Acupuncture for hyperlipidaemia in adults: A systematic review and meta-analysis
Yan-Hong Yu, Jing-He Chen, Qian-Chun Yang
1Second Clinical Medical College, Guangzhou University of Chinese Medicine, Guangzhou, China; Department of nephropathy medicine, Guangdong Provincial Hospital Of Chinese Medicine, Guangzhou, China.
2Second Outpatient Department, First Affiliated Hospital, Guangzhou University of Chinese Medicine, Guangzhou,China; Graduate School of Pharmaceutical Sciences, College of Pharmacy, Ewha Womans University, 52 Ewhayeodae-gil, Seodaemun-gu, Seoul, South Korea
Abstract Objective: To assess the efficacy and safety of acupuncture for hyperlipidemia in adults. Methods: We searched electronic databases, including PubMed, the Cochrane Central Register of Controlled Trials, EMBASE, CBM, CNKI,and VIP. All included studies were assessed in terms of quality and risk bias. The Review Manager 5.3.3 software was used for the data analyses, and the GRADE profiler software was applied to classify the systematic review results.Results: Seventeen studies were identified (n = 1,408). Acupuncture (electro-acupuncture or magnetic needle) was equally as effective as sham treatment (needle acupuncture) (relative risk [RR], 0.95; 95% confidence interval [CI],0.72-1.24). Acupuncture (needle acupuncture, electro-acupuncture, moxibustion, and acupoint catgut embedding) was as effective as statin therapy (RR 0.10; 95%CI, 0.97-1.24). Acupuncture was as effective as Chinese herbal preparations(electro-acupuncture and auricular acupoint) (RR, 0.97; 95%CI, 0.89-1.06). However, insufficient evidence was available to demonstrate whether acupressure was effective compared with acupuncture plus other treatments (RR, 1.04;95%CI, 0.87-1.25). Conclusion: Acupuncture may improve hyperlipidemia levels. However, additional large, properly randomized, placebo-controlled, double-blind studies are required.
Keywords: Acupuncture, Hyperlipidaemia, Randomized controlled trials, Systematic review
Background
An abnormally high blood lipid level is also known as hyperlipoproteinemia or hyperlipidemia and is characterized by elevations in total cholesterol (TC), low density lipoprotein cholesterol (LDL-C), and/or triglycerides (TG) and low levels of high-density lipoprotein cholesterol (HDL-C) [1]. Hyperlipidemia is not a disease but a metabolic derangement that is caused by abnormal lipid and lipoprotein metabolism. This disorder is characterized by abnormally high concentrations of lipids (fats) in the blood, which are correlated with the development of atherosclerosis, which is the underlying cause of coronary heart disease (CHD)and stroke [2]. Genome-wide association studies have identified several genetic loci that contribute to variations in plasma lipids, including HDL-C [3], and dietary factors influence plasma lipid levels (such as LDL-C) [4]. Large,prospective, global, epidemiological studies have reported that high LDL-C and low HDL-C are among the most important predictors of future cardiovascular events,including myocardial infarction, ischemic stroke, and death[5]. In 2006, the prevalence of less than optimal concentrations of lipids and lipoproteins was estimated to be 102.2 million for TC, 35.1 million for HDL-C, and 71.2 million for LDL-C. These rates include 46.8% of all American adults for TC, 16.2% for HDL-C, and 32.6%for LDL-C [6].
Elevated LDL-C is the primary treatment target for patients at risk of CHD [7]. Moreover, higher levels of HDL-C are associated with reduced plaque progression and reduced frequency of cardiovascular events [8].Current HDL-C-elevating drugs (fibrates and niacin) have limited efficacy and undesirable side effects [9].Atherogenic dyslipidemia increases the risk for CHD and peripheral vascular disease and remains a serious public health problem despite efforts to implement lifestyle modifications and pharmacological interventions using lipid modifying drugs [10]. Statins are the first-line medication widely prescribed to lower LDL-C levels and lower LDL particle numbers; however, their effect on HDL particles is modest [11]. Niacin is the most effective agent currently available for raising HDL cholesterol and shows a decrease in atherogenic particle numbers to a greater extent than that of atorvastatin monotherapy when used in combination with simvastatin [12]. HMG-CoA reductase inhibitors (statins) are the first-line therapy as an adjunct to therapeutic life changes [13]. Statins inhibit cholesterol synthesis in the liver and induce dose-dependent LDL-C reductions in the range of 20–60%, depending on the drug and dosage used [14].
The acupuncture technique most often studied scientifically involves penetrating the skin with thin, solid,metallic needles that are manipulated by the hands or by electrical stimulation. Acupuncture is one of the main modalities of traditional Chinese medicine (TCM) and has been practiced in China and other Asian countries for thousands of years. Acupuncture is a procedure in which specific body areas, the acupoints (also called meridian points), are pierced with fine needles for therapeutic purposes [15]. Acupuncture involves complex theories of the regulation of Yin and Yang forces such as Qi (air),blood, and body fluids. According to TCM, an imbalance in the Yin and Yang forces of the body or an excess or deficiency of Qi, blood, or body fluids are the main causes of pain and disease. Acupuncture treats illness by recreating the balance between the Yin and Yang forces and restores normal Qi, blood, and body fluids by stimulating different acupoints that govern different parts of the body and their interactions [16]. Various forms of acupuncture have been developed besides traditional needle acupuncture, including moxibustion,electro-acupuncture, magnetic needle, acupoint injection,auricular acupoint, and acupoint catgut embedding.
Acupuncture has been used clinically to treat high blood lipids in China for many years. However, its effects and safety have not been reviewed systematically.
Methods
Study criteria
Types of studies.Only randomized controlled trials(RCTs) were included.
Participants.Studies enrolled adult patients with high blood lipids who had TC levels > 5.72 mmol/L (220 mg/dL) or LDL-C levels > 3.60 mmol/L (160 mg/dL)and/or TG levels > 1.70 mmol/L (140 mg/dL), or HDL-C levels < 1.04 mmol/L (40 mg/dL). Patients with high blood lipids of any gender, ethnic group, and aged of 18-75 years were included. Studies were excluded if subjects had familial high blood lipids(hyperlipoproteinemia or hyperlipidemia), secondary high blood lipids (hyperlipoproteinemia or hyperlipidemia), or were treated with lipid lowering drugs during the 2 weeks before entering the study.
Interventions.Acupuncture aloneversusplacebo or sham treatment, acupunctureversusother treatments alone, and acupuncture plus other treatmentsversusother treatments alone. Other treatments included Chinese herbal preparations and Western medicine.
Outcome measures.Primary outcomes included mortality, total effective rate, and secondary outcomes included blood lipids levels (e.g., TC, TG, LDL-C, and HDL-C), adverse effects (e.g., myocardial infarction,angina pectoris, stroke (any stroke, hemorrhagic or non-hemorrhagic). TCM outcomes such as tongue coat and pulse condition, and economic index were included.
Search methods.We used PubMed (1966–May 2017),the Cochrane Central Register of Controlled Trials,EMBASE (1980–May 2017), the Chinese Biomedicine Database (1976–May 2017), CNKI (1979–May 2017),and VIP (1989–May 2017). All studies included were analyzed according to the Cochrane Handbook criteria.The following search terms were used: (Acupuncture OR electro-acupuncture OR electro-acupuncture OR acupoint OR acupoint injection OR acu-point OR acupressure OR moxibustion OR catgut embedding OR zhenjiu OR zhen jiu OR zhenci OR zhen ci OR cizhen OR dianzhen OR dian zhen OR zhen ya OR er zhen OR ti zhen OR she zhen OR tou pi zhen) AND (hypercholesterolemia OR hyperlipemia OR hyperlipidemia OR high blood lipids).
Data collection and analysis
Study selection.Titles and abstracts identified from the register were scrutinized by two reviewers. The full texts of all potentially relevant studies were obtained for review. An inclusion form was developed to assist in study selection. The reviewer decided which studies fit the inclusion criteria and graded their methodological quality. Disagreements regarding inclusion criteria were resolved by discussion between the reviewers.
Data extraction and management.Data were extracted independently by two authors. Data on patients, methods,interventions, outcomes, and results were extracted using a data extraction form. Differences were resolved by consensus and, when necessary, in consultation with a third reviewer. The authors of the studies were contacted to clarify the details when there was uncertainty.
Assessment of Risk of Bias in Included Studies.The following items were independently assessed by our authors using the risk of bias assessment tool. (1)Was there adequate sequence generation (selection bias)? (2)Was allocation adequately concealed (selection bias)? (3)Was knowledge of the allocated interventions adequately prevented during the study (e.g., participants and personnel, outcome assessors) (detection bias)? (4) Were incomplete outcome data adequately addressed (attrition bias)? (5) Are reports of the study free of suggesting selective outcome reporting (reportingbias)? (6)Was the study apparently free of other problems that could put it at risk for bias?
Data analyses.Data analyses were performed using the Cochrane Collaboration RevMan ver. 5.1.6 software.Results are expressed as relative risks (RR) and 95%confidence intervals (CIs) for dichotomous outcomes(e.g., mortality, effective rate, and adverse effects), and as mean difference (MD) with 95% CIs for continuous outcomes such as TC, TG, HDL-C, and LDL-C. We used fixed-effects and random-effects models for the analysis of the pooled data of the 17 studies.
Subgroup analyses.Subgroup analyses were carried out according to acupuncture therapy and comparators (e.g.,identical statin types).
Sensitivity analyses. Sensitivity analyses were conducted by excluding low-quality studies (based on the description of randomization, concealment of allocation,blinded assessment of outcomes, and description/analyses of withdrawals and dropouts) and a comparison of the results of the merger analysis of the fixed- and random-effects models.
Results
Search results
The initial search identified 779 potentially relevant articles. Of these, 73 were in the English database. A total of 298 articles were initially included after duplicate publications were excluded, and 23 articles were later excluded because they did not meet the inclusion criteria.Of the 275 potentially eligible reports, 258 were excluded for further assessment because telephone interviews with the original authors revealed that they were not RCTs.Therefore, 17 studies (1,408 participants) were included in this review. All were published in Chinese (Figure 1).
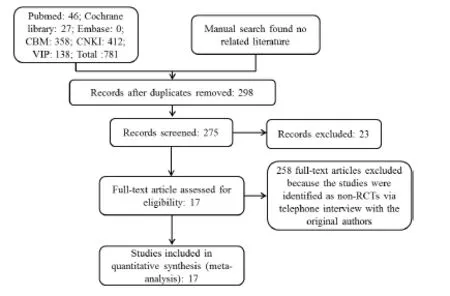
Figure 1 Study flow diagram
Studies included
The ratio of male to female participants in the 17 studies was 849/559 [17-18, 20-28, 30-33]. Two studies [19, 28]did not report the number of males and females. In total,1,408 adults were included in the 17 studies, all from China [17–33]. Patient ages ranged from 18–75 years.The average population size of the trials was 82.8 subjects (range, 50–204 participants).
The diagnostic criteria for high blood lipids in all studies included TC ≥ 5.72 mmol/L (220 mg/dL), LDL-C≥ 3.60 mmol/L (160 mg/dL), TG ≥ 1.70 mmol/L (140 mg/dL), or HDL-C ≤ 1.04 mmol/L (40 mg/dL). Fifteen studies [17–19, 21-26, 28-33] reported the total effective rate; 14 studies [17-24, 27-29, 31-33] reported blood lipid levels (e.g., TC, TG, HDL-C, and LDL-C). Two studies[25, 30] reported blood lipid levels (e.g., TC, TG, and LDL-C); One study [26] reported blood lipid levels (e.g.,TC, TG, and HDL-C).
Acupuncture interventions were administered as needle acupuncture, moxibustion, electro-acupuncture, magnetic needle, acupoint injection, auricular acupoint, and acupoint catgut embedding. The longest therapy duration was 6 weeks, and the shortest was 2 weeks. The follow-up duration in two studies [19, 30] was 2 months,and in one study [29] the follow-up duration was 1 month.In 14 studies [17-18, 20-28, 31-33], the follow-up duration was not stated. Two studies [22, 26] compared acupunctureversussham acupuncture, eight [17, 19, 21,18, 23, 24, 30, 32] compared acupunctureversusstatins,four [20, 25, 27, 28] compared acupunctureversusChinese herbal preparations, and three [33, 31, 29]compared acupuncture plus other treatmentsversusother treatments. The study descriptions are shown in Table 1.
