Current Status of Coronary Atherectomy
Ahmad A. Mahmoud, MD, Ahmed N. Mahmoud, MD, Akram Y. Elgendy, MD and R. David Anderson, MD
1Division of Cardiovascular Medicine, Department of Medicine, University of Florida, 1600 S.W. Archer Rd., P.O. Box 100277,Gainesville, FL 32610-0277, USA
Abstract There are several techniques for performing coronary atherosclerotic plaque modification, known as atherectomy. Historically, clinical trials show mostly equivalence between various coronary atherectomy techniques, balloon angioplasty,and percutaneous coronary stenting. In the last several years the use of a given atherectomy technique has been mostly as a means of facilitating stent delivery in vessels that are heavily calcified. No clinical trials have shown superiority of any atherectomy method over more standard techniques of percutaneous coronary intervention. This review begins with a discussion of directional atherectomy, which is no longer available. The rotational atherectomy technique and its clinical trial data are presented. Orbital atherectomy is then discussed in detail, including the relevant clinical trials. Finally, laser atherectomy techniques are reviewed, and the pertinent trial data are presented. Lastly, future directions are detailed.
Keywords: coronary artery disease; percutaneous coronary intervention; atherosclerotic plaque
lntroduction
Coronary atherectomy is defined as removal of atherosclerotic plaque from the intimal layer of the coronary arteries. Although coronary atherectomy is considered a technically demanding intervention,it plays a key role in preparation of heavily calcified vessels before stent implantation [1]. Common techniques of coronary atherectomy include directional atherectomy, rotational atherectomy, orbital atherectomy, and excimer laser atherectomy. The use of atherectomy during percutaneous coronary intervention (PCI) has evolved dramatically, from the historical directional atherectomy to more modern modalities, such as orbital atherectomy.In this review, we discuss the history, the technical aspects, and the clinical evidence behind the efficacy and safety of each coronary atherectomy modality, with an emphasis on the optimal technique to avoid unnecessary complications.
Methods
We searched MEDLINE, PubMed, and Web of Science for all observational studies or clinical trials conducted on directional, rotational, orbital,or laser coronary atherectomy from inception to August 2017. The search was limited to human studies and the English language. The keywords“directional,” “rotational,” “orbital,” “laser,”“atherectomy,” “coronary,” and “percutaneous”were used. Of an initial 550 records, 74 were included in the study.
Types of Coronary Atherectomy
Directional Coronary Atherectomy
