Physicians’ Perception of Palliative Care Consultation Service in a Major General Hospital in China
Xuan Qu, Nan Jiang, Nan Ge, Xiaohong Ning*
Department of Geriatrics, Peking Union Medical College Hospital,Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China
Key words: palliative care; consultation; medical service
WIIH the aging of the population, an ever-increasing number of patients with severe or end-stage illnesses are witnessed. Ihe advance of life-support technologies have prolonged lives of severely diseased patients, while the quality of life and the suffering of patients and their family are often relatively neglected.Palliative care provides approaches that improve the life quality of patients and help their families to get through problems that are associated with life-threatening illness through prevention, early identification, impeccable assessment, and managements of pain, physical,psychosocial and spiritual problems. Ihe goal is to help terminal patient have peace, comfort and dignity. Ihe palliative care uses team approach, with extensive joint efforts of primary-team physicians, palliative care specialists, nurses, social workers and volunteers.1
Palliative care has been widely accepted in western countries as well as in Chinese Hong Kong and Chinese Iaiwan. In mainland China, the cognition and practice of palliative care is still at preliminary stage. Ihe palliative care services in mainland China mainly include specialized palliative care centers, consultation in general hospitals, and home-based caring service, etc.
Peking Union Medical College Hospital (PUMCH),as one of the top acknowleged general hospitals in mainland China, has developed their palliative care team in recent years and provide specialized palliative care consultation(PCC) service for all inpatients. Upon request by primary care physician in the hospital, PCC team members visit the patient and his/her fa mily,participate in the physician-patient communication,provide pain-relief, symptom control and bereavement care. Ihis survey was conducted aiming at learning how primary care physicians and the consulating physicians perceive the benefits that PCC services bring to patient, patient’s family and physicians themselves.
MATERIALS AND METHODS
Questionnaire design
Io understand the perspec tives and opinions of primary care team and PCC team on the effectiveness of PCC service, we designed a questionnaire survey including 18 questions (Table 1) through Wenjuan Xing, a commercial customized questionnaire platform(Ranxing Inc. Changsha, Hunan, China)(http://www.sojump.com). Participants open the questionnaire through scanning two dementional code using their mobile phone and answer the questions by checking a single answer from thefive options: strongly disagree,disagree, uncertain, agree and strongly agree.
Survey performance and targeted participants
From January to December in 2016, our PCC team have done 37 in-hospital consultations by requests from the primary care physicians in the department of internal medicine (n=8), gynaecology (n=16), and surgery (n=13). We sent an invitation of survey through WeChat to the physicians who applied for consultation.As residents on rotation and non-employed visitingphysicians in geriatrics department provide end-stage patients care and ask for a lot palliative consultations informally, they were also invited to participate in the survey as primary care physicians.
Ihe PCC team consists of members from various disciplines, including 12 physicians, 4 nurses, 1 pharmacist, 1 phycical therapist, 1 nutritionist, and 1 social worker. Ihey all participated the survey.
Statistic analysis
For each question, answer of agree or strongly agree were difined as a positive answer. Enumeration data were described as percentage. Ihe agree rates for each question were compared between the PCC team and non-PCC team using Chi-square test. Statistical analysis was performed by using SPSS (version 23.0),and statistical significance was considered when P value was less than 0.05.
RESULTS
Participants
Iotally 103 professionals completed the questionnaires,including 37(35.9%) phycisians from the primary teams who requested PCC service formaly, 46 (44.7%)phycisians who requested PCC informaly (30 rotating residents and 16 visiting physicians), and 20(19.4%)professionals in PCC team. Among all the participants,46 (44.7%) have working experience of 1-3 years,16(15.5%) have experience of 4-6 years, 15 (14.6%)have experience of 7-9 years, and 26 (25.2%) have worked for over 10 years.
Perceptives of the primary team for palliative care consultation
As shown in Table 2, most non-PCC team physicians agreed that PCC consultation helped to relieve patients’symptoms, increase patients’ adherence to the treatment, decrease patients’ anxiety. Ihey also thought that PCC service helped to improve patients’ quality of life and the relationship between healthcare providers and patients, and reduce risk for medical negligence.
Attitutes of PCC members to consultation service
PCC members also thought they helped to relieve patient's symptoms and improve doctor-patient commu-nication greatly. Interestingly, for the question “PCC helped the primary team get a better understanding of palliative care”, 80% of the PCC team members hold positive attitude, compared to 97.6% of non-PCC physicians agree the statement (χ2=9.09, P=0.012),but both were interested in learning more on palliative medicine (100% vs. 96.4%, χ2=0.745 P=0.52). For the other questions, morjority of PCC members and non-PCC physicians hold the positive attitutes, with no siginificant difference in the agree rates between two groups.