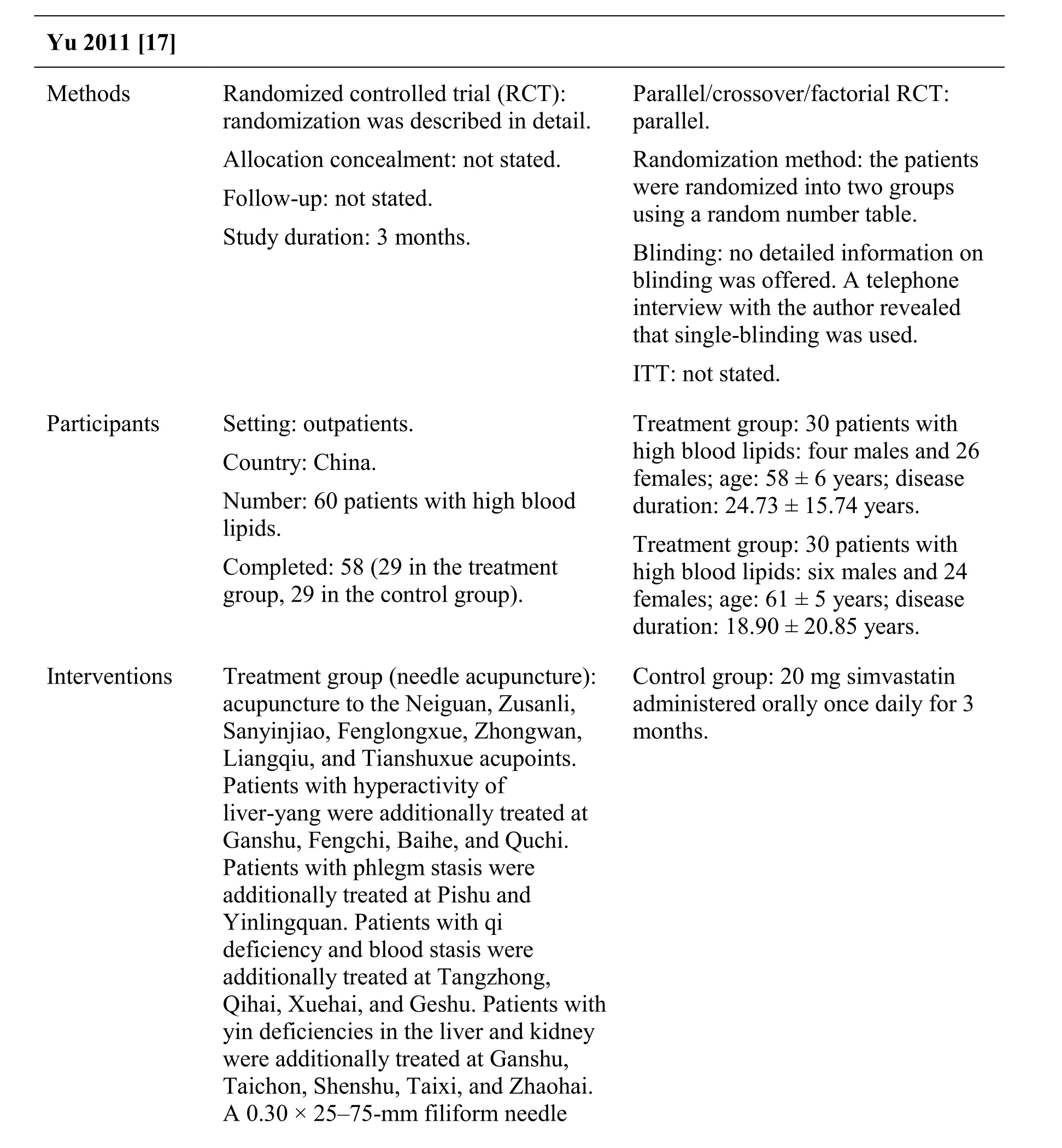
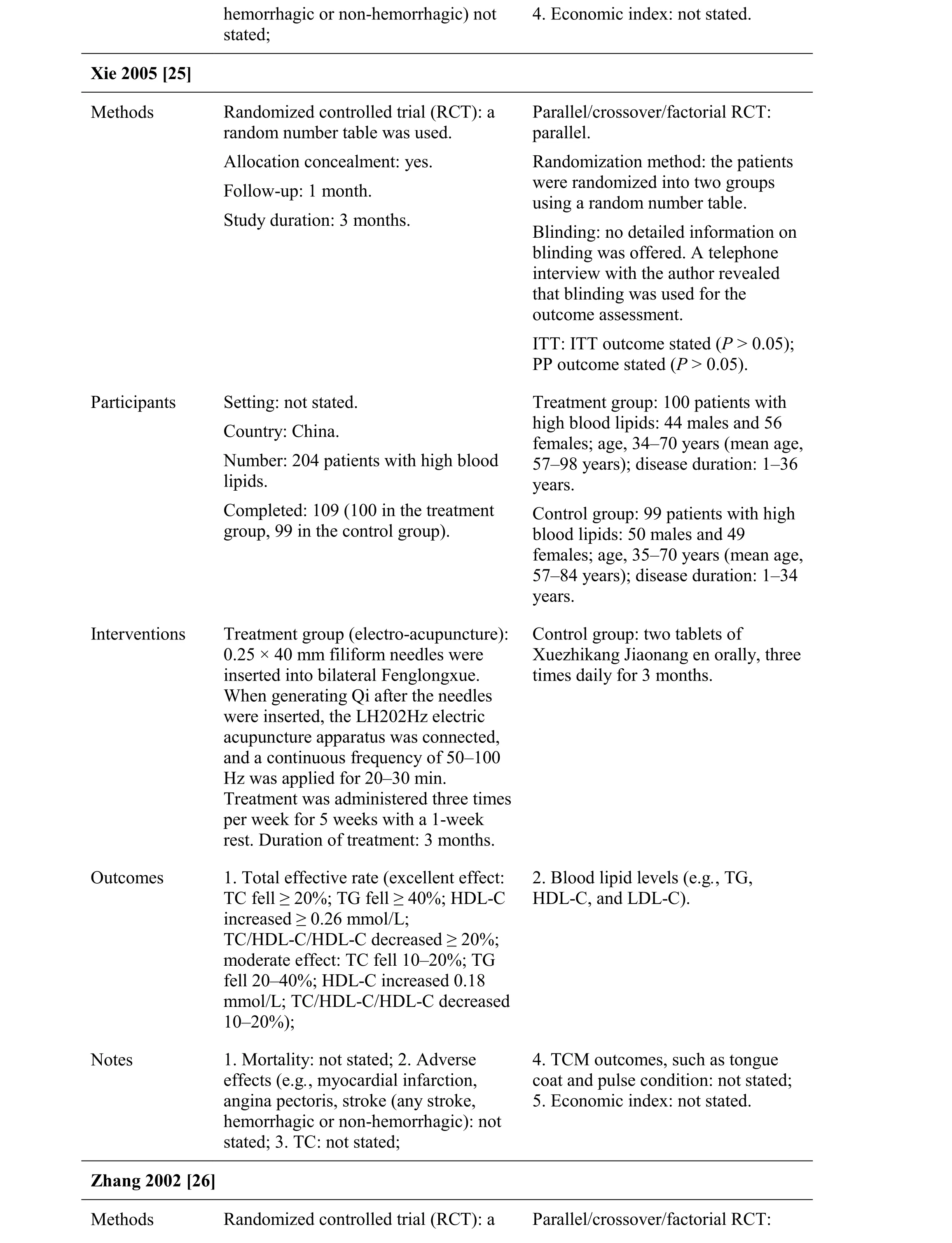
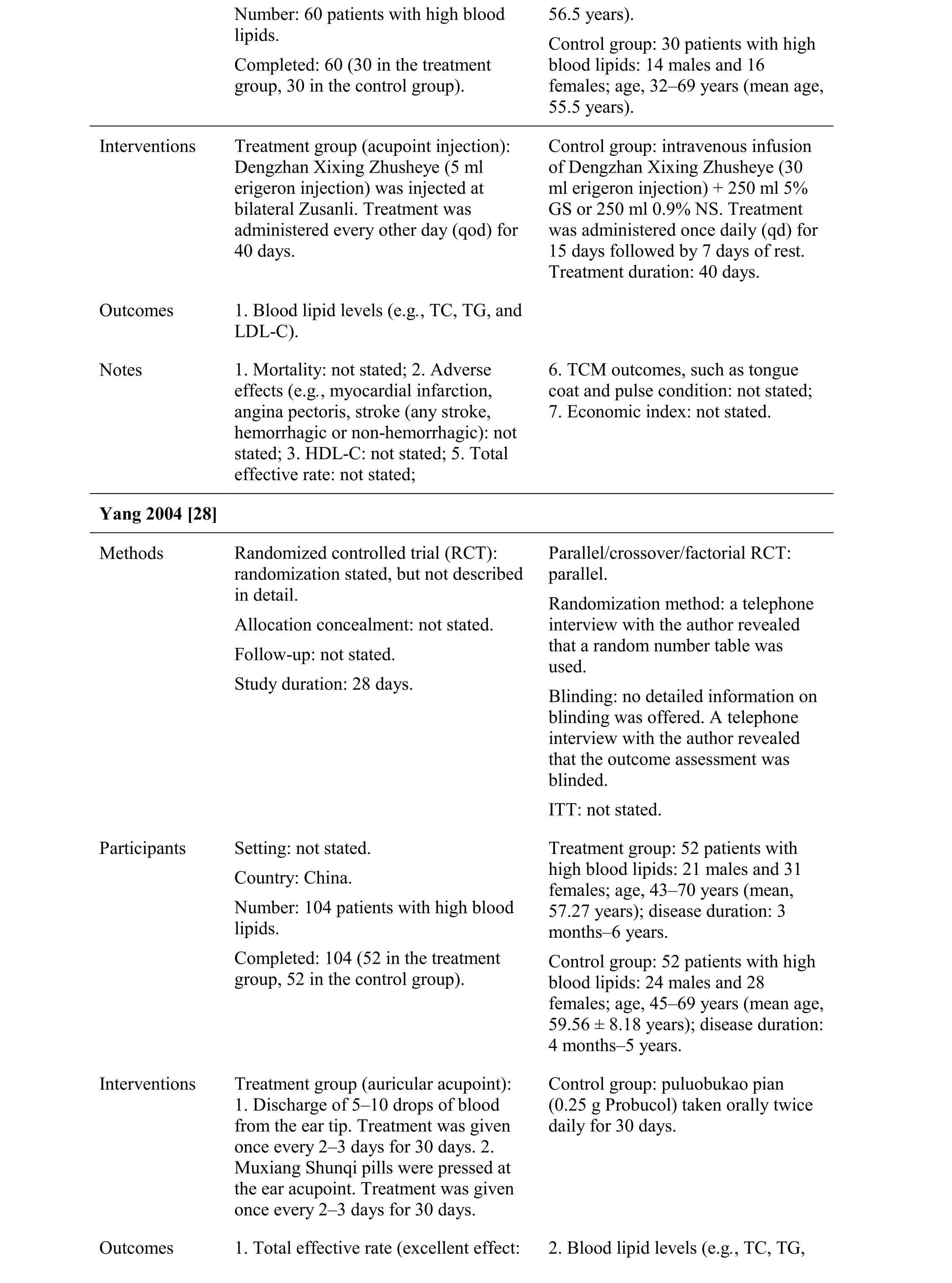
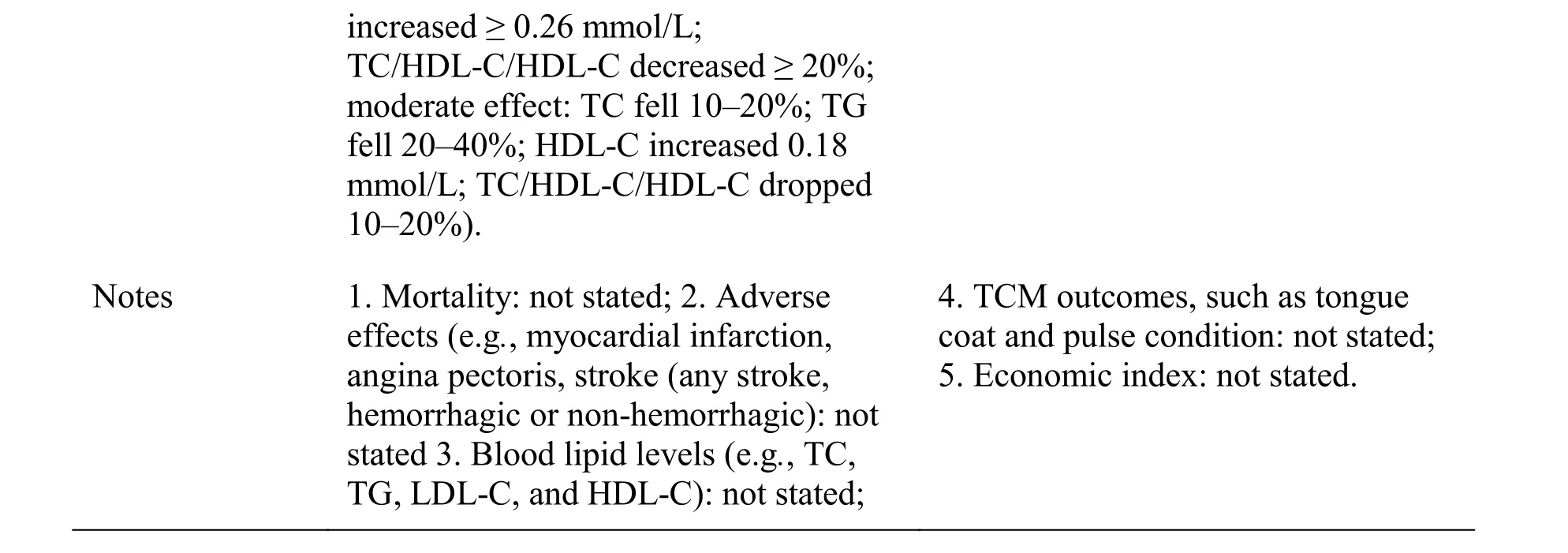
Table 1 Characteristics of the studies.