Directional coronary atherectomy (Figure 1) was approved by the FDA in 1990 [3] as a catheter equipped with a cup-shaped rotating cutting system that faces the lesion through a window in the side of the atherectomy device [4]. A 2 mm balloon is present on the side opposing that window. First, the atherectomy catheter is advanced across the lesion over the guidewire. The balloon is then inflated,displacing the exposed cutting system toward the lesion. The rotating cutter is then activated and used to remove layers of the plaque, which are compressed in the device housing. The atherectomy catheter is then withdrawn and the aspirated debris is removed. The catheter can be used more than once until the optimum angiographic results are obtained [4].
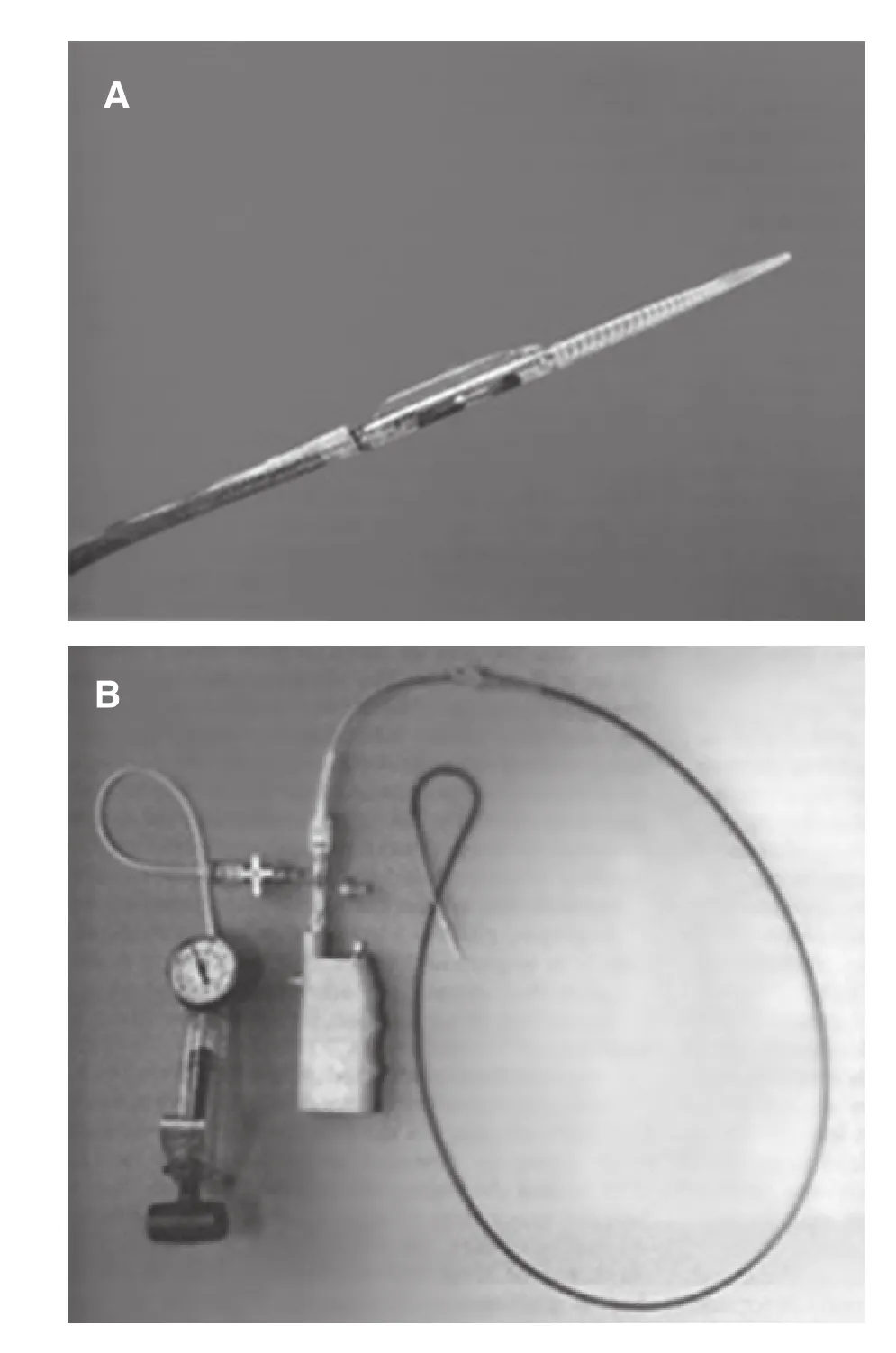
Figure 1 Directional Atherectomy Device.
In the Balloon vs. Optimal Atherectomy Trial(BOAT) [3], 1000 patients were randomized to undergo either directional coronary atherectomy or percutaneous transluminal coronary angioplasty(PTCA). There was more luminal gain in the directional coronary atherectomy arm than in the PTCA arm early in the trial. However, at the 1-year clinical follow-up, there was no significant reduction in the mortality rate, target-lesion revascularization (TLR)rate, target-vessel revascularization (TVR) rate, or target-vessel failure rate (including Q-wave myocardial infarction, TVR, or death) with directional atherectomy compared with PTCA. This technique is obsolete, and directional coronary atherectomy is currently not commercially available in the United States for treatment of patients with coronary artery disease.
Rotational Atherectomy
In 1987, Ritchie et al. [5] introduced rotational atherectomy as a technique for endovascular treatment of obstructive atherosclerotic disease in animal models. In the 1990s, rotational atherectomy also emerged as an alternative to balloon angioplasty[6, 7]. However, since the development of coronary stenting, rotational atherectomy has served mainly as a facilitator for stent delivery in complex and typically calcified coronary lesions.
Tech nical Aspects
Rotational atherectomy is performed with a diamond-coated, nickel-plated, elliptical burr. The diamond crystals are 20 μm in size and located in the leading edge, ranging from 2000 to 3000 in number. The commercially available rotational atherectomy system is the Rotablator (Boston Scientific Corporation; Scimed, Plymouth, MN,USA) (Figure 2). The burr operates in a range of 140,000–190,000 rotations per minute (rpm) over a 0.009-inch guidewire and the sizes range from 1.25 to 2.5 mm in diameter. The burr size is usually increased in 0.25–0.5 mm increments until the desired result is achieved. A cocktail flush is used as a lubricant during the procedure, usually consisting of nitroglycerine, verapamil, heparin, anda specifically manufactured lubricant (Rotaglide)[8, 9]. Because of the high-speed rotation of the burr, it has the ability to differentiate between inelastic structures (e.g., calcium or fibrous tissue) and healthy intima that usually deflect away the cutting edges of the device. Also, such high-speed rotation can facilitate device advancement through tortuous vessels and tight lesions [10, 11].
