lntravascular Ultrasound–Guided Percutaneous Coronary lntervention: An Updated Review
Dhruv Mahtta, MD, MBA, Ahmed N. Mahmoud, MD, Mohammad K. Mojadidi, MD and lslam Y. Elgendy, MD
1Department of Medicine, University of Florida, 1600 SW Archer Road, Gainesville, FL 32610, USA
2Division of Cardiovascular Diseases, Department of Medicine, University of Florida, 1600 SW Archer Road, Gainesville, FL 32610, USA
Abstract Common practice dictates the performance of percutaneous coronary intervention under conventional angiographic guidance. With studies suggesting the high incidence of intraobserver variability, especially in angiographic borderline lesions, new modalities such as intravascular ultrasound (IVUS) guidance during percutaneous coronary intervention have surfaced. Multiple studies have shown improved outcomes with IVUS guidance, mainly driven by a decrease in ischemia-driven target lesion revascularization. In the past two decades, a multitude of studies have investigated the uses and clinical outcomes associated with this technology. In this review, we highlight the utility, advantages, economic implications, and clinical outcomes of IVUS guidance over standard angiographic guidance, with emphasis on data as they pertain to IVUS-guided stent implantation.
Keywords: bare metal stent; drug-eluting stent; intravascular ultrasound; major adverse cardiac events; outcomes;percutaneous coronary intervention
Background
Since its inception in the 1950s, coronary angiography has been considered the gold standard for defining coronary anatomy, while percutaneous coronary intervention (PCI) remains the mainstay management for obstructive atherosclerotic disease. However, drawbacks of coronary angiography–guided PCI have been well described [1–3].A number of discrepancies exist between apparent angiographic disease severity and the lesion’s true physiologic effect on myocardial perfusion.This disparity is largely due to interobserver and intraobserver variability, the complexity of coronary lesions (tortuosity, overlap of structures, difference in lumen dimensions), and limitations in two-dimensional projection of the lumen [4–7]. The conventional method of quantifying atherosclerotic severity based on percent stenosis relies on the lesion itself in addition to the surrounding “diseasefree” lumen, which is used as a reference. However,studies illustrate that the natural development and progression of atherosclerosis is rather diffuse and seldom consists of a “disease-free” segment [8, 9].The two-dimensional view of angiography allows assessment of only the arterial lumen and precludes the observer from a qualitative or quantitative evaluation of the actual vessel wall. Hence a diffuse,concentric, or symmetrically diseased coronary lumen may present a challenge in true physiologic assessment of the severity of a stenotic lesion. Apart from simple assessment of stenotic lesions, conventional coronary angiography is more prone to inaccurate sizing of stents during PCI. Accurate sizing of stents is essential in attaining improved shortterm outcomes, as well as in preventing late stent thrombosis and in-stent restenosis (ISR). Improper apposition, underexpansion, and inadequate stent length are often the culprits for such future complications [10–12]. Thus sole coronary angiography guidance poses several limitations in identification of true physiologic lesions and proper positioning of stents.
Advantages of lntravascular Ultrasound lmaging
The limitations of coronary angiography in detecting and treating lesions have prompted further interest in other methods for better assessment and intervention. One such method is the use of intravascular ultrasound (IVUS) imaging whereby a catheter with a mini-ultrasound transducer is advanced over the guidewire, visualizing a 360° cross-sectional view of all three arterial layers in addition to the vessel lumen [13]. The use of this technology allows better characterization of coronary plaque burden (including plaque composition, severity, length, and morphology), as well as more precise stent deployment(including proper expansion, extension, and apposition). Providing a direct cross-sectional view, IVUS imaging permits reliable detection of positive arterial wall remodeling during early atherosclerosis,diffusely advanced disease, and complex lesions that may otherwise be difficult to assess with simple angiography [14]. Besides better visualization of the atherosclerotic process within the arterial wall, IVUS imaging has a higher sensitivity for detecting stenotic lesions and thrombi within the arterial lumen [2].