was inserted into the acupoints with a uniform reinforcing-reducing maneuver. The needles were left in place for 20 min. Treatment was administered once daily for 10 days followed by a 1-week rest. Duration of treatment: 3 months.Outcomes 1. Total effective rate (excellent effect:LDL-C dropped to the normal range;moderate effect: LDL-C fell 30%);2. Blood lipid levels (e.g., TC, TG,LDL-C, and HDL-C).Notes 1. Mortality, not stated; 2. Adverse effects (e.g., myocardial infarction,angina pectoris, stroke (any stroke,hemorrhagic or non-hemorrhagic): not stated;3. Traditional Chinese medicine(TCM) outcomes, such as tongue coat and pulse condition: not stated;4. Economic index: not stated.Wei 2009 [18]Methods Randomized controlled trial (RCT):randomization stated, but not described in detail.Allocation concealment: not stated.Follow-up: not stated.Study duration: 1 month.Parallel/crossover/factorial RCT:parallel.Randomization method: a telephone interview with the author revealed that a random number table was used.Blinding: no detailed information on blinding was offered. A telephone interview with the author revealed that single-blinding was used.ITT: not stated.Participants Setting: inpatients and outpatients.Country: China.Number: 66 patients with high blood lipids.Completed: 66 (34 in the treatment group, 32 in the control group).Treatment group: 34 patients with high blood lipids: 20 males and 14 females; mean age, 61 years; disease duration: not stated.Control group: 32 patients with high blood lipids: 18 males and 14 females; mean age, 61 years; disease duration: not stated.Interventions Treatment group (moxibustion):moxibustion with Hua Tuo brand treated at the Fenglong and Zusanli acupoints at 10 cm distance. The moxibustion was left in place for 5 min.Treatment was administered once daily for 1 month.Control group: 10 mg pravastatin taken orally once daily for 1 month.Outcomes 1. Total effective rate (excellent effect:TC fell ≥ 20%; TG fell ≥ 40%; HDL-C increased ≥ 0.26 mmol/L;TC/HDL-C/HDL-C dropped ≥ 20%;moderate effect: TC fell 10– 20%; TG fell 20–40%; HDL-C increased 0.18 mmol/L; TC/HDL-C/HDL-C dropped 10–20%);2. Blood lipid levels (e.g., TC, TG,LDL-C, and HDL-C).
Notes 1. Mortality: not stated; 2. Adverse effects (e.g., myocardial infarction,angina pectoris, stroke (any stroke,hemorrhagic or non-hemorrhagic): not stated;3. TCM outcomes, such as tongue coat and pulse condition: not stated;4. Economic index: not stated.Li 2008 [19]Methods Randomized controlled trial (RCT):randomization was described in detail.Allocation concealment: not stated.Follow-up: 2 months.Study duration: 1 month.Parallel/crossover/factorial RCT:parallel.Randomization method: the patients were randomized into two groups using a random number table.Blinding: no detailed information on blinding was offered. A telephone interview with the author revealed that single-blinding was used.ITT: not stated.Participants Setting: inpatients and outpatients Country: China.Number: 62 patients with high blood lipids.Completed: 62 (32 in the treatment group, 30 in the control group).Treatment group: 32 patients with high blood lipids, but gender, age,and course not stated.Control group: 32 patients with high blood lipids, but gender, age, and course not stated.Interventions Treatment group (laser needle acupuncture): helium-neon laser needles of 0.4 × 25–50 mm treated at the Zusanli and Fenglongxue acupoints.The Helium-neon laser needles were left in place for 15–20 min. Treatment was administered once daily for 7 days with a 3-day rest. Treatment duration:28 days.Control group: 10 mg simvastatin taken orally once daily for 28 days.Outcomes 1. Total effective rate (excellent effect:TC fell ≥ 20%; TG fell ≥ 40%; HDL-C increased ≥ 0.26 mmol/L;TC/HDL-C/HDL-C dropped ≥ 20%;moderate effect: TC fell 10–20%; TG fell 20–40%; HDL-C increased 0.18 mmol/L; TC/HDL-C/HDL-C dropped 10–20%);2. Blood lipid levels (e.g., TC, TG,LDL-C, and HDL-C).Notes 1. Mortality: not stated; 2. Adverse effects (e.g., myocardial infarction,angina pectoris, stroke (any stroke,hemorrhagic or non-hemorrhagic): not stated;3. TCM outcomes, such as tongue coat and pulse condition: not stated;4. Economic index: not stated.Huang 2003 [20]Methods Randomized controlled trial (RCT):randomization stated, but not described in detail.Allocation concealment: not stated.Parallel/crossover/factorial RCT:parallel.Randomization method: a telephone interview with the author revealed that a random number table was
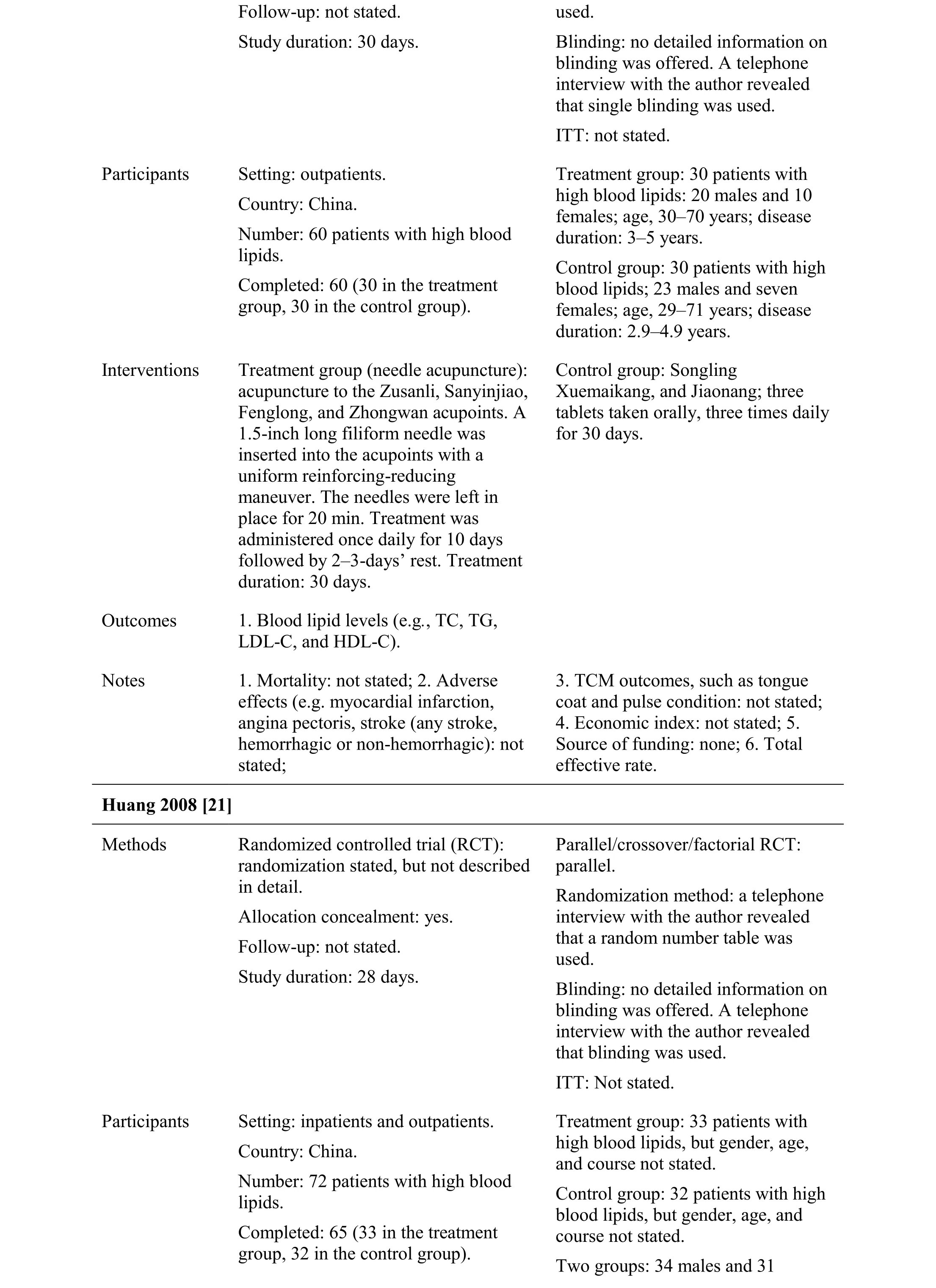
Number: 60 patients with high blood lipids.Completed: 60 (30 in the treatment group, 30 in the control group).duration: 3–5 years.Control group: 30 patients with high blood lipids; 23 males and seven females; age, 29–71 years; disease duration: 2.9–4.9 years.Interventions Treatment group (needle acupuncture):acupuncture to the Zusanli, Sanyinjiao,Fenglong, and Zhongwan acupoints. A 1.5-inch long filiform needle was inserted into the acupoints with a uniform reinforcing-reducing maneuver. The needles were left in place for 20 min. Treatment was administered once daily for 10 days followed by 2–3-days’ rest. Treatment duration: 30 days.Control group: Songling Xuemaikang, and Jiaonang; three tablets taken orally, three times daily for 30 days.Outcomes 1. Blood lipid levels (e.g., TC, TG,LDL-C, and HDL-C).Notes 1. Mortality: not stated; 2. Adverse effects (e.g. myocardial infarction,angina pectoris, stroke (any stroke,hemorrhagic or non-hemorrhagic): not stated;3. TCM outcomes, such as tongue coat and pulse condition: not stated;4. Economic index: not stated; 5.Source of funding: none; 6. Total effective rate.Huang 2008 [21]Methods Randomized controlled trial (RCT):randomization stated, but not described in detail.Allocation concealment: yes.Follow-up: not stated.Study duration: 28 days.Parallel/crossover/factorial RCT:parallel.Randomization method: a telephone interview with the author revealed that a random number table was used.Blinding: no detailed information on blinding was offered. A telephone interview with the author revealed that blinding was used.ITT: Not stated.Participants Setting: inpatients and outpatients.Country: China.Number: 72 patients with high blood lipids.Completed: 65 (33 in the treatment group, 32 in the control group).Treatment group: 33 patients with high blood lipids, but gender, age,and course not stated.Control group: 32 patients with high blood lipids, but gender, age, and course not stated.Two groups: 34 males and 31
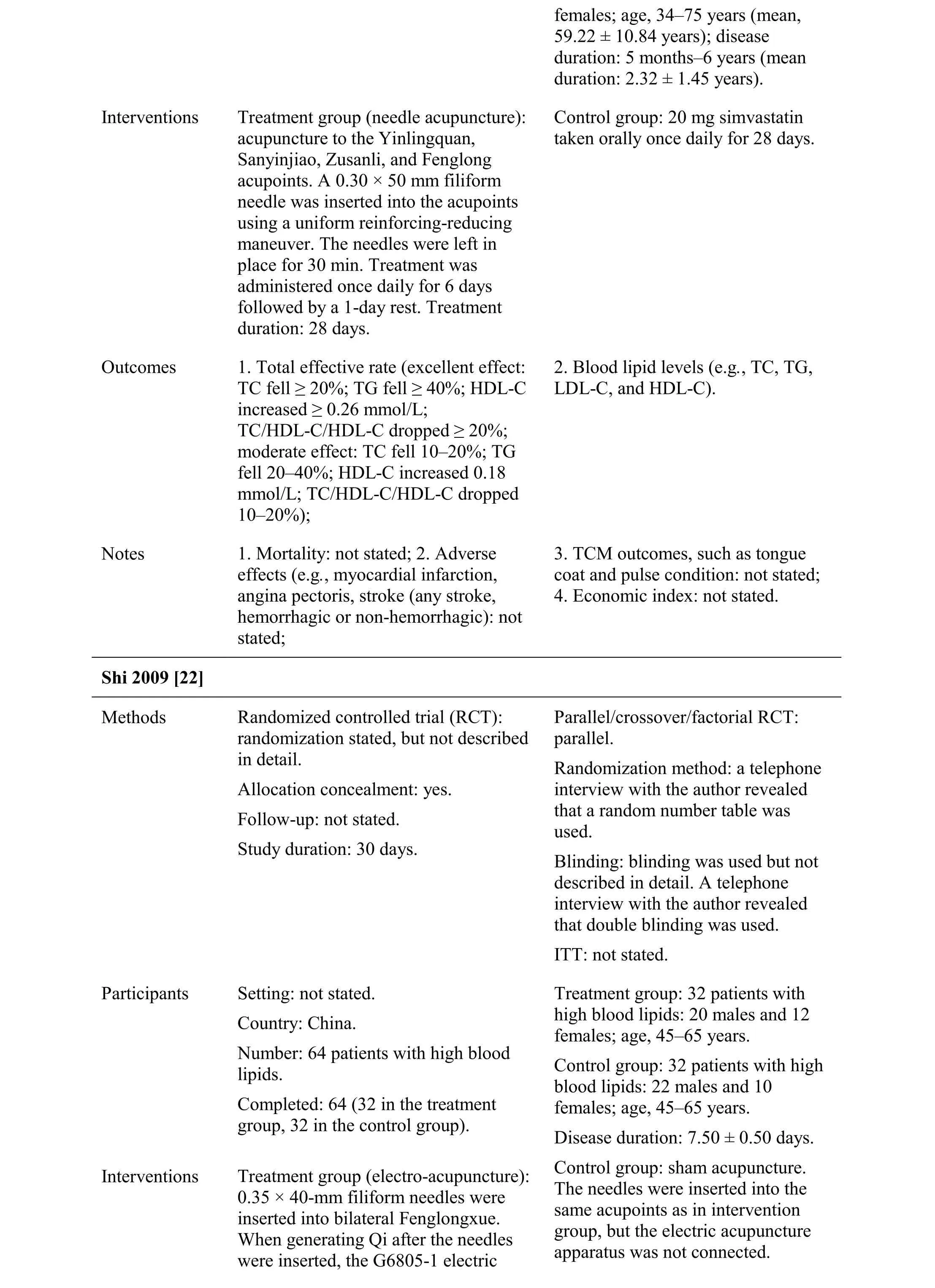