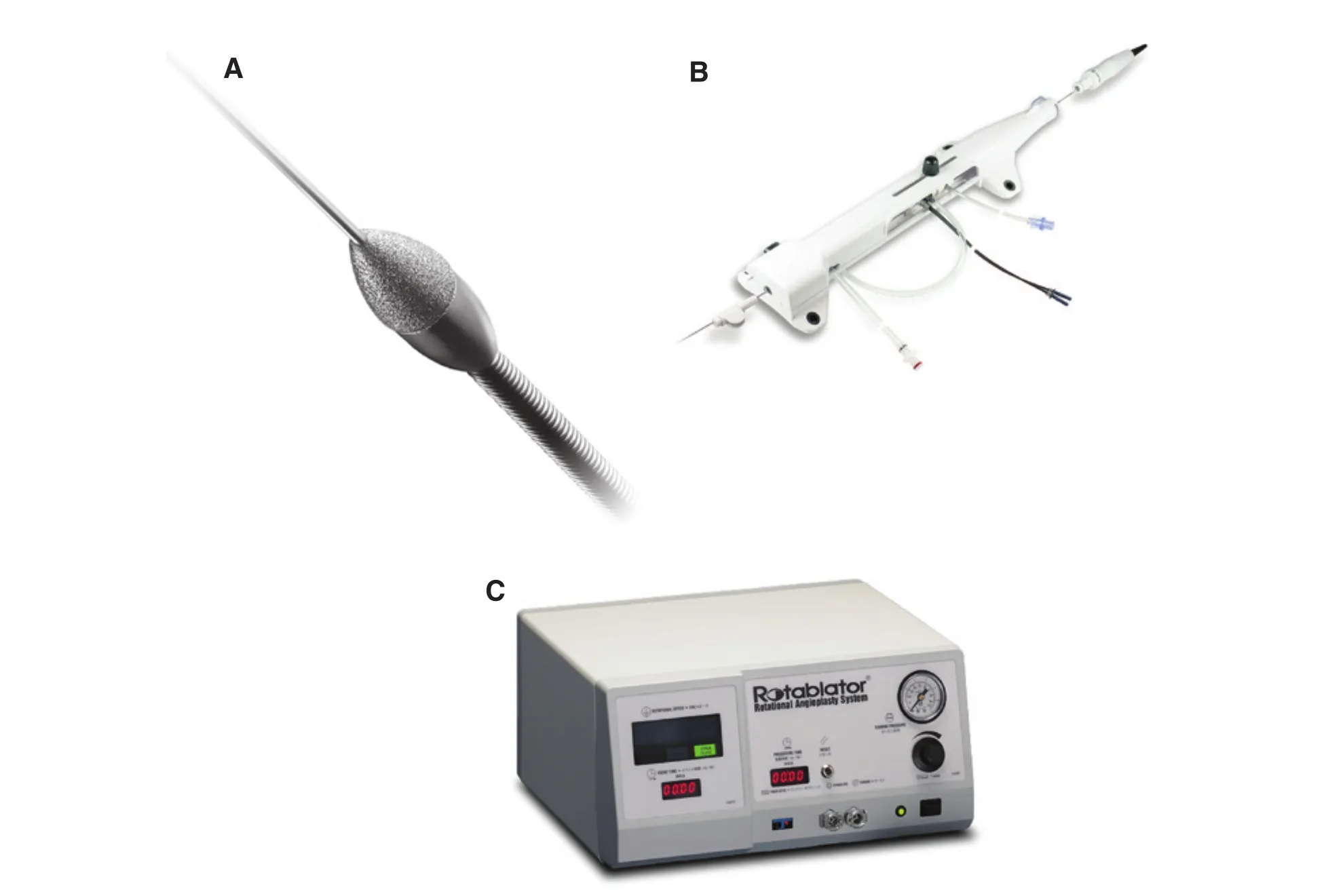
Figure 2 Rotablator Rotational Atherectomy System.
Clinical Evidence behind the Efficacy and Safety of Rotational Atherectomy
Patients undergoing rotational atherectomy may experience complications related to PCI such as vascular access complications, stroke, and the need for urgent coronary artery bypass graft surgery;angiographic complications such as dissection, perforation, slow flow/no reflow, or side branch loss; or rotational atherectomy–specific complications such as vasospasm or burr entrapment [11–13]. Multiple large, multicenter trials have evaluated the efficacy and safety of rotational atherectomy compared with PTCA and PCI. The randomized Comparison of Balloon Angioplasty versus Rotational Atherectomy(COBRA) in complex coronary lesions study [14]was a prospective, randomized, multicenter trial that enrolled 502 patients with complex calcified coronary lesions. Patients were randomized to undergo either PTCA or rotational atherectomy. Procedural success was comparable between the groups, with no significant differences in periprocedural complications. At the 6-month follow-up, there was no significant difference in the rate of TVR or recurrence of symptoms between rotational atherectomy and PCI.