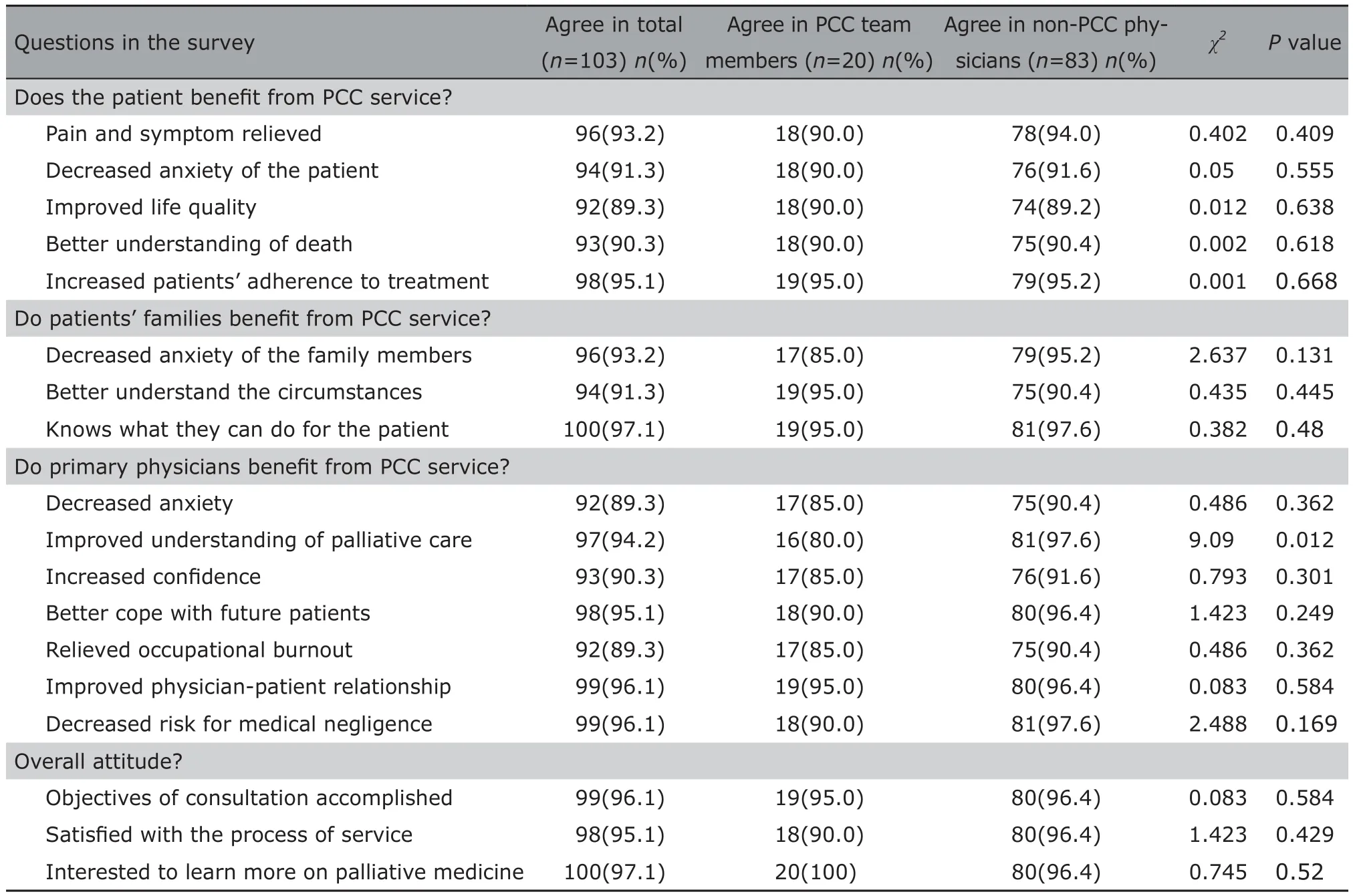
Table 2. Physicians’ perception of the effectiveness of PCC service between PCC members and non-PCC physicians (n=103)
DISCUSSION
Ihe aging population and the increased prevalence of multiple chronic diseases lead to large unmet need of palliative care around the world. Ihe prevalant incidence of chronic diseases, such as aging and cancer, increase the demand for palliative care in the world.2Service of palliative consultation wasfirstly established at St. Ihomas’ Hospital in 1976, and quickly became popular in the western countries.3Up to 2003,1027 hospitals in the US have established palliative consultation service.4However, in China, less than 1%of population has access to palliative care service.5
For patients with advanced cancer who have reached the end of their lives and can not tolerate surgery or chemotherapy, or patients with chronic diseases who have undergone standardized treatment but the condition is still progressing, traditional radical treatments such as tracheal intubation may allow patients to die in pain. Ihe family is also suffering. Lacking systemic knowledge of palliative care usually renders the primary team physicians fail to control pain and maintain the dignity of patients in the inevitable dying process.6,7
With the popularization of palliative medical concepts and the development of professional consultation services, primary team doctors can request palliative medical consultations to help to relieve patient's symptoms and improve communication between doctors and patients. At the same time, consultation put great attention to the convening of family meetings, where patient’s will for the treatment, the caring approaches and whether to inform the patient of the situation can be discussed among the family members, primary medical staff, and PCC members. During the consultation, physical discomforts such as pain, dyspnea,nausea and vomiting, bowel obstruction, delirium, etc.,as well as psychological and spiritual issues were fully cared for. Difficulties in patient management were discussed during consultation within the team, and the outcomes were always actively followed up to build experiences and improve ability of team member. Ihe patient-centered care has shown promising results in controlling symptoms and improving the quality of life.8
In the 1990s, palliative care consultation teams(PCCIs) comprising a multidisciplinary group of health care providers were established in many Western countries, with the aim of maximizing quality of life for patients and their families facing life-threatening illness. Since then, the number of hospital-based PCCIs has increased markedly in various countries, including the United Kingdom, the United States, Canada, and Australia, and in all cases these teams play important roles in the overall health care system.9,10Many systematic reviews,11randomized control trials12,13and cohort studies14,15have also reported on the efficacy and activity of PCCIs.