females; age, 34–75 years (mean,59.22 ± 10.84 years); disease duration: 5 months–6 years (mean duration: 2.32 ± 1.45 years).Interventions Treatment group (needle acupuncture):acupuncture to the Yinlingquan,Sanyinjiao, Zusanli, and Fenglong acupoints. A 0.30 × 50 mm filiform needle was inserted into the acupoints using a uniform reinforcing-reducing maneuver. The needles were left in place for 30 min. Treatment was administered once daily for 6 days followed by a 1-day rest. Treatment duration: 28 days.Control group: 20 mg simvastatin taken orally once daily for 28 days.Outcomes 1. Total effective rate (excellent effect:TC fell ≥ 20%; TG fell ≥ 40%; HDL-C increased ≥ 0.26 mmol/L;TC/HDL-C/HDL-C dropped ≥ 20%;moderate effect: TC fell 10–20%; TG fell 20–40%; HDL-C increased 0.18 mmol/L; TC/HDL-C/HDL-C dropped 10–20%);2. Blood lipid levels (e.g., TC, TG,LDL-C, and HDL-C).Notes 1. Mortality: not stated; 2. Adverse effects (e.g., myocardial infarction,angina pectoris, stroke (any stroke,hemorrhagic or non-hemorrhagic): not stated;3. TCM outcomes, such as tongue coat and pulse condition: not stated;4. Economic index: not stated.Shi 2009 [22]Methods Randomized controlled trial (RCT):randomization stated, but not described in detail.Allocation concealment: yes.Follow-up: not stated.Study duration: 30 days.Parallel/crossover/factorial RCT:parallel.Randomization method: a telephone interview with the author revealed that a random number table was used.Blinding: blinding was used but not described in detail. A telephone interview with the author revealed that double blinding was used.ITT: not stated.Participants Setting: not stated.Country: China.Number: 64 patients with high blood lipids.Completed: 64 (32 in the treatment group, 32 in the control group).Treatment group: 32 patients with high blood lipids: 20 males and 12 females; age, 45–65 years.Control group: 32 patients with high blood lipids: 22 males and 10 females; age, 45–65 years.Disease duration: 7.50 ± 0.50 days.Interventions Treatment group (electro-acupuncture):0.35 × 40-mm filiform needles were inserted into bilateral Fenglongxue.When generating Qi after the needles were inserted, the G6805-1 electric Control group: sham acupuncture.The needles were inserted into the same acupoints as in intervention group, but the electric acupuncture apparatus was not connected.
acupuncture apparatus was connected and a continuous 4-Hz wave was applied for 30 min. Treatment was administered once daily for 30 days.Outcomes 1. Total effective rate (excellent effect:TC fell ≥ 20%; TG fell ≥ 40%; HDL-C increased ≥ 0.26 mmol/L;TC/HDL-C/HDL-C dropped ≥ 20%;moderate effect: TC fell 10–20%; TG fell 20–40%; HDL-C increased 0.18 mmol/L; TC/HDL-C/HDL-C dropped 10–20%);2. Blood lipid levels (e.g., TC, TG,LDL-C, and HDL-C).Notes 1. Mortality: not stated; 2. Adverse effects (e.g., myocardial infarction,angina pectoris, stroke (any stroke,hemorrhagic or non-hemorrhagic): not stated;3. TCM outcomes, such as tongue coat and pulse condition: not stated;4. Economic index: not stated.Zhang 2007 [23]Methods Randomized controlled trial (RCT): a random number table was used.Allocation concealment: not stated.Follow-up: not stated.Study duration: 29 days.Parallel/crossover/factorial RCT:parallel.Randomization method: the patients were randomized into two groups using a random number table.Blinding: no detailed information on blinding was offered. A telephone interview with the author revealed that blinding was used during the outcome assessment.ITT: not stated.Participants Setting: not stated.Country: China.Number: 60 patients with high blood lipids.Completed: 60 (32 in the treatment group, 28 in the control group).Treatment group: 32 patients with high blood lipids, but gender, age,and course not stated.Control group: 28 patients with high blood lipids, but gender, age, and course not stated.Two groups: 27 males and 33 females; age, 43–75 years (mean age,66 years).Interventions Treatment group (electro-acupuncture):2-inch filiform needles were inserted into bilateral Fenglongxue. When generating Qi after the needles were inserted, the LH202H electric acupuncture apparatus was connected and a continuous frequency of 2/100Hz was applied for 30 min. Treatment was administered once daily for 5 days with 2 days of rest. Treatment duration: 29 days.Control group: 10 mg pravastatin taken orally once daily for 29 days.Outcomes 1. Total effective rate (excellent effect:TC fell ≥ 20%; TG fell ≥ 40%; HDL-C increased ≥ 0.26 mmol/L;2. Blood lipid levels (e.g., TC, TG,LDL-C, and HDL-C).
TC/HDL-C/HDL-C dropped ≥ 20%;moderate effect: TC fell 10–20%; TG fell 20–40%; HDL-C increased 0.18 mmol/L; TC/HDL-C/HDL-C dropped 10–20%);Notes 1. Mortality: not stated; 2. Adverse effects (e.g., myocardial infarction,angina pectoris, stroke (any stroke,hemorrhagic or non-hemorrhagic): not stated;3. TCM outcomes, such as tongue coat and pulse condition: not stated;4. Economic index: not stated.Zhang 2007 [24]Methods Randomized controlled trial (RCT):randomization stated, but not described in detail.Allocation concealment: not stated.Follow-up: not stated.Study duration: 29 days.Parallel/crossover/factorial RCT:parallel.Randomization method: a telephone interview with the author revealed that a random number table was used.Blinding: not detailed. No information on blinding was provided. A telephone interview with the author revealed that blinding was used during the outcome assessment.ITT: not stated.Participants Setting: not stated.Country: China.Number: 50 patients with high blood lipids.Completed: 50 (25 in the treatment group, 25 in the control group).Treatment group: 25 patients with high blood lipids: 13 males and 12 females; age, 43–75 years (mean age,61 years).Control group: 25 patients with high blood lipids: 12 males and 13 females; age, 26–75 years (mean age,66 years).Interventions Treatment group (electro-acupuncture):2 inch filiform needles were inserted into bilateral Fenglongxue. When generating Qi after the needles were inserted, the LH202Hz electric acupuncture apparatus was connected,and a continuous frequency of 2/100Hz was applied for 30 min. Treatment was administered once daily for 5 days with a 2-day rest. Treatment duration: 29 days.Control group: 10 mg pravastatin taken orally once daily for 29 days.Outcomes 1. Total effective rate (excellent effect:TC fell ≥ 20%; TG fell ≥ 40%; HDL-C increased ≥ 0.26 mmol/L;TC/HDL-C/HDL-C decreased ≥ 20%;moderate effect: TC fell 10–20%; TG fell 20–40%; HDL-C increased 0.18 mmol/L; TC/HDL-C/HDL-C decreased 10–20%);2. Blood lipid levels (e.g., TC, TG,LDL-C, and HDL-C).Notes 1. Mortality: not stated; 2. Adverse effects (e.g., myocardial infarction,angina pectoris, stroke (any stroke,3. TCM outcomes, such as tongue coat and pulse condition: not stated;
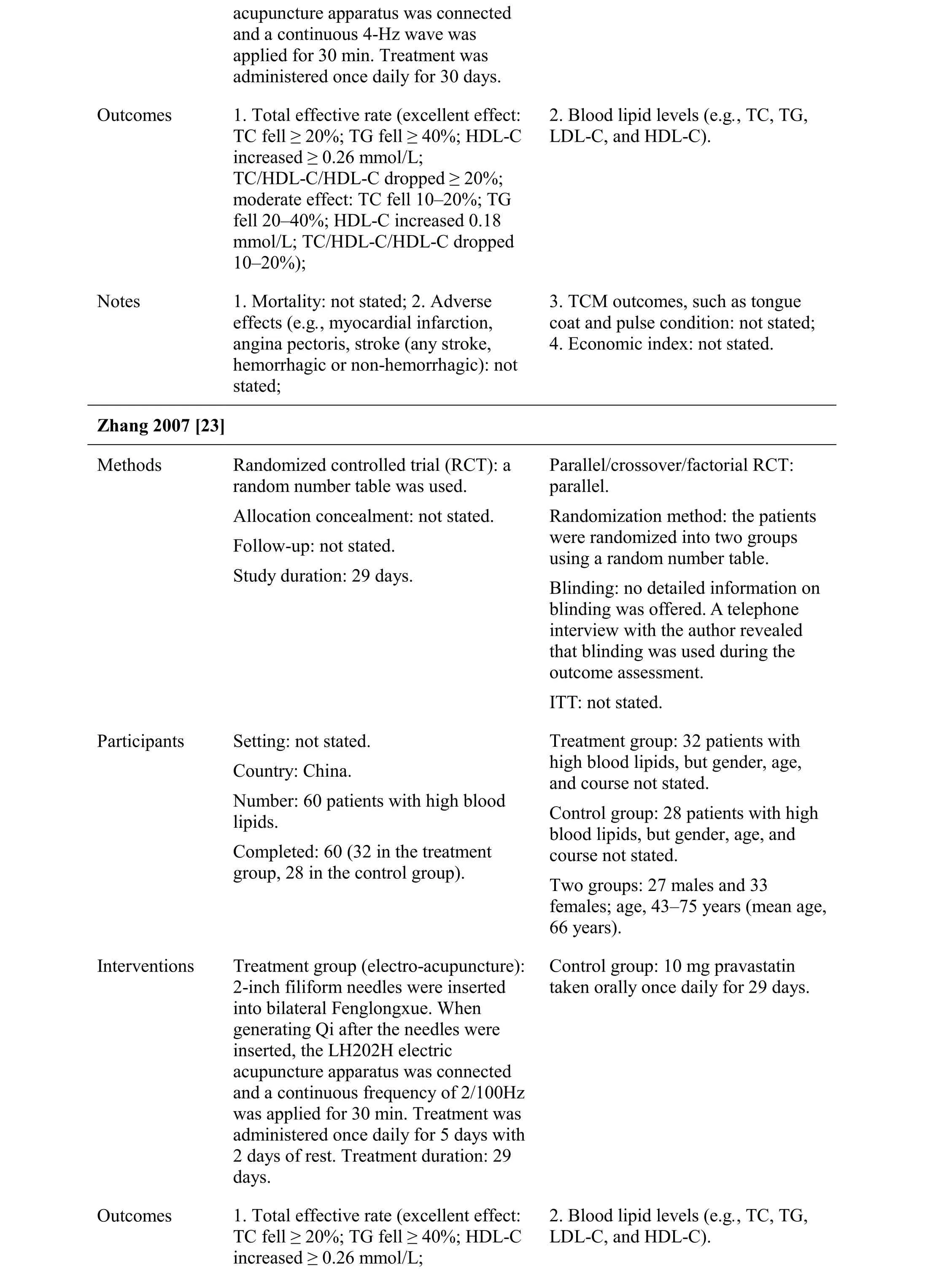
?