In the Dilatation vs. Ablation Revascularization Trial (DART) [15], 446 patients with nonseverely calcific angiographic stenosis in small vessels were randomized to undergo either PTCA or rotational atherectomy. Rotational atherectomy was found to be safe; however, it provided no additional benefit over conventional PTCA with respect to TVR rates at 12 months. In the randomized Rotational Atherectomy prior to Taxus Stent Treatment for Complex Native Coronary Artery Disease(ROTAXUS) trial [16], 240 patients with calcified complex coronary lesions were randomly assigned to undergo either rotational atherectomy followed by drug-eluting stent implantation or conventional stenting without prior rotational atherectomy.The rates of procedural success and initial luminal gain were higher in the rotational atherectomy group. However, at follow-up at 9 months there was more luminal loss in the rotational atherectomy group because of TVR. The adverse events in the rotational atherectomy group were in-stent restenosis (11.4%), TLR (11.7%), stent thrombosis(0.8%), and major adverse cardiac events (MACE)(24.2%). There was no significant difference in the incidence of these complications between both groups. At 2 years, the incidence of MACE corresponded to about one-third of the patients in each group, with no differences in death rate (rotational atherectomy group vs. standard therapy; 8.3%vs. 7.4%,P= 1.00), TLR rate (13.8% vs. 16.7%,P= 0.58), TVR rate (19.3% vs. 22.2%,P= 0.62)and myocardial infarction rate (8.3% vs. 6.5%,P= 0.80) [17].
In the Angioplasty versus Rotational Atherectomy for Treatment of Diffuse In-Stent Restenosis Trial(ARTIST) [18], 298 patients with significant instent restenosis within bare metal stents (>70%)that occurred more than 3 months after implantation were randomly assigned to undergo either PTCA or rotational atherectomy followed by low-pressure PTCA. There was comparable immediate procedural success in both groups. During long-term follow-up, the PTCA group had more net luminal gain than the rotational atherectomy group when assessed by coronary angiography 6 months after intervention. The 6-month event-free survival rate was higher in the PTCA group than in the rotablation group (Table 1).
In a recent meta-analysis of 22 studies evaluating the efficacy of various lesion modification techniques, including rotational atherectomy, lesionmodification was found to be associated with a lower risk of TLR and MACE at 1 year. This effect was more pronounced in randomized clinical trials than in observational studies [19]. Table 1 summarizes major trials comparing rotational atherectomy with conventional PTCA/PCI.
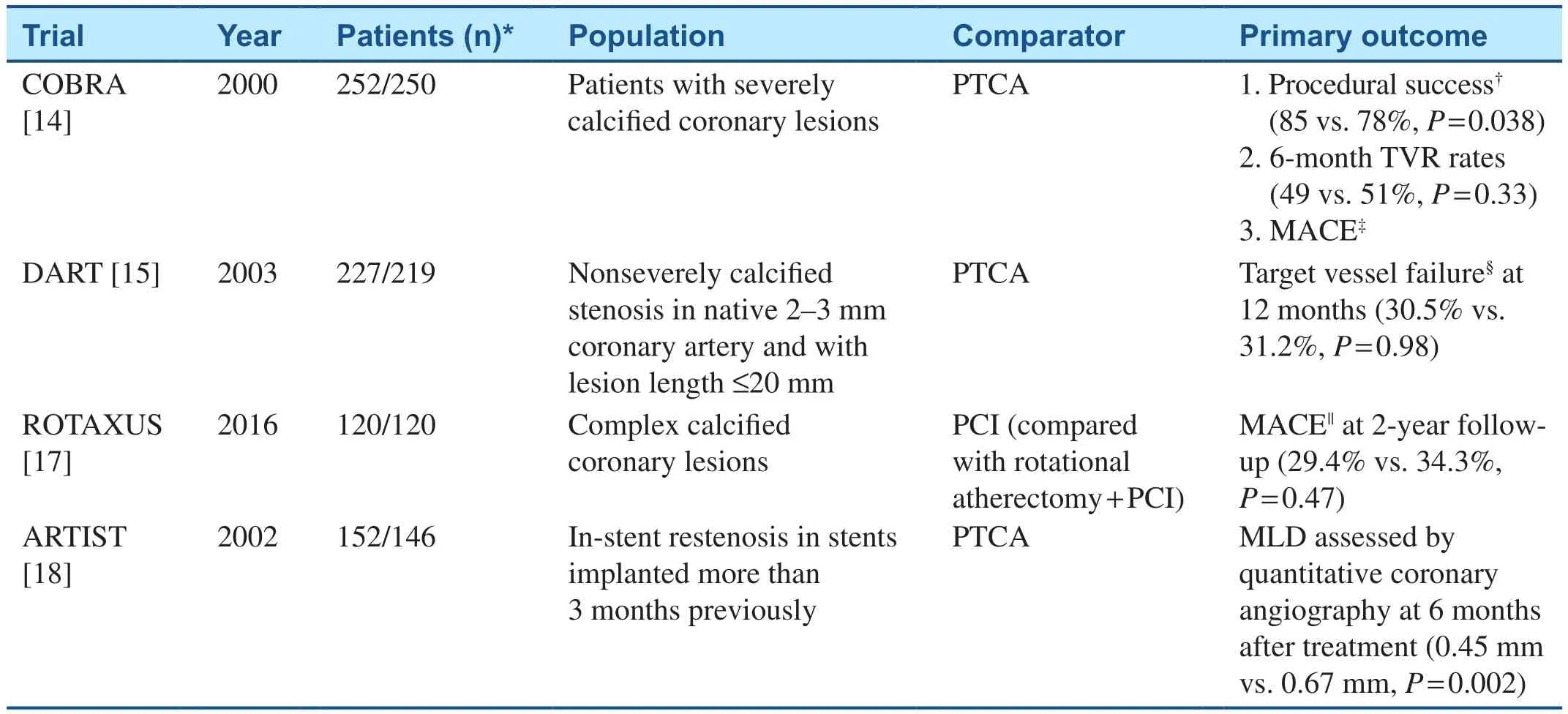
Table 1 Clinical Trials that Compared the use of Rotational Atherectomy with Conventional Percutaneous Coronary Intervention (PCI).