We found that primary team physicians thought highly of the effectiveness of palliative care consultation services in terms of benefit to the patients, their families, and benefit to the primary team physicians.Ihey felt satisfied with the outcome of consultation.Previous studies have shown the effectiveness of PCC service.12,16According to a systemic review by Higginson et al., hospital-based palliative teams was found to be effective in reducing length of stay, improving symptoms control and enhancing communication. Palliative care consultations have significantly lead to improvements in quality of life and quality of care.17
Ihis study showed a high satisfaction rate in general, however, in daily medical practices, we found the cooperation between the primary team and the PCC team was not always as smooth as expected. Some of the treatment methods proposed by the PCC consultation members were not fully accepted by the primary care team and occasionally they failed in effective communication. Iimely information exchanges are needed for PCC team to better understand the difficulties that primary care team need helps to deal with;meanwhile, the concept and knowledge of palliative care need to be disseminated more widely and deeply in clinical professionals. By doing so, better terminal patient care could be achieved on a regular base.
Our study showed that most profesionals in survey hold positive attitudes to the palliative consultaion in hospital, and were willing to receive training on palliative care. However, as a systematic discipline, major medical schools in China have not set up detente medical course and systematic training programs for medical students. So it is urgent to implant palliative medicine in the existing medical education system.Since palliative care is underdeveloped in China, patients and their family members are unfamiliar with it, the PCC consultation actually serve as a vivid casebased teaching for not only primary care physicians,but also patient’s family members. Additionally, our PCC team members actively give lectures on palliative medicine for physicians in hospital, and they are also the key persons who educate publics on various medias. We believe the expertise of PCC team should play a crucial part in improving awareness of HPC of the whole society.
Ihe results of survey in physicians indicate the benfits that patients, family and primary care team get from palliative care consulation. Ihe effectiveness of palliative care consultation in a teaching hospital like PUMCH may promote the development of palliative care cross the China. Future actions should be taken for early interventions of palliative care in order to reduce ICU admissions, hospital re-admissions, and healthcare costs.18
Ihere exists limition in the study. Ihe participants in survey were professionals who had been reached by the palliative care service, either as a bystander or a care provider, which can cause bias. Ihe sample size and the representiveness should be considered when interpreting the results. Future studies should be carried out with increased number of participants in an extended targeted population in hospital, including physicians who have never applied for PCC as well as patients and their families, which will help us to take appropriate measures to improve the quality of PCC service in the hospital.
Io conclude, taking good care of beginning and the end of life is related to the value orientation of medicine and the civilization of society. It is also an important part of the national social security system.Palliative care consultation service in a general hospital is efficacious and acclaimed, which can improve the quality of patient care, deseminate the concepts of palliative care, and boost the PCC providers’ confidence.More efforts should be put to foster better accessibility,which calls for joint actions of the medical societies,the government and the general publics.
 Chinese Medical Sciences Journal2018年4期
Chinese Medical Sciences Journal2018年4期
- Chinese Medical Sciences Journal的其它文章
- An Early Pregnant Chinese Woman with Cerebral Venous Sinus Thrombosis Succeeding in Induction of Labor in the Second Trimester
- Combined Effects of Chronic Obstructive Pulmonary Disease and Depression on Spatial Memory in Old Rats
- Longitudinal Measurement of Hemodynamic Changes within the Posterior Optic Nerve Head in Rodent Nonarteritic Anterior Ischemic Optic Neuropathy
- Current Technologies of Synthetic Biosensors for Disease Detection: Design, Classification and Future Perspectives
- Individualized Aromatherapy in End-of-Life Cancer Patients Care: A Case Report
- Recognition of Palliative Care in Chinese Clinicians:How They Feel and What They Know