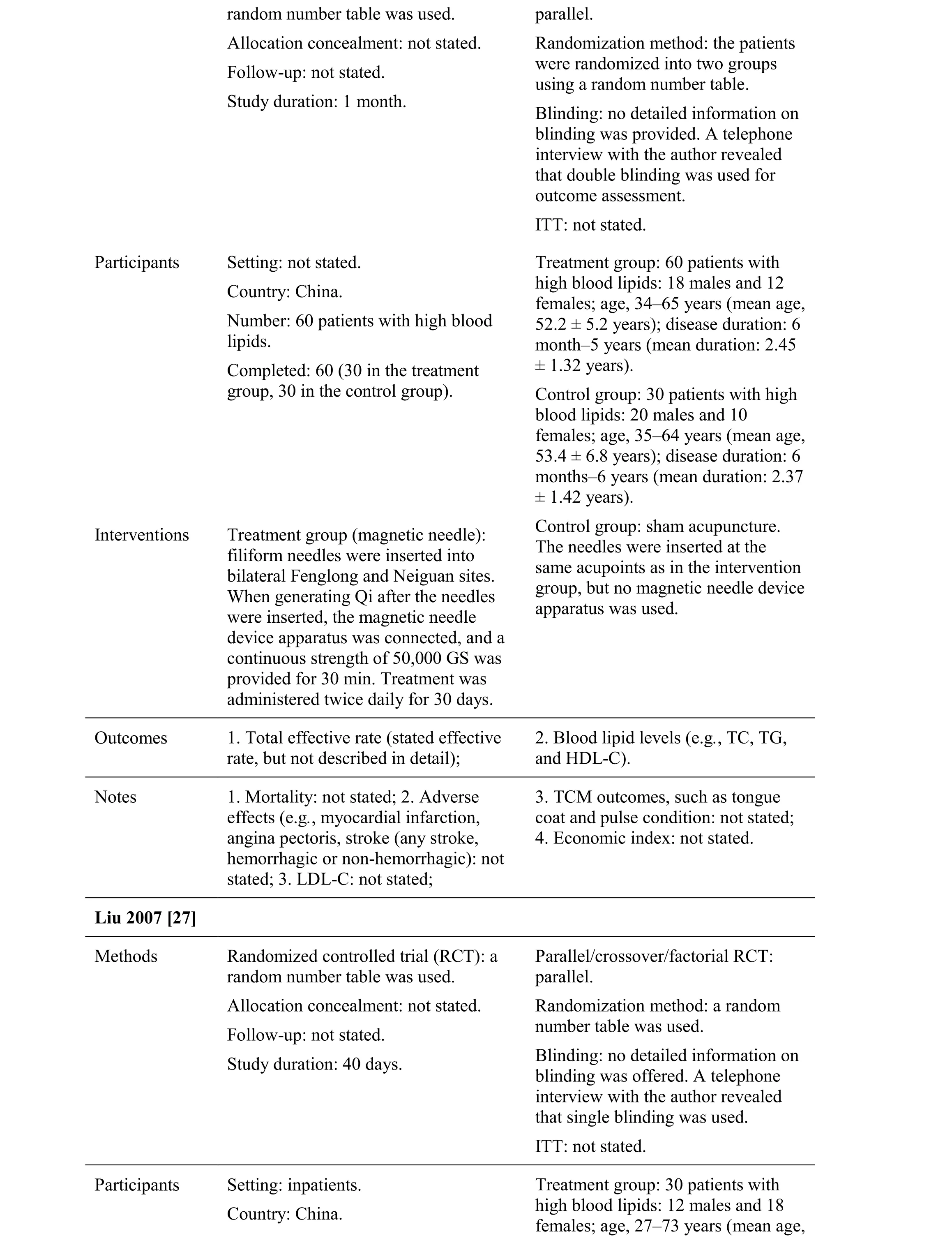
random number table was used.Allocation concealment: not stated.Follow-up: not stated.Study duration: 1 month.parallel.Randomization method: the patients were randomized into two groups using a random number table.Blinding: no detailed information on blinding was provided. A telephone interview with the author revealed that double blinding was used for outcome assessment.ITT: not stated.Participants Setting: not stated.Country: China.Number: 60 patients with high blood lipids.Completed: 60 (30 in the treatment group, 30 in the control group).Treatment group: 60 patients with high blood lipids: 18 males and 12 females; age, 34–65 years (mean age,52.2 ± 5.2 years); disease duration: 6 month–5 years (mean duration: 2.45± 1.32 years).Control group: 30 patients with high blood lipids: 20 males and 10 females; age, 35–64 years (mean age,53.4 ± 6.8 years); disease duration: 6 months–6 years (mean duration: 2.37± 1.42 years).Interventions Treatment group (magnetic needle):filiform needles were inserted into bilateral Fenglong and Neiguan sites.When generating Qi after the needles were inserted, the magnetic needle device apparatus was connected, and a continuous strength of 50,000 GS was provided for 30 min. Treatment was administered twice daily for 30 days.Control group: sham acupuncture.The needles were inserted at the same acupoints as in the intervention group, but no magnetic needle device apparatus was used.Outcomes 1. Total effective rate (stated effective rate, but not described in detail);2. Blood lipid levels (e.g., TC, TG,and HDL-C).Notes 1. Mortality: not stated; 2. Adverse effects (e.g., myocardial infarction,angina pectoris, stroke (any stroke,hemorrhagic or non-hemorrhagic): not stated; 3. LDL-C: not stated;3. TCM outcomes, such as tongue coat and pulse condition: not stated;4. Economic index: not stated.Liu 2007 [27]Methods Randomized controlled trial (RCT): a random number table was used.Allocation concealment: not stated.Follow-up: not stated.Study duration: 40 days.Parallel/crossover/factorial RCT:parallel.Randomization method: a random number table was used.Blinding: no detailed information on blinding was offered. A telephone interview with the author revealed that single blinding was used.ITT: not stated.Participants Setting: inpatients.Country: China.Treatment group: 30 patients with high blood lipids: 12 males and 18 females; age, 27–73 years (mean age,
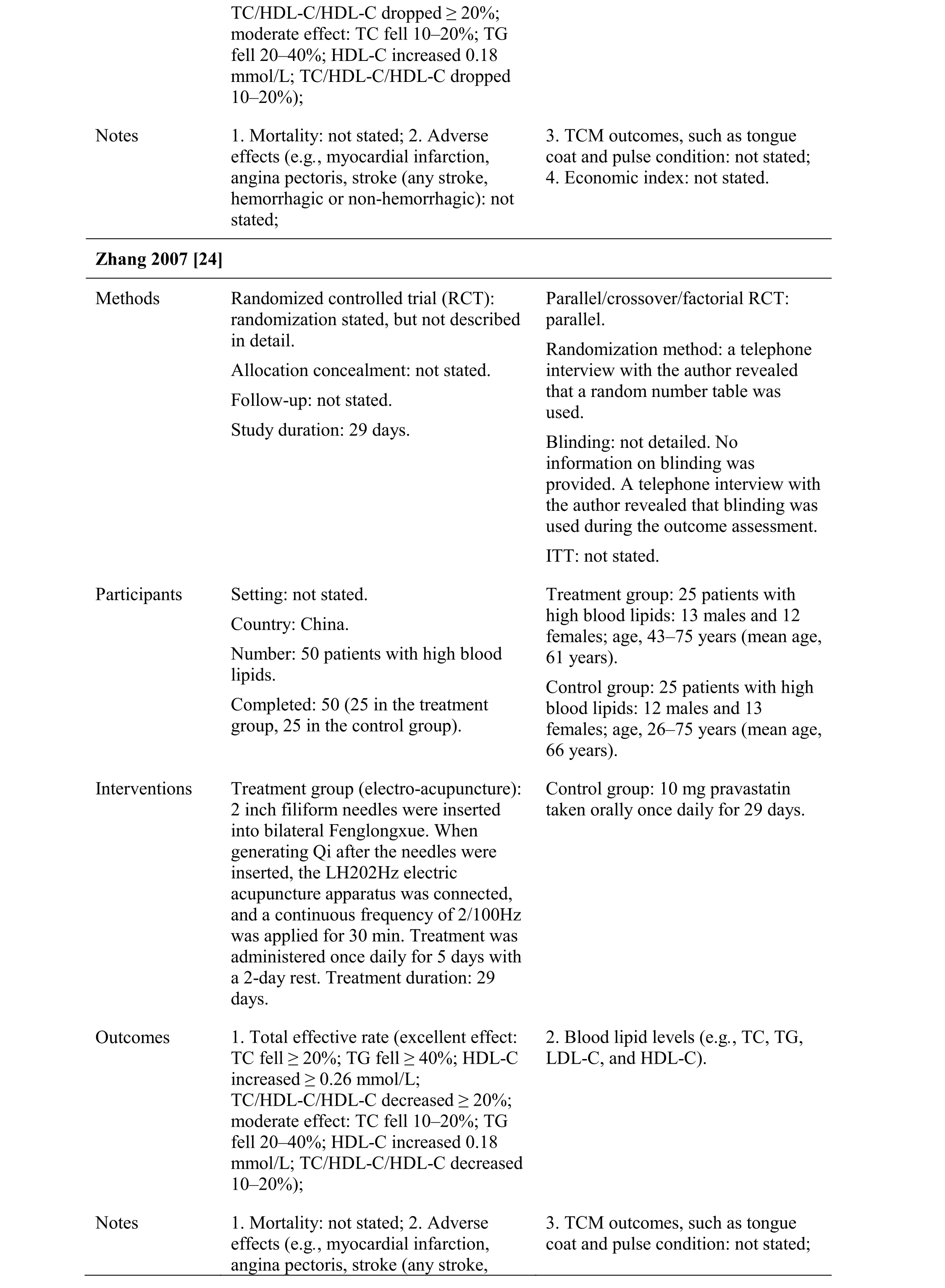
Number: 60 patients with high blood lipids.Completed: 60 (30 in the treatment group, 30 in the control group).56.5 years).Control group: 30 patients with high blood lipids: 14 males and 16 females; age, 32–69 years (mean age,55.5 years).Interventions Treatment group (acupoint injection):Dengzhan Xixing Zhusheye (5 ml erigeron injection) was injected at bilateral Zusanli. Treatment was administered every other day (qod) for 40 days.Control group: intravenous infusion of Dengzhan Xixing Zhusheye (30 ml erigeron injection) + 250 ml 5%GS or 250 ml 0.9% NS. Treatment was administered once daily (qd) for 15 days followed by 7 days of rest.Treatment duration: 40 days.Outcomes 1. Blood lipid levels (e.g., TC, TG, and LDL-C).Notes 1. Mortality: not stated; 2. Adverse effects (e.g., myocardial infarction,angina pectoris, stroke (any stroke,hemorrhagic or non-hemorrhagic): not stated; 3. HDL-C: not stated; 5. Total effective rate: not stated;6. TCM outcomes, such as tongue coat and pulse condition: not stated;7. Economic index: not stated.Yang 2004 [28]Methods Randomized controlled trial (RCT):randomization stated, but not described in detail.Allocation concealment: not stated.Follow-up: not stated.Study duration: 28 days.Parallel/crossover/factorial RCT:parallel.Randomization method: a telephone interview with the author revealed that a random number table was used.Blinding: no detailed information on blinding was offered. A telephone interview with the author revealed that the outcome assessment was blinded.ITT: not stated.Participants Setting: not stated.Country: China.Number: 104 patients with high blood lipids.Completed: 104 (52 in the treatment group, 52 in the control group).Treatment group: 52 patients with high blood lipids: 21 males and 31 females; age, 43–70 years (mean,57.27 years); disease duration: 3 months–6 years.Control group: 52 patients with high blood lipids: 24 males and 28 females; age, 45–69 years (mean age,59.56 ± 8.18 years); disease duration:4 months–5 years.Interventions Treatment group (auricular acupoint):1. Discharge of 5–10 drops of blood from the ear tip. Treatment was given once every 2–3 days for 30 days. 2.Muxiang Shunqi pills were pressed at the ear acupoint. Treatment was given once every 2–3 days for 30 days.Control group: puluobukao pian(0.25 g Probucol) taken orally twice daily for 30 days.Outcomes 1. Total effective rate (excellent effect: 2. Blood lipid levels (e.g., TC, TG,