Useful Techniques to lmprove the Safety of Rotational Atherectomy
Heat is produced by burr-lesion friction [20].This produced heat may cause excessive platelet aggregation and vessel injury [21]. This could be reduced by intermittent ablation with backing out of the lesion and avoiding burr deceleration of more than 5000 rpm [11]. Also, this technique helps in the production of smaller particulate, thus decreasing the risk of distal microembolization and slow/no reflow, which is the most common complication in rotational atherectomy [11, 22–25]. Continuous flush using the previously mentioned cocktail infusion during the procedure helps reduce the heat produced, decreasing the incidence of vasospasm,and flushing the microparticles through the distal microcirculation [8]. Also, glycoprotein IIb/IIIa inhibitors could be used to reduce the incidence of slow/no reflow [25]. In a randomized clinical trial that enrolled 100 participants, however, there was no difference in the incidence of slow flow with low-speed rotational atherectomy (140,000 rpm)compared with high-speed rotational atherectomy(190,000 rpm) [22].
Burr entrapment is one of the dreaded complications in rotational atherectomy. It occurs because of advancement of the burr through a nonadequately dilated lesion, and is thought to be due to a lack of ablating surface on the back of the burr. This could be avoided by a more gradual advancement of the burr and backing out of the lesion when deceleration occurs [11]. When burr entrapment occurs,removal is necessary by either aggressive positioning of the guiding catheter or balloon dilation [11,26–28]. Surgical removal is rarely indicated.
The risk of perforation and distal embolization can be reduced by use of smaller burr sizing (burrto-artery ratio less than 0.7) while having the same rate of procedural success and with fewer angiographic complications than more aggressive sizing(burr-to-artery ratio greater than 0.7) [11, 29, 30].Also, bleeding from the vascular access site is one of the complications that can be decreased by use of a smaller sheath size, radial access, and smaller burr sizing [31–33]. Rotational atherectomy is often needed in patients with a greater burden of atherosclerosis and vascular calcification, with greater liability for aortic debris mobilization causing stroke [34, 35]. Smaller guiding catheters may limit the incidence of stroke associated with rotational atherectomy [35].
Summary
Rotational atherectomy appears to be generally safe when compared with PTCA or PCI alone in highly calcific lesions. However, the evidence supporting its long-term benefit in terms of TVR rate reduction and its use as a primary device is not robust. The use of this technique should be on a case-to-case basis and should be primarily reserved for patients with a low risk of adverse events and where its use might facilitate stenting.
Orbital Atherectomy
Technical Aspects

Figure 3 Diamondback 360 Orbital Atherectomy System.
Orbital atherectomy is another method used for heavily calcific atherosclerotic lesion modification[36]. The Diamondback 360 orbital atherectomy system (Cardiovascular Systems Inc., St. Paul,MN, USA) (Figure 3) has a diamond-coated crown that is nearly similar in structure to that of the Rotablator, but the crown is eccentrically mounted and has the ability to expand laterally, increasing the luminal diameter by increasing the rotational speed [37]. The faster rotation will create more centrifugal force, and increase the orbital rotation diameter, without the need for the use of multiplesized catheters. The rotational speed ranges from 60,000 to 200,000 rpm. As the crown orbits around the wire and along the periphery of the vessel, it creates a sanding action that removes a layer of the plaque with each pass. Theoretically, the more elastic healthy vessel wall tissue will deviate away from the crown, in contrast to the calcified plaques,which are more rigid and have more friction with the orbiting crown. This differential vessel wall and plaque modification minimizes the risk of vessel wall trauma [36].
The orbital atherectomy system crown has different shapes (classic, solid, and micro solid). The solid crown achieves larger lumens in larger vessels because of greater weight. The crowns should be advanced over a stainless steel, silicone-coated ViperSlide. Continuous lubricant and saline infusions are used during atherectomy runs to decrease friction [38].
