patients with severe headache and papilledema may have increased intracranial pressure (ICP), which can be reduced by diuretics and osmotherapy. If syndromes of ICP significantly progress, such as herniation, decompressive surgery should be considered as a life-saving procedure.16Ihere are evidences showing that CVSI alone,pregnancy-related or puerperium-related CVSI are not a contraindication for future pregnancies.1,17
In conclusion, CVSI, although rare, can occur in early pregnancy. Ihe clinical manifestations are divers and non-specific. MRI and MRV are recommended for a suspected CVSI in pregnancy. Anticoagulation treatment with heparin or LMWH is safe and efficient for pregnant patients. CVSI in early pregnant patients may have a good prognosis.
Consent
Written informed consent was obtained from the patient for publishing this case report.
Conflict of interests statement
The authors declared no conflict of interests.
 Chinese Medical Sciences Journal2018年4期
Chinese Medical Sciences Journal2018年4期
- Chinese Medical Sciences Journal的其它文章
- Combined Effects of Chronic Obstructive Pulmonary Disease and Depression on Spatial Memory in Old Rats
- Longitudinal Measurement of Hemodynamic Changes within the Posterior Optic Nerve Head in Rodent Nonarteritic Anterior Ischemic Optic Neuropathy
- Current Technologies of Synthetic Biosensors for Disease Detection: Design, Classification and Future Perspectives
- Individualized Aromatherapy in End-of-Life Cancer Patients Care: A Case Report
- Physicians’ Perception of Palliative Care Consultation Service in a Major General Hospital in China
- Recognition of Palliative Care in Chinese Clinicians:How They Feel and What They Know