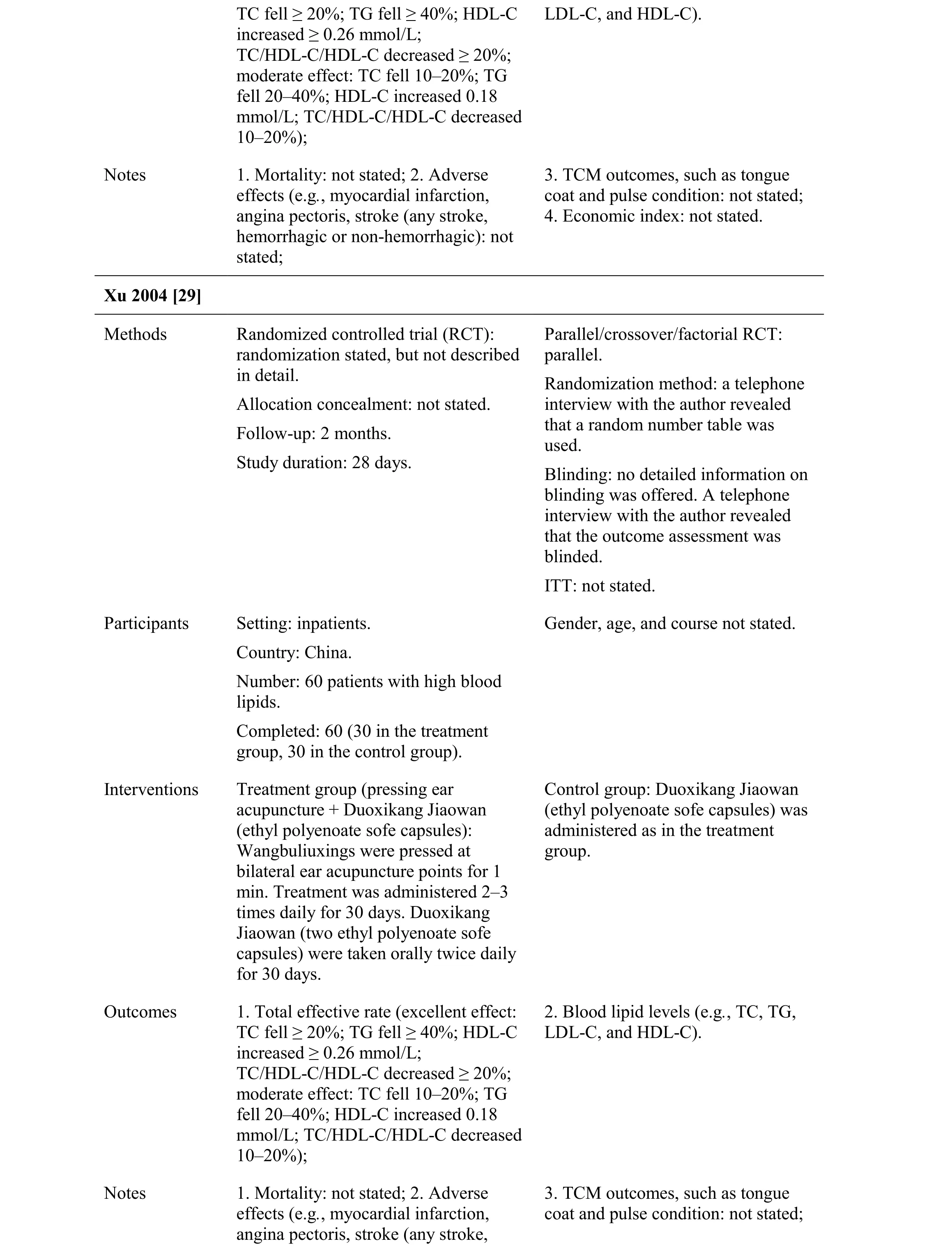
TC fell ≥ 20%; TG fell ≥ 40%; HDL-C increased ≥ 0.26 mmol/L;TC/HDL-C/HDL-C decreased ≥ 20%;moderate effect: TC fell 10–20%; TG fell 20–40%; HDL-C increased 0.18 mmol/L; TC/HDL-C/HDL-C decreased 10–20%);LDL-C, and HDL-C).Notes 1. Mortality: not stated; 2. Adverse effects (e.g., myocardial infarction,angina pectoris, stroke (any stroke,hemorrhagic or non-hemorrhagic): not stated;3. TCM outcomes, such as tongue coat and pulse condition: not stated;4. Economic index: not stated.Xu 2004 [29]Methods Randomized controlled trial (RCT):randomization stated, but not described in detail.Allocation concealment: not stated.Follow-up: 2 months.Study duration: 28 days.Parallel/crossover/factorial RCT:parallel.Randomization method: a telephone interview with the author revealed that a random number table was used.Blinding: no detailed information on blinding was offered. A telephone interview with the author revealed that the outcome assessment was blinded.ITT: not stated.Participants Setting: inpatients.Country: China.Number: 60 patients with high blood lipids.Completed: 60 (30 in the treatment group, 30 in the control group).Gender, age, and course not stated.Interventions Treatment group (pressing ear acupuncture + Duoxikang Jiaowan(ethyl polyenoate sofe capsules):Wangbuliuxings were pressed at bilateral ear acupuncture points for 1 min. Treatment was administered 2–3 times daily for 30 days. Duoxikang Jiaowan (two ethyl polyenoate sofe capsules) were taken orally twice daily for 30 days.Control group: Duoxikang Jiaowan(ethyl polyenoate sofe capsules) was administered as in the treatment group.Outcomes 1. Total effective rate (excellent effect:TC fell ≥ 20%; TG fell ≥ 40%; HDL-C increased ≥ 0.26 mmol/L;TC/HDL-C/HDL-C decreased ≥ 20%;moderate effect: TC fell 10–20%; TG fell 20–40%; HDL-C increased 0.18 mmol/L; TC/HDL-C/HDL-C decreased 10–20%);2. Blood lipid levels (e.g., TC, TG,LDL-C, and HDL-C).Notes 1. Mortality: not stated; 2. Adverse effects (e.g., myocardial infarction,angina pectoris, stroke (any stroke,3. TCM outcomes, such as tongue coat and pulse condition: not stated;
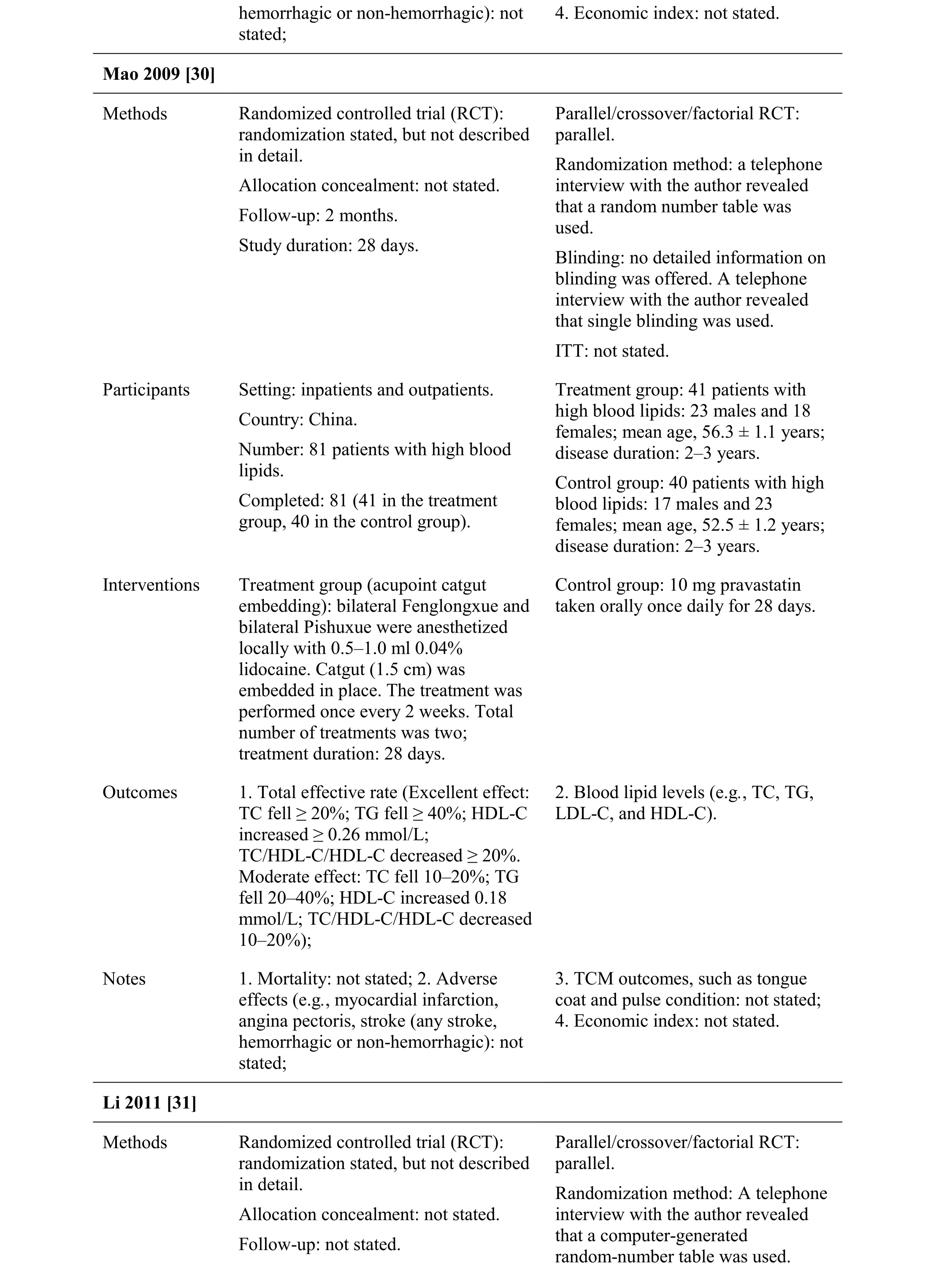
hemorrhagic or non-hemorrhagic): not stated;4. Economic index: not stated.Mao 2009 [30]Methods Randomized controlled trial (RCT):randomization stated, but not described in detail.Allocation concealment: not stated.Follow-up: 2 months.Study duration: 28 days.Parallel/crossover/factorial RCT:parallel.Randomization method: a telephone interview with the author revealed that a random number table was used.Blinding: no detailed information on blinding was offered. A telephone interview with the author revealed that single blinding was used.ITT: not stated.Participants Setting: inpatients and outpatients.Country: China.Number: 81 patients with high blood lipids.Completed: 81 (41 in the treatment group, 40 in the control group).Treatment group: 41 patients with high blood lipids: 23 males and 18 females; mean age, 56.3 ± 1.1 years;disease duration: 2–3 years.Control group: 40 patients with high blood lipids: 17 males and 23 females; mean age, 52.5 ± 1.2 years;disease duration: 2–3 years.Interventions Treatment group (acupoint catgut embedding): bilateral Fenglongxue and bilateral Pishuxue were anesthetized locally with 0.5–1.0 ml 0.04%lidocaine. Catgut (1.5 cm) was embedded in place. The treatment was performed once every 2 weeks. Total number of treatments was two;treatment duration: 28 days.Control group: 10 mg pravastatin taken orally once daily for 28 days.Outcomes 1. Total effective rate (Excellent effect:TC fell ≥ 20%; TG fell ≥ 40%; HDL-C increased ≥ 0.26 mmol/L;TC/HDL-C/HDL-C decreased ≥ 20%.Moderate effect: TC fell 10–20%; TG fell 20–40%; HDL-C increased 0.18 mmol/L; TC/HDL-C/HDL-C decreased 10–20%);2. Blood lipid levels (e.g., TC, TG,LDL-C, and HDL-C).Notes 1. Mortality: not stated; 2. Adverse effects (e.g., myocardial infarction,angina pectoris, stroke (any stroke,hemorrhagic or non-hemorrhagic): not stated;3. TCM outcomes, such as tongue coat and pulse condition: not stated;4. Economic index: not stated.Li 2011 [31]Methods Randomized controlled trial (RCT):randomization stated, but not described in detail.Allocation concealment: not stated.Follow-up: not stated.Parallel/crossover/factorial RCT:parallel.Randomization method: A telephone interview with the author revealed that a computer-generated random-number table was used.