Orbital atherectomy ablates in both directions, as opposed to rotational atherectomy, decreasing the risk of entrapment [39]. Also, the gradual increase in the ablation’s diameter in orbital atherectomy by increasing the rotation speed facilitates the procedure, as a 6 F guiding catheter can be used for all cases. This decreases the need for catheter exchanges and the use of larger guides (≥7 F guiding catheter)that are needed when rotational atherectomy burrs more than 1.25 mm in diameter are used [39]. The orbital atherectomy system provides a single point of contact with the vessel wall when rotating. This prevents the device from obstructing flow, helps to minimize the generation of heat, and allows for continuous clearance of microscopic particulate matter. Also, orbital atherectomy releases particles that are smaller in diameter (2 μm) compared with rotational atherectomy (5 μm). This decreases the potential incidence of distal microvascular obstruction, and the incidence of the subsequent slow/no reflow with orbital atherectomy use (0.9%) compared with rotational atherectomy use (2–20%) [22,38, 40–43].
Orbital atherectomy ablates through the whole vessel diameter. This may help to decrease the incidence of asymmetrical ablation, which happens more with rotational atherectomy, especially in angulated and eccentric vessel lesions because of wire bias as it may come in contact more with one side of the vessel wall [39].
Clinical Evidence behind the Efficacy and Safety of Orbital Atherectomy
The ORBIT I trial [44] evaluated the safety and performance of an orbital atherectomy system in treating de novo calcified coronary lesions. Among 50 enrolled patients, the device success rate was 98%, and the procedural success rate was 94%.The cumulative major adverse in-hospital cardiac event rate was 4% (two non–Q-wave myocardial infarctions). Angiographic complications included six dissections and one perforation [44]. ORBIT II enrolled 443 patients with severely calcified coronary lesions. The orbital atherectomy system was used to modify calcified lesions before stent placement. A stent was successfully delivered in 97.7% of cases, and there were low rates of inhospital Q-wave myocardial infarction (0.7%), cardiac death (0.2%), and TVR (0.7%) [40] (Table 2).On follow-up of the ORBIT II participants for 3 years, the overall 3-year MACE rate was 23.5%,including cardiac death (6.7%), TVR (10.2%),and myocardial infarction (11.2%), and the 3-year TLR rate was 7.8% [45]. Although ORBIT I and ORBIT II showed that orbital atherectomy was safe and effective for the treatment of calcific lesions, both were single-arm trials, which did not compare orbital atherectomy with conventional PCI or rotational atherectomy. The Evaluation of Treatment Strategies for Severe Calcific Coronary Arteries: Orbital Atherectomy vs. Conventional Angioplasty prior to Implantation of Drug-Eluting Stents (ECLIPSE) trial is an ongoing multicenter,randomized prospective trial and will shed more light on the efficacy of orbital atherectomy compared with standard PCI.
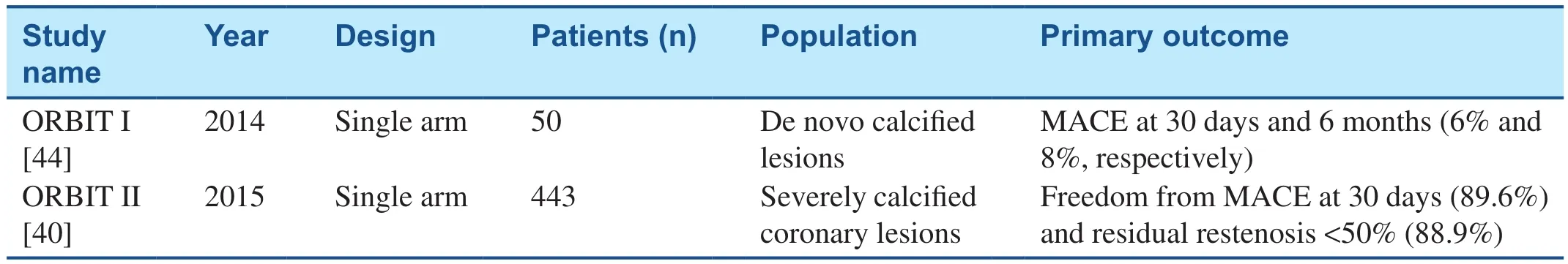
Table 2 Clinical Trials that Evaluated the Efficacy and Safety of Orbital Atherectomy.
In ORBIT I and ORBIT II, many high-risk patient subsets were excluded, such as those with kidney disease, recent myocardial infarction, long diffuse disease, severe left ventricular dysfunction, or unprotected left main coronary artery disease. This might have impacted the results of both trials. In a retrospective study including 458 high-risk patients with severe coronary artery calcification who were treated with orbital atherectomy before stenting, the MACE incidence at 30 days was only 1.7%. TLR,stroke, stent thrombosis, and 30-day all-cause death were infrequent as well [46]. Table 2 illustrates major clinical trials evaluating the efficacy and safety of orbital atherectomy.