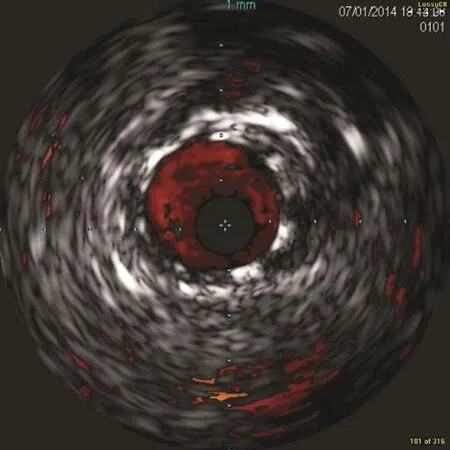
Figure 1 Intravascular Ultrasound Image After Stent Deployment, Showing Adequate Stent Apposition.
IVUS imaging has also been proven to better facilitate the stent deployment process during PCI. As described earlier, two major predictors of ISR or stent thrombosis are stent underexpansion(resulting in smaller intrastent minimum lumen area [MLA]) and the concept of “geographic miss,”where uncovered plaque edges are left behind(Figure 1) [12, 15, 16]. IVUS-guided PCI allows better assessment of stent geometry compared with angiographic guidance, minimizing the incidence of underexpansion or geographic miss. Studies have shown that IVUS guidance results in more frequent use of balloon postdilation. One study demonstrated that despite the initial angiographic appearance of appropriate dilation, nearly 80% of cases required further postdilation when interrogated by IVUS imaging [17]. Larger stent sizes, final larger angiographic minimum lumen diameters (MLDs),and minimum stent areas are also achieved with IVUS guidance [18, 19]. Lastly, IVUS-guided intervention often requires less contrast medium during stent implantation; this is especially advantageous in patients with renal impairment [20, 21].
Clinical Outcomes
Earlier studies in the bare metal stent (BMS) era demonstrated that IVUS guidance achieved a larger MLD within a 6-month follow-up [22]. However,most studies were not powered for clinical end points. In a large meta-analysis of eight randomized trials, Parise et al. [23] demonstrated that IVUS guidance during BMS implantation was associated with a lower incidence of major adverse cardiac events(MACEs) because of a reduction in target lesion revascularization at a follow-up of 6–30 months.However, there was no difference with regard to hard clinical end points, including death and myocardial infarction (MI).
With advances and increased use of drug-eluting stents (DESs), the field of interventional cardiology experienced a revolution through which the risk of restenosis has significantly reduced compared with that in PCI with BMSs [24, 25]. It was initially hypothesized that because of the benefits already offered by DESs over BMSs, the need for an IVUS-guided PCI approach and additional risk reduction may be marginal at best. Earlier studies in the DES era continued to support an increased MLD and reduction in diameter stenosis with IVUS guidance,although these studies were not powered to evaluate clinical outcomes with IVUS guidance [18,19, 26–28]. In a large observational study (~8600 patients), the Assessment of Dual Antiplatelet Therapy With Drug-Eluting Stents (ADAPT-DES),IVUS guidance was superior to conventional angiography in reducing the risk of stent thrombosis,MI, and MACEs (i.e., composite of cardiac death,MI, or stent thrombosis). Approximately 75% of the patients were treated with second-generation DESs (mainly everolimus-eluting stents [EESs]).IVUS guidance resulted in additional procedural optimization that otherwise would not have been performed under simple angiographic guidance. In descending frequency, the common changes were selection of larger stents/balloons, higher inflation pressures, and longer stents. Although the benefit of IVUS guidance was significant in all patient subgroups, they were remarkably apparent in patients with acute coronary syndrome and/or complex lesions [29]. Data from this large study provided further evidence to support the benefit of IVUS guidance in improving outcomes. However, this study was limited by its observational nature, and thus unmeasured confounding variables could not be excluded. Additionally, the decision to use IVUS guidance and further therapeutic changes based on those findings was left to the operator’s discretion.