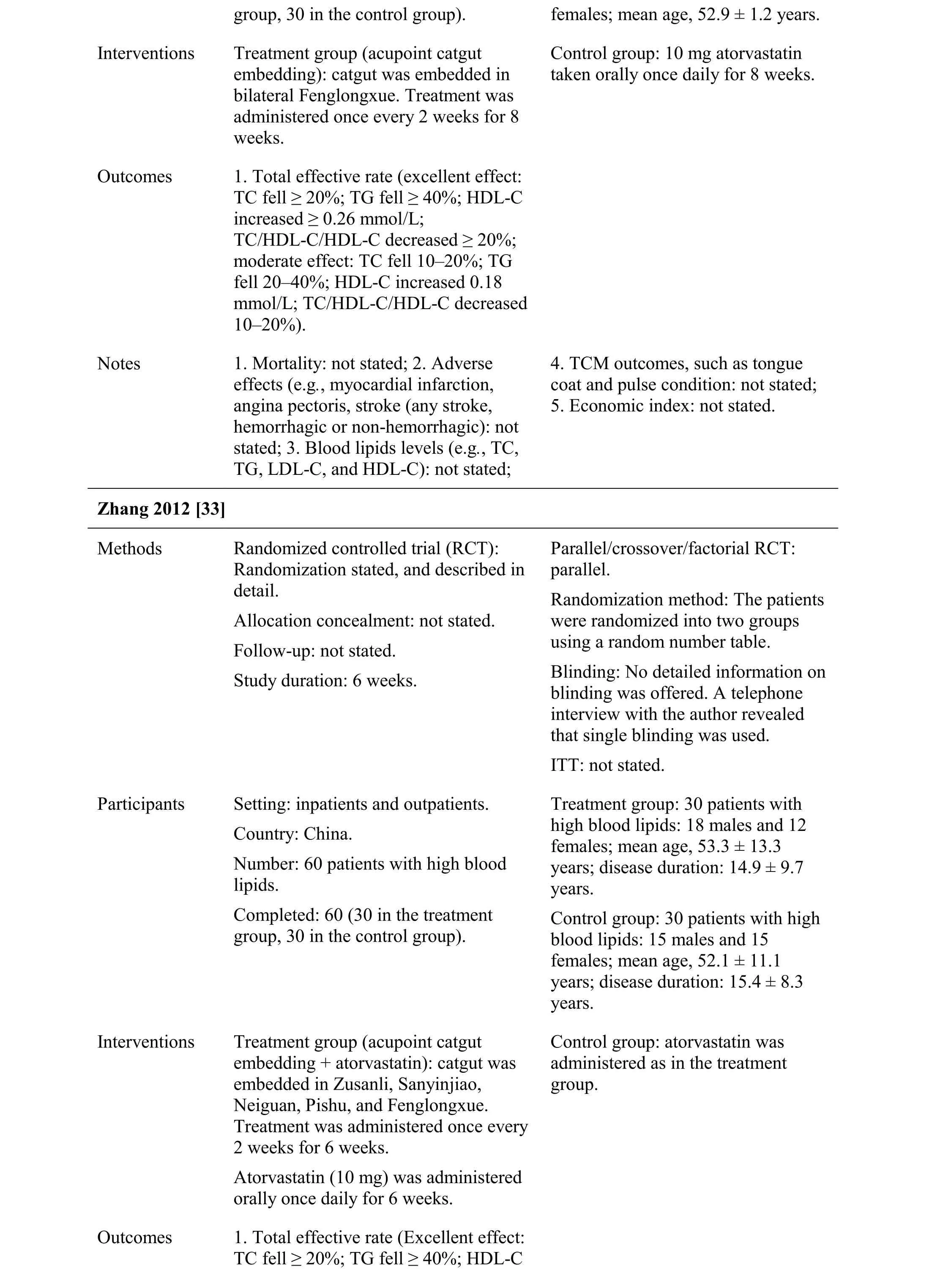
group, 30 in the control group). females; mean age, 52.9 ± 1.2 years.Interventions Treatment group (acupoint catgut embedding): catgut was embedded in bilateral Fenglongxue. Treatment was administered once every 2 weeks for 8 weeks.Control group: 10 mg atorvastatin taken orally once daily for 8 weeks.Outcomes 1. Total effective rate (excellent effect:TC fell ≥ 20%; TG fell ≥ 40%; HDL-C increased ≥ 0.26 mmol/L;TC/HDL-C/HDL-C decreased ≥ 20%;moderate effect: TC fell 10–20%; TG fell 20–40%; HDL-C increased 0.18 mmol/L; TC/HDL-C/HDL-C decreased 10–20%).Notes 1. Mortality: not stated; 2. Adverse effects (e.g., myocardial infarction,angina pectoris, stroke (any stroke,hemorrhagic or non-hemorrhagic): not stated; 3. Blood lipids levels (e.g., TC,TG, LDL-C, and HDL-C): not stated;4. TCM outcomes, such as tongue coat and pulse condition: not stated;5. Economic index: not stated.Zhang 2012 [33]Methods Randomized controlled trial (RCT):Randomization stated, and described in detail.Allocation concealment: not stated.Follow-up: not stated.Study duration: 6 weeks.Parallel/crossover/factorial RCT:parallel.Randomization method: The patients were randomized into two groups using a random number table.Blinding: No detailed information on blinding was offered. A telephone interview with the author revealed that single blinding was used.ITT: not stated.Participants Setting: inpatients and outpatients.Country: China.Number: 60 patients with high blood lipids.Completed: 60 (30 in the treatment group, 30 in the control group).Treatment group: 30 patients with high blood lipids: 18 males and 12 females; mean age, 53.3 ± 13.3 years; disease duration: 14.9 ± 9.7 years.Control group: 30 patients with high blood lipids: 15 males and 15 females; mean age, 52.1 ± 11.1 years; disease duration: 15.4 ± 8.3 years.Interventions Treatment group (acupoint catgut embedding + atorvastatin): catgut was embedded in Zusanli, Sanyinjiao,Neiguan, Pishu, and Fenglongxue.Treatment was administered once every 2 weeks for 6 weeks.Atorvastatin (10 mg) was administered orally once daily for 6 weeks.Control group: atorvastatin was administered as in the treatment group.Outcomes 1. Total effective rate (Excellent effect:TC fell ≥ 20%; TG fell ≥ 40%; HDL-C
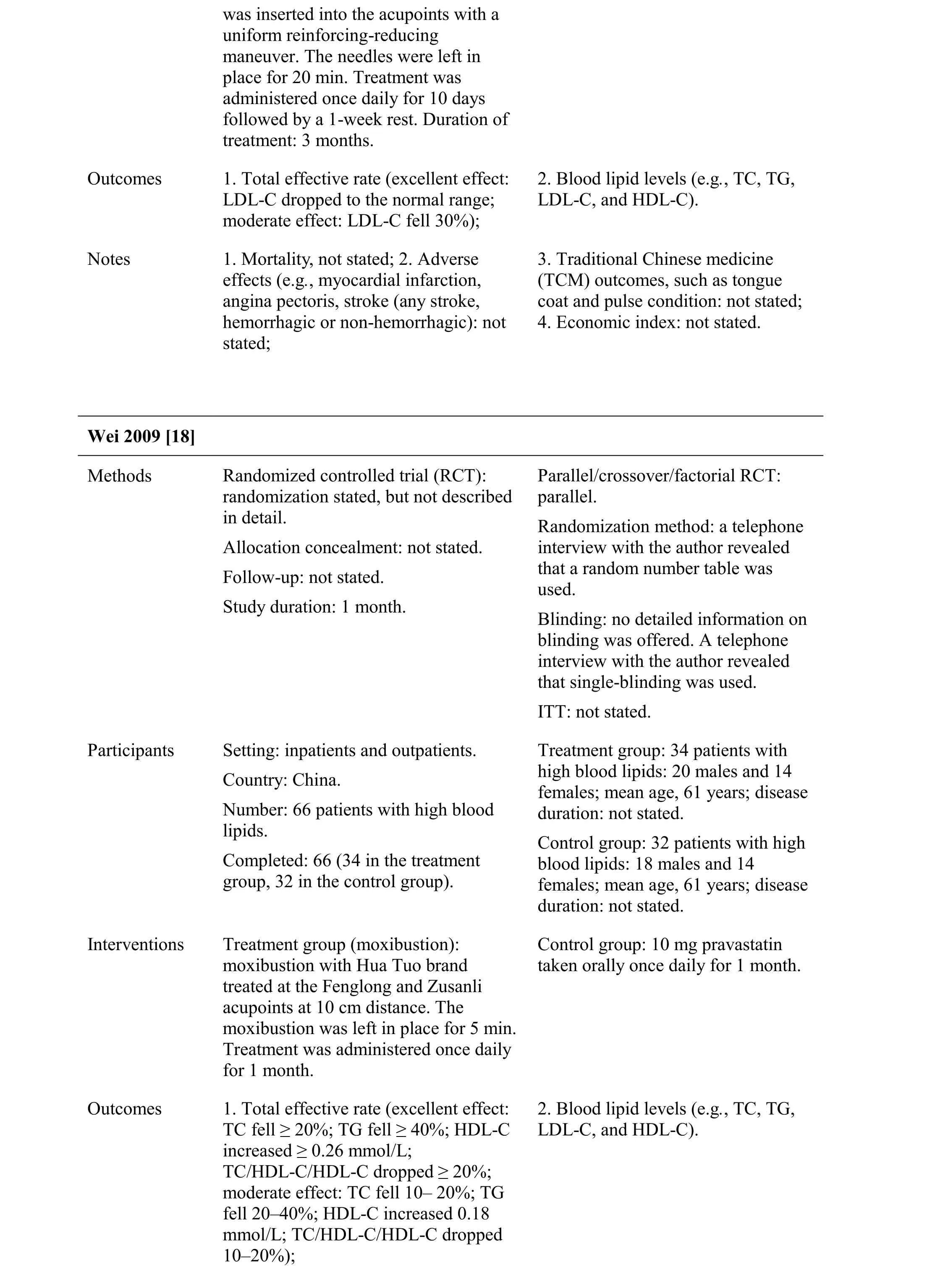
Risk of bias.The methodological quality of the randomization sequence, allocation concealment, blinding,incomplete outcome data, selective outcome reporting,and potential threats are summarized in Figure 2 and Figure 3.
?
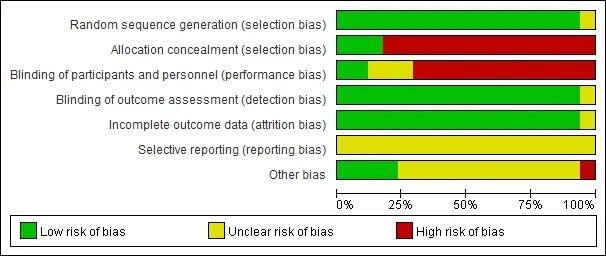
Figure 2 Methodological quality. Judgments regarding each item across all studies are presented as percentages
Randomization and allocation concealment.Fifteen studies [17-30, 33] used a random number table, two [31,32] used a computer-generated random-number table, and three used allocation concealment. Therefore, 14 studies had a high risk of selection bias.
Blinding.Two studies [22, 26] used double-blinding(outcome assessment, participants, or personnel), 15[17-21, 23-25, 27-33] used single-blinding (outcome assessment was blinded), which was determined by telephone interviews with the authors if the blinding methods were not described. Thus, these studies had a low risk of performance bias and low detection bias.
Flow of participants and intention-to-treat.Three studies [19, 25, 30] reported follow-up. In two [19, 30],the follow-up time was 2 months after treatment. One study [25] reported a follow-up time after the first month of treatment. Three studies [17, 21, 25] reported withdrawal or dropout. One study [17] reported dropout of two participants, but the proportion of drop-outs was <10%; thus, this was thought to represent a low risk of bias due to incomplete outcome data. One study [21] reported that seven participants dropped out, but that the proportion of drop-outs was < 10%; this was thought to represent a low risk of bias due to incomplete outcome data. One study [25] reported that five participants dropped out; however, the ITT wasP> 0.05.
Selective outcome reporting. No detailed evidence of selective reporting was detected in any of the 17 studies[17-33]. However, the risk of selective reporting bias was unclear because we were unable to compare the protocol with published reports.
Other potential sources of bias.Twelve studies [17-33]did not describe patient compliance. Three studies [19, 20,22] did not describe participant baseline demographic information. The appropriateness of the significance analyses used was assessed; all were considered appropriate. Although we conducted comprehensive searches and tried to avoid bias, we could not exclude potential publication bias because all 17 studies were published in China.
Effects of interventions.We collected data on the basis of acupuncture aloneversusplacebo or sham acupuncture.Acupuncture aloneversusstatins (e.g., simvastatin,pravastatin, or atorvastatin), acupuncture aloneversusChinese herbal preparations (e.g., Songling Xuemaikang Jiaonang, Xuezhikang Jiaonang, Dengzhan Xixing Zhusheye, and Puluobukao pian), acupuncture plus other therapyversusother therapy (e.g., Duoxikang Jiaowan,Xuemaikang Capsule, and atorvastatin). Acupuncture including needle acupuncture, moxibustion,electro-acupuncture, magnetic needle, acupoint injection,auricular acupoint, and acupoint catgut embedding were assessed.