Useful Techniques to lmprove the Safety of Orbital Atherectomy
Orbital atherectomy is mainly a time-dependent procedure. Luminal gain in orbital atherectomy will be more with slower advancement at lower rotational speed than with faster advancement at a higher rotational speed. The nose cone of the device is initially placed at the lesion without being fully occlusive. Then the device is advanced slowly, initially at lower rotational speed, with maintaining a transverse advancement speed of 1–3 mm per second at the target lesion. The recommended run time should not exceed 30 seconds, with a total treatment time not exceeding 5 minutes, and rest time between the runs equal to or more than the run time[47]. This technique also allows more prolonged contact and relative increase at the flow rate of the lubricant (ViperSlide) to help to wash out the microparticles and to achieve a smoother wall for better stent opposition [48, 49].
ViperWire is a stiffer wire than the usual workhorse coronary guidewire. Securing the distal end of the wire during advancement of the device is important to avoid complications such as wire perforation or system disengagement due to distal wire migration. Usually a skilled assistant is needed; however,in a single-center study, single operator technique was feasible with comparable safety [50].
Summary
Orbital atherectomy appears to be a promising modality for treatment of highly calcific lesions.However, most of the current evidence is based on single-arm trials, and thus more evidence from the ongoing case-control and randomized clinical trials is mandatory for further evaluation of the efficacy and safety of this procedure.
Excimer Laser Atherectomy
The use of laser atherectomy in animal models dates back to 1983. It was first used in experimental atherosclerotic plaque ablation in 1985 [51].
Technical Aspects
Laser atherectomy uses a high-energy, monochromatic light beam to vaporize the plaque without damaging the surrounding tissue. In the past, an argon laser and a neodymium–yttrium aluminum garnet laser were used. However, they had deep tissue penetration and the energy was delivered in a continuous output form, causing excessive adjacent tissue damage and complications such as vasospasm, thrombosis, and perforation [51–54].Currently, endovascular interventions use a xenon chloride (XeCl) excimer laser. A XeCl excimer laser has high energy and short penetration depth,and the light is delivered with a short interaction time, minimizing thermal energy release. This focuses the ablation to the area the laser beam is touching, minimizing surrounding tissue damage,leading to less incidence of thrombosis, vasospasm, and restenosis [51, 53]. An excimer laser can also vaporize thrombi, suppressing platelet aggregation, and vaporize procoagulant reactants, in addition to debulking the underlying plaque, facilitating stent delivery [55, 56]. The light is delivered via a fiber-optic catheter in pulses [57]. Each pulse of energy removes a thickness of 10 μm of tissue[58]. Typically, the pulse repetition rate is usually 25–40 per second. The catheter should be advanced slowly (0.5 mm per second and no faster than 1 mm per second) to create a large and smooth track because of shallow penetration [51]. Iodinated dye and blood (hemoglobin) absorb the excimer laser energy, causing cavitations, vapor bubbles, and percussive waves, leading to dissections or perforations [59–61]. Saline infusion before and during catheter advancement has resulted in improvements in both angiographic and clinical outcomes [51,61]. Currently CVX-300 (Spectranetics, Colorado Springs, CO, USA) is the commercially available system used in coronary laser atherectomy.
Clinical Evidence behind the Efficacy and Safety of Excimer Laser Atherectomy
In the CARMEL multicenter study [62], excimer laser angioplasty was successfully used in more than 90% of the enrolled 151 acute myocardial infarction patients (65% of the patient population had grade III–IV angiographic thrombus burden,and in 21% the saphenous vein graft was the target vessel), with a relatively low rate (8.6%) of MACE.However, as it was a single-arm trial there is limited evidence regarding the added benefit of excimer laser angioplasty compared with standard-care PCI [62]. In the Coronary Graft Results following Atherectomy with Laser (CORAL) study, excimer laser atherectomy was used in patients with saphenous vein graft disease [63]. There was a high initial technical success rate, and a low rate of events attributed to the use of the laser itself. This safety profile was present despite a patient population that had smaller reference vessel diameters, more thrombus, more vessel angulation, and smaller minimal lumen diameter when compared with patients in the Saphenous Vein Graft Angioplasty Free of Emboli Randomized (SAFER) trial [64] control group. However, when compared with the distal occlusion device (PercuSurge GuardWire) arm,which had significant benefit with its use in terms of reduction in the rate of MACE (death, myocardial infarction, emergency bypass, and TVR) at 30 days,CORAL patients had a significantly higher 30-day MACE rate, suggesting a lack of significant benefit with excimer laser use in saphenous vein graft interventions.
In the Laser Angioplasty for Restenotic Stents(LARS) multicenter trial, laser angioplasty and PTCA were used for the treatment of in-stent restenosis and compared with the use of stand-alone PTCA. Patients treated with excimer laser atherectomy had a reduced rate of repeated target-site coronary intervention at 30 days, but not at a later follow-up. Also, the incidence of MACE was similar between both groups [65].
Summary
There is no apparent added benefit to the use of an excimer laser in the treatment of in-stent restenosis and there is evidence of worse outcomes when it is used in saphenous vein graft disease. Thus we recommend against the routine use of such a modality as an adjunct to PCI/PTCA until further data are available.