Several randomized controlled clinical trials evaluated the potential benefit of IVUS guidance for DES implantation (Table 1). Most trials were small and underpowered for clinical outcomes.Moreover, some of these trials were limited to a specific population (e.g., chronic total occlusion[CTO]). In the largest, randomized, multicenter trial to date, Impact of Intravascular Ultrasound Guidance on Outcomes of Xience Prime Stents in Long Lesions (IVUS-XPL), 1400 patients with long coronary lesions (defined as greater than or equal to 28 mm in length) treated with EESs were randomized to receive IVUS guidance before stent implantation versus conventional angiography. At the 1-year, IVUS guidance was associated with a lower rate of composite cardiac death,MI, or target lesion revascularization, which was primarily driven by a lower risk of target lesion revascularization [30]. There was no difference in the risk of hard outcomes (i.e., cardiac death and MI). In a meta-analysis of randomized trials in the era of DESs (i.e., seven trials with 3200 patients),IVUS-guided PCI was associated with significant reduction in risk of MACEs because of a reduction in target lesion revascularization at a mean of 15 months. There was a marginal reduction in stent thrombosis and cardiovascular mortality in the IVUS-guidance group [37]. This meta-analysis was limited because of inclusion of both first-generation and second-generation DESs. In a patientlevel analysis of the three randomized controlled trials (2345 patients) that exclusively used secondgeneration DESs, IVUS guidance was associated with a reduction in the risk of the composite of cardiac death, MI, or stent thrombosis compared with conventional angiography. Furthermore, the risk of MI was reduced with IVUS guidance at 1 year [38]. Several meta-analyses (of observational and randomized controlled trials, and randomized controlled trials alone) were conducted in the past decade to evaluate outcomes with IVUS guidance for implantation of DESs, and these meta-analyses consistently demonstrated a reduction in MACEs,mostly due to a reduction in target lesion revascularization (Figure 2). These studies collectively demonstrate the superiority of IVUS-guided intervention irrespective of stent type (BMS, first- or second-generation DES). This benefit is further enhanced for longer lesions. In a metaregression analysis of 14 randomized trials, irrespective of stent type, for every 10-mm increase in lesion length, the risk of MACEs decreased by approximately 19%(P = 0.037) at a mean of 14 months [43].
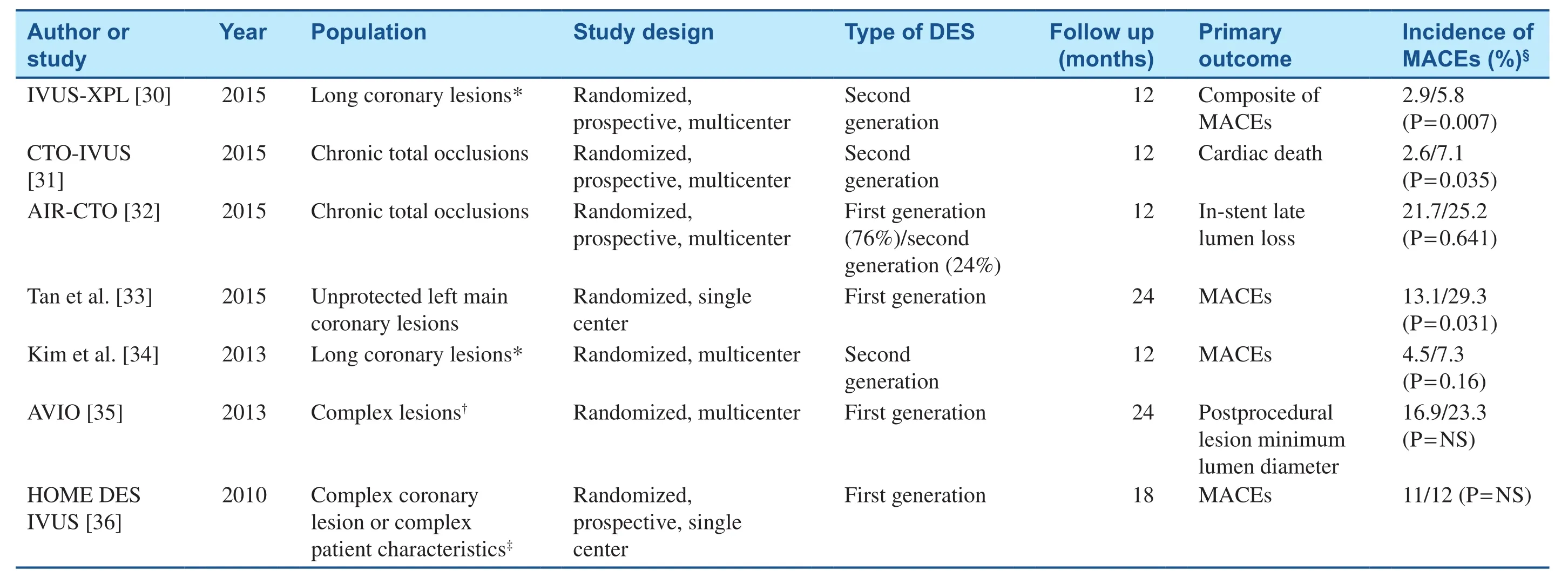
Table 1 Studies Comparing Drug-Eluting Stent (DES) Implantation with Intravascular Ultrasound Guidance Versus Conventional Angiographic Guidance.
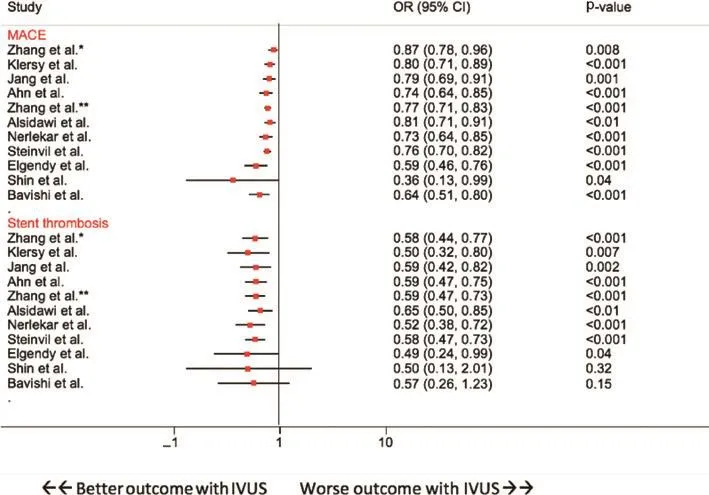
Figure 2 Summary Estimates for Major Adverse Cardiac Events (MACEs) and Stent Thrombosis Across the Meta-analyses Conducted in the Era of Drug-Eluting Stents (Zhang et al. [26], Klersy et al. [27], Jang et al. [18], Ahn et al. [19], Zhang et al.[28], Alsidawi et al. [39], and Nerlekar et al. [40], Meta-analysis of Observational Studies and Randomized Trials; Steinvil et al. [41], Elgendy et al. [37], Shin et al. [38], and Bavishi et al. [42], Meta-analysis of Randomized Trials Only).CI, confidence interval; HR, hazard ratio; IVUS, intravascular ultrasound guidance OR, odds ratio; RR, risk ratio.
The US Food and Drug Administration approved the use of the Absorb bioresorbable vascular scaffold; however; there have been growing concerns regarding the increased risk of adverse events, in particular scaffold thrombosis, with this current first-generation bioresorbable vascular scaffold with regard to mid-term to long-term outcomes [44].Some authors suggested that an optimal implantation technique with a more liberal use of IVUS guidance could mitigate the risk of scaffold thrombosis.For example, in a real-world cohort of 400 lesions treated with bioresorbable vascular scaffolds in 264 patients, IVUS guidance was used in approximately 86% of the lesions, and only three patients had definite or probable scaffold thrombosis at 2 years [45].Because of growing concerns over the higher incidence of adverse events, the bioresorbable vascular scaffold system was recalled by its manufacturer,Abbott Vascular, in April, 2017.
lVUS Guidance in Special Situations
The concept behind improvement in angiographic and clinical outcomes with the use of IVUS guidance during PCI is largely attributed to better visualization, which allows larger MLD and greater stent cross-sectional area to minimize geographic miss. With this in mind along with findings of the landmark trials, the interventional cardiology community turned its attention to investigating the role of IVUS guidance in special circumstances such as CTOs and left main coronary artery (LMCA)lesions.