Comparison of Efficacy of Different Coronary Atherectomy Modalities
The Excimer Laser, Rotational Atherectomy, and Balloon Angioplasty Comparison (ERBAC) study[66] involved 685 patients randomized to undergo various PCI methods, including excimer laser atherectomy, rotational atherectomy, and conventional balloon angioplasty in a single center.Rotational atherectomy had the greatest initial procedure success (89% vs. 77% vs. 80%, respectively), but no difference was observed in the rates of major in-hospital complications at follow-up at 6 months. Revascularization of the original target lesion was performed more frequently in the rotational atherectomy group (42.4%) and the excimer laser atherectomy group (46.0%) than in the balloon angioplasty group (31.9%,P= 0.013) [66].Currently, the most commonly used techniques for atherectomy are rotational atherectomy and orbital atherectomy. However, multicenter randomized clinical trials are needed to compare the procedural success, clinical safety, and efficacy in the treatment of calcified coronary lesions.
Use of lntravascular Ultrasound lmaging for Coronary Atherectomy
In a post hoc analysis of the ORBIT II trial, patients who underwent intravascular ultrasound (IVUS)imaging before orbital atherectomy (n= 35) were compared with patients who did not undergo IVUS imaging for initial lesion assessment (n= 405).Procedural outcomes and the 3-year MACE rate were evaluated. There was a significant reduction in the number of stents used in patients who underwent IVUS imaging before orbital atherectomy and increased postorbital atherectomy mean minimal lumen diameter. The 3-year MACE rate was similar in both groups, however [67]. This may be explained by the enhanced ability of IVUS imaging to detect target-lesion calcification [68]. Optical coherence tomography (OCT)was also used to compare the effects of rotational and orbital atherectomy on plaque modification in severely calcified coronary lesions [69]. The incidence of dissections was comparable between rotational atherectomy and orbital atherectomy. Orbital atherectomy resulted in deeper postatherectomy dissections (lacunae) shown by OCT. This might also explain the better stent apposition found after orbital atherectomy compared with rotational atherectomy. However, the impact on long-term outcome remains to be determined [69].
Cost-Effectiveness of Coronary Atherectomy
In a carefully selected population, coronary atherectomy seems to be cost-effective. The cost-effectiveness of orbital atherectomy in US patients older than 65 years was evaluated in a post hoc analysis, where patients undergoing orbital atherectomy in the ORBIT II trial were compared with those undergoing conventional PCI in the Assessment of Dual Antiplatelet Therapy with Drug Eluting Stents(ADAPT-DES) trial. Orbital atherectomy was projected to save an additional 0.41 life-years compared with conventional PCI. Such benefit was more pronounced when orbital atherectomy was used in the inpatient setting [70]. Adequate patient selection and the preintervention planned use of atherectomy may help to decrease the procedural time, amount of contrast, fluoroscopy time, and number of dilation balloons [71]. This is might also help to reduce in-hospital MACE and the incidence of procedural dissections. However, the long-term clinical benefits are yet unproven [72].
Future Considerations
The current direction is to make the atherectomy a safer procedure by the integration of intravascular imaging. This may help in adequate lesion selection and preparation as regards depth and length. It may also help in avoiding additional damage to areas with healthy intima and adventitia, and theoretically decrease the restenosis rates. It may also help in early visualization of complications such as coronary dissection and perforation. The Pantheris OCT-guided peripheral atherectomy device (Avinger Inc.) is approved by the FDA for peripheral vascular interventions. However, similar devices are still not available for coronary use.
Conclusions
Coronary atherectomy is a technically demanding procedure. Currently, the leading role of atherectomy is to facilitate a higher rate of procedural success in heavily calcified lesions to allow successful PCI. Further clinical trials are needed to establish any added efficacy in reducing long-term morbidity and/or mortality. However, atherectomy may still have a role in an era of increased intervention for calcified coronary lesions, particularly with advancements in the use of intravascular imaging techniques such as IVUS imaging and OCT.
Conflict of lnterest
David Anderson is a consultant for Biosense Webster. All other authors declare that they have no conflicts of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or notfor-profit sectors.
 Cardiovascular Innovations and Applications2018年3期
Cardiovascular Innovations and Applications2018年3期
- Cardiovascular Innovations and Applications的其它文章
- Cardiovascular Innovations and Applications
- The Contemporary Role of Femoral Artery Access
- Persisting Angina after Successful Surgical Removal of a Large Coronary Artery Aneurysm Attached to the Proximal Portion of the Left Circumflex Artery: Role of Coronary Artery Spasm
- Speckle Tracking Echocardiography ldentifies lmpaired Longitudinal Strain as a Common Deficit in Various Cardiac Diseases
- Bioresorbable Vascular Scaffold in the Midportion of the Left Anterior Descending Artery for Cardiac Allograft Vasculopathy in a Cardiac Transplant Patient
- The Use of Direct Oral Anticoagulants for Prevention of Stroke and Systemic Embolic Events in East Asian Patients with Nonvalvular Atrial Fibrillation