Studies have shown better outcomes in patients with successful recanalization of CTOs compared with their counterparts with failed attempts at percutaneous recanalization [46–48]. With the IVUS-guided PCI technique gaining popularity, several studies suggested that the use of IVUS-guided wiring may better facilitate successful CTO recanalization via use of the side branch [49–51]. This technique’s effect on clinical end points was tested by researchers in two multicenter, prospective,randomized controlled trials. The Chronic Total Occlusion Intervention with Drug-Eluting Stents(CTO-IVUS) study was the first randomized trial to investigate improvement in clinical end points after DES implantation with IVUS guidance versus angiography guidance during CTO intervention[31]. Patients were followed up for 12 months, the IVUS-guidance group had significantly lower rates of MACEs (defined as the composite of cardiac death, MI, or target vessel revascularization) (2.6%vs. 7.1%, P = 0.035, 95% confidence interval 0.13–0.97). The Angiographic and Clinical Comparisons of Intravascular Ultrasound Versus Angiography-Guided Drug-Eluting Stent Implantation for Patients with Chronic Total Occlusion Lesions(AIR-CTO) study was another randomized controlled trial, where the authors investigated differences in late lumen loss between IVUS-guided and angiography-guided CTO interventions [32].This study showed that when IVUS-guided CTO PCI was associated with reduced late lumen loss,ISR, and stent thrombosis as compared with angiographic guidance. However, improvement in these measures did not translate into significant reduction of composite MACEs because of the small number of patients enrolled in the study.
Two recent randomized trials (i.e., EXCEL and NOBLE) compared PCI using a DES with bypass surgery for an unprotected LMCA [52, 53]. While the EXCEL trial showed that PCI with an EES had comparable clinical outcomes to coronary artery bypass graft for an unprotected LMCA at 3 years,the NOBLE trial concluded that coronary artery bypass graft was superior to use of a DES at 5 years.Some authors have suggested that these discrepant findings might have been attributed to more prevalent use of IVUS guidance in the EXCEL trial[54]. This was supported by two medium-sized propensity-matched analyses (i.e., approximately 1000 patients in the first study from Spain and approximately 300 patients in the second study from Korea) that demonstrated that IVUS guidance use was associated with better outcomes for unprotected LMCA PCI compared with conventional angiography [55, 56]. Table 2 summarizes the studies that have investigated the use of IVUS guidance versus conventional angiographic guidance during LMCA PCI.
lVUS and Other lnvestigatory Modalities
Another modality that has been used to guide PCI in the modern era is fractional flow reserve (FFR),which relies on pure physiologic assessment of coronary stenosis. Compared with conventional angiographic guidance, FFR-guided PCI has been shown to improve clinical outcomes and reduce MACEs [58]. Correlation between the physiologically ischemia-producing lesions and IVUS imaging findings has been evaluated by several researchers. Jasti et al. [59] showed that in patients with angiographically ambiguous LMCA disease,there is a strong correlation between IVUS imaging parameters and FFR calculation. IVUS imaging parameters studied by the authors included MLD,MLA, and cross-sectional narrowing. Of all these parameters, MLA of 5.8 mm2and MLD of 2.8 mm had the strongest correlation with physiologicallysignificant LMCA stenosis. Other authors have conducted similar studies looking at correlations between these two modalities for non-LMCA stenosis. Moderate correlation between the IVUS imaging parameter of MLA and FFR of less than 0.8 has been documented for non-LMCA lesions.Plaque morphology as seen on IVUS imaging was not shown to correlate with FFR findings [60]. It is suggested that the degree to which MLA correlates with FFR may be vessel dependent, being particularly limited in ischemic lesions within small vessels [61]. The modest correlation between IVUS imaging findings and FFR is also in part due to the need for different cutoff values depending on the location of the lesion and the amount of myocardium supplied by the target vessel [62].
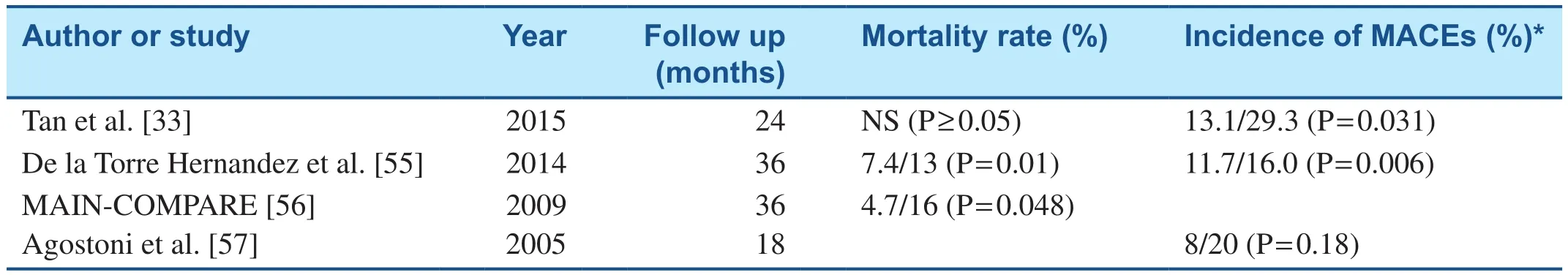
Table 2 Studies Comparing Percutaneous Coronary Intervention with Intravascular Ultrasound Guidance Versus Conventional Angiographic Guidance in Patients with Left Main Coronary Artery Disease.
Optical coherence tomography (OCT) and instantaneous wave-free ratio (iFR) are worth mentioning at this juncture. Although OCT can provide higher-resolution images as compared with IVUS imaging, some studies have shown that OCT-guided stent implantation resulted in smaller postprocedural luminal diameter [63]. In the ILUMIEN III: OPTIMIZE PCI trial, OCT guidance was noninferior to IVUS guidance but was also not superior to IVUS guidance or angiographic guidance in terms of median minimum stent area [64]. The DEFINE-FLAIR (Functional Lesion Assessment of Intermediate Stenosis to Guide Revascularization)and the iFR-SWEDEHEART (The Instantaneous Wave-Free Ratio versus Fractional Flow Reserve in Patients with Stable Angina Pectoris or Acute Coronary Syndrome) trials compared use of iFR with FFR and concluded that iFR-guided revascularization was noninferior to FFR-guidance with respect to MACEs at the 1-year follow-up. The rate of adverse procedural symptoms and the procedure time were less in the iFR-guidance cohort [65, 66].
Economic lmpact of lVUS Use
The use of IVUS technology comes with associated costs and potential increased procedure time. This was further explored in an Italian study by Alberti et al. [67]. The cost-effectiveness of this technology was utmost evident in patients with additional medical comorbidities such as diabetes or chronic kidney disease, or in patients with ACS. However,with longer follow-up (mainly more than 1 year),the incremental cost difference between angiographic-guided and IVUS-guided PCI started to decline. Although the additional cost benefit of this technology was most apparent during the first year after stent implantation, we know from prior metaanalyses that the clinical benefits of this technology still hold true over a longer follow-up [19]. Lastly,Alberti et al. reached a reassuring conclusion that the incremental cost added by IVUS-guided PCI remained below the willingness-to-pay threshold in the Italian population, thereby establishing it as a concrete therapeutic strategy.
Final Remarks
Although evidence exists regarding improvement in clinical and angiographic outcomes with the use of IVUS guidance, the interventional cardiology community has continued to show hesitance in adopting this technology during routine PCIs. This is evident by the rate of IVUS guidance use of approximately 20% in the United States and even lower in some other countries [68]. It is speculated that this may be related to the cost of the equipment and lack of financial reimbursement [69]. Given that evidence suggests greater benefit in clinical outcomes for complex cases such as LMCA disease, complicated coronary anatomy, longer lesions, or CTOs, IVUS guidance should be considered for these interventions even in the DES era.
Conflict of lnterest
The authors declare no conflicts of interest.
Funding
This research received no specific grants from any funding agency in the public, commercial, or nonprofit sectors.REVlEW
 Cardiovascular Innovations and Applications2018年3期
Cardiovascular Innovations and Applications2018年3期
- Cardiovascular Innovations and Applications的其它文章
- Speckle Tracking Echocardiography ldentifies lmpaired Longitudinal Strain as a Common Deficit in Various Cardiac Diseases
- Current Status of Coronary Atherectomy
- The Use of Direct Oral Anticoagulants for Prevention of Stroke and Systemic Embolic Events in East Asian Patients with Nonvalvular Atrial Fibrillation
- Bioresorbable Vascular Scaffold in the Midportion of the Left Anterior Descending Artery for Cardiac Allograft Vasculopathy in a Cardiac Transplant Patient
- The Contemporary Role of Femoral Artery Access
- Cardiovascular Innovations and Applications