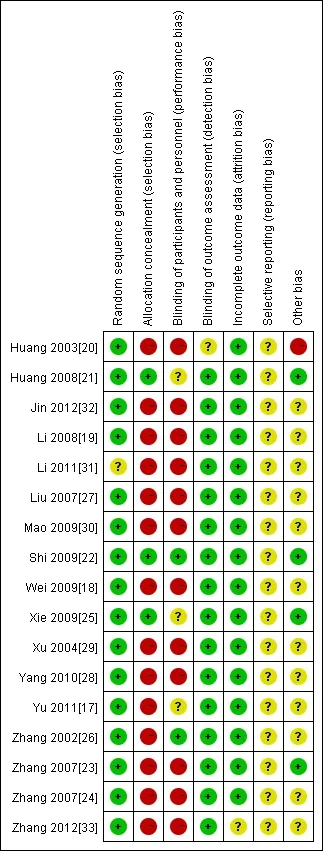
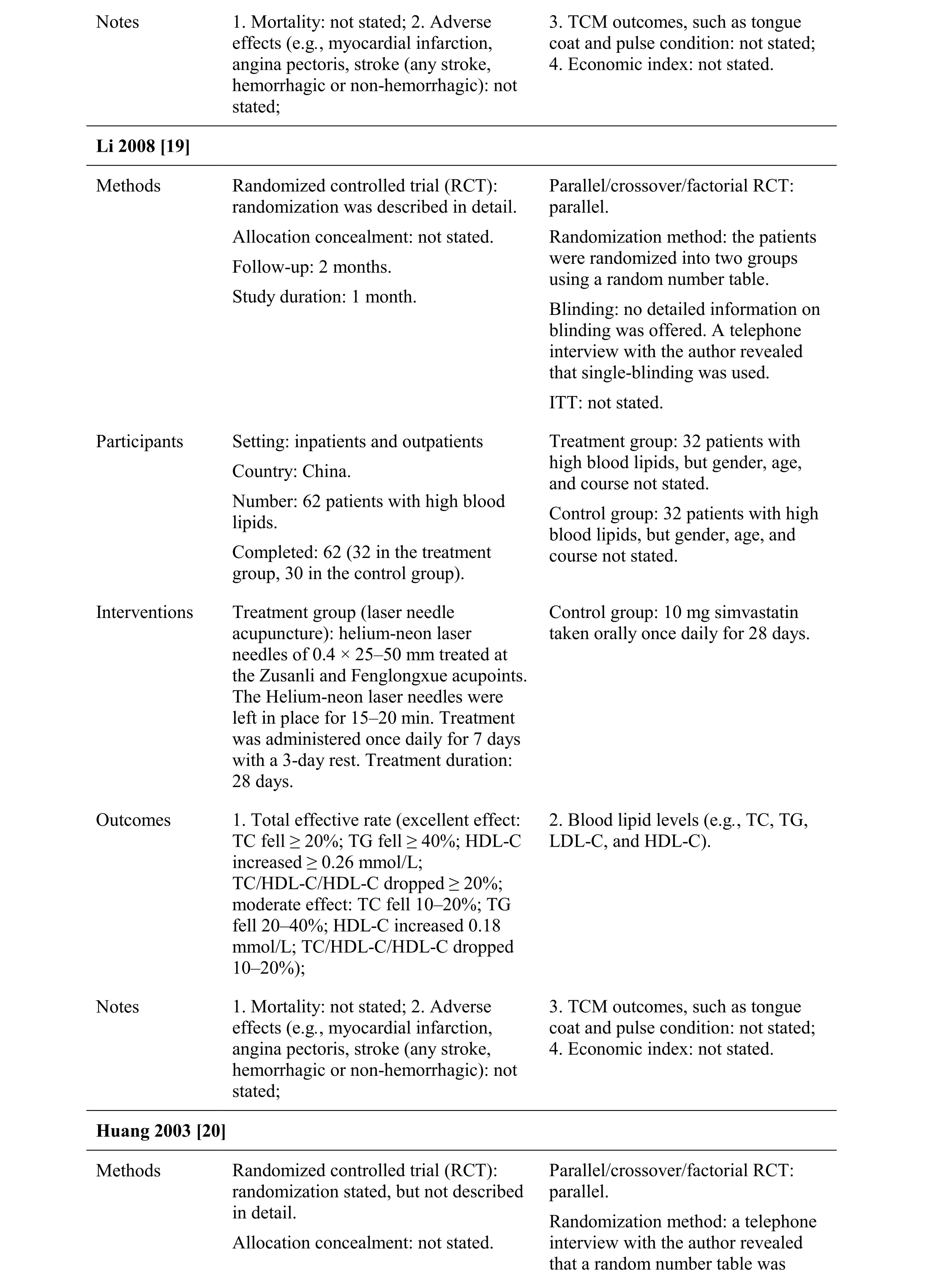
Figure 3 Methodological quality summary
Comparison 1: Acupuncture alone versus placebo or sham acupuncture
Two studies compared acupuncture with sham acupuncture. One [22] assessed electro-acupuncture,while the other [26] assessed magnetic needles.
Total effective rate.Studies that compared acupuncture aloneversusplacebo or sham acupuncture reported no significant difference in the total effective rate between the two groups (Figure 4; analysis 1.1; RR, 0.95; 95%CI,0.72-1.24).
TC.One study compared acupuncture aloneversusplacebo or sham acupuncture and reported a significant difference in TC between the two groups (Figure 5;analysis 1.2; (MD, 0.85; 95%CI, -1.13- -0.56).
TG. One study compared acupuncture aloneversusplacebo or sham acupuncture and reported no significant difference in TG between the two groups (Figure 6;analysis 1.3; (MD, -0.28; 95%CI, -0.71-0.14).
HDL-C:One study compared acupuncture aloneversusplacebo or sham acupuncture and reported a significant difference in HDL-C between the two groups (Figure 7;analysis 1.4; MD, 0.23; 95%CI, 0.08-0.37).
LDL-C:One study compared acupuncture aloneversusplacebo or sham acupuncture and reported a significant difference in LDL-C between the two groups (Figure 8;analysis 1.5; MD, -0.33; 95%CI, -0.63- -0.03).
Comparison 2: Acupuncture alone versus statins
Eight studies compared acupunctureversusstatins. One study [18] assessed moxibustion, three [17, 19, 21]assessed needle acupuncture, two [13, 24] assessed electro-acupuncture, and two [30, 32] assessed acupoint catgut embedding.
Total effective rate.Studies that compared acupuncture and statins reported no significant differences in the total effective rate between the two groups (Figure 9; analysis 2.1; RR, 1.10; 95%CI, 0.97-1.24).
Three studies [21, 19, 17] compared acupuncture and simvastatin and reported no significant difference in total effective rate (Figure 9; analysis 2.1.1 in analysis 2.1; RR,1.05; 95%CI, 0.95-1.16).
Four studies [18, 23, 24, 30] compared acupunctureversuspravastatin and reported a significant difference in total effective rate (Figure 9; analysis 2.1.2 in analysis 2.1;RR, 1.30; 95%CI, 1.10-1.55).
One study [32] compared acupunctureversusatorvastatin and reported no significant increase in total effective rate (Figure 9; analysis 2.1.3 in analysis 2.1; RR,0.93; 95%CI, 0.78-1.10).
TC.One study compared acupunctureversusstatins and reported no significant difference in TC between the two groups (Figure 10; analysis 2.2; MD, -0.03; 95%CI,-0.16-0.09).
Three studies [21, 19, 17] compared acupunctureversussimvastatin and reported no significant difference in TC (Figure 10; analysis 2.2.1 in analysis 2.2; MD,-0.15; 95%CI, -0.60–0.29).
Four studies [30, 18, 23, 24] compared acupunctureversuspravastatin and reported no significant difference in TC (Figure 10; analysis 2.2.2 in analysis 2.2; MD, 0.02;95%CI, -0.16–0.19).
TG:One study compared acupunctureversusstatins and reported a significant difference in TG between the two groups (Figure 11; analysis 2.3; MD, 0.20; 95%CI, 0.07–0.33).
Three studies [21, 19, 17] compared acupunctureversussimvastatin, but no significant difference in TG was identified (Figure 11; analysis 2.3.1 in analysis 2.3;MD, 0.00; 95%CI, -0.20-0.21).
Four studies [30, 18, 23, 24] compared acupunctureversuspravastatin and reported a significant difference in TG (Figure 11; analysis 2.3.2 in analysis 2.3; MD, 0.30;95%CI, 0.16-0.44).
HDL-C:One study compared acupunctureversusstatins and reported a significant difference in HDL-C between the two groups (Figure 12; analysis 2.4; MD, -0.11; 95%CI, -0.16- -0.07).
Three studies [21, 19, 17] compared acupunctureversussimvastatin and reported no significant difference in HDL-C (Figure 12; analysis 2.4.1 in analysis 2.4; MD,-0.06; 95% CI, -0.22-0.11).
Four studies [30, 18, 23, 24] compared acupunctureversuspravastatin and reported a significant difference in HDL-C (Figure 12; analysis 2.4.2 in analysis 2.4; MD,-0.11; 95% CI, -0.17- -0.06).
LDL-C:One study compared acupunctureversusstatins and reported a significant difference in LDL-C between the two groups (Figure 13; analysis 2.5; MD, 0.42; 95%CI, 0.32-0.52).
Three studies [21, 19, 17] compared acupunctureversussimvastatin and reported no significant difference in LDL-C (Figure 13; analysis 2.5.1 in analysis 2.5; MD,0.23; 95% CI, -0.29-0.74).
Four studies [30, 18, 23, 24] compared acupunctureversuspravastatin and reported a significant difference in LDL-C (Figure 13; analysis 2.5.2 in analysis 2.5; MD,0.43; 95% CI, 0.33-0.53).
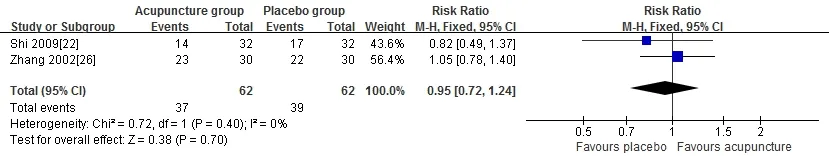
Figure 4 Comparison: acupuncture alone versus placebo or sham acupuncture: outcome 1: total effective rate
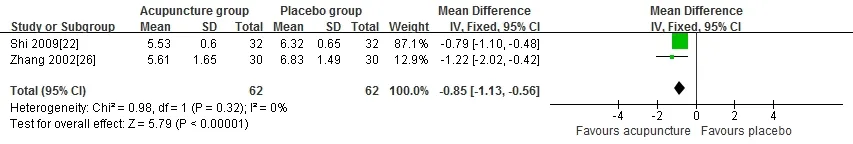
Figure 5 Comparison: acupuncture alone versus placebo or sham acupuncture: outcome 2: TC
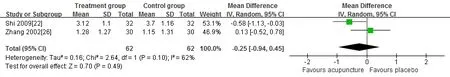
Figure 6 Comparison: acupuncture alone versus placebo or sham acupuncture: outcome 3: TG
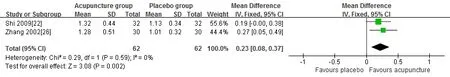
Figure 7 Comparison: acupuncture alone versus placebo or sham acupuncture: outcome 4: HDL-C
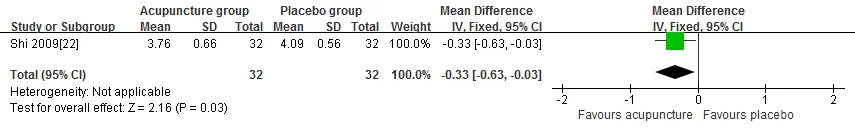
Figure 8 Comparison: acupuncture alone versus placebo or sham acupuncture: outcome 5: LDL-C
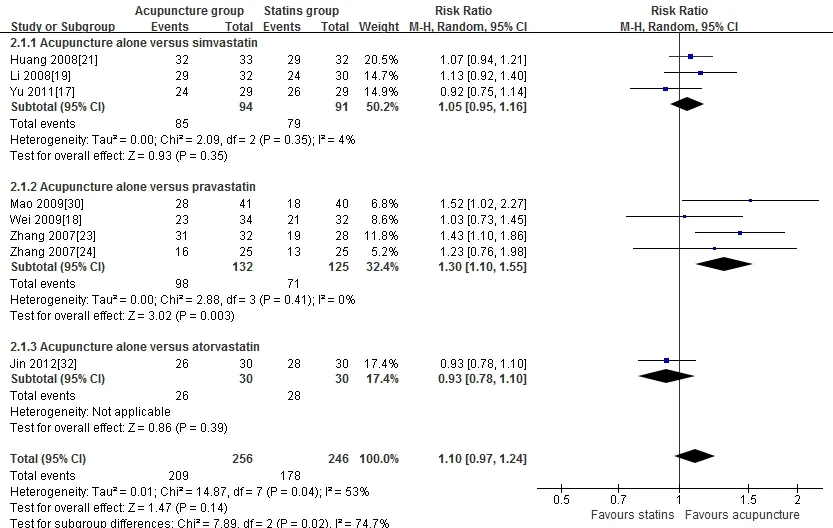
Figure 9 Comparison: acupuncture alone versus statins: outcome 1: total effective rate
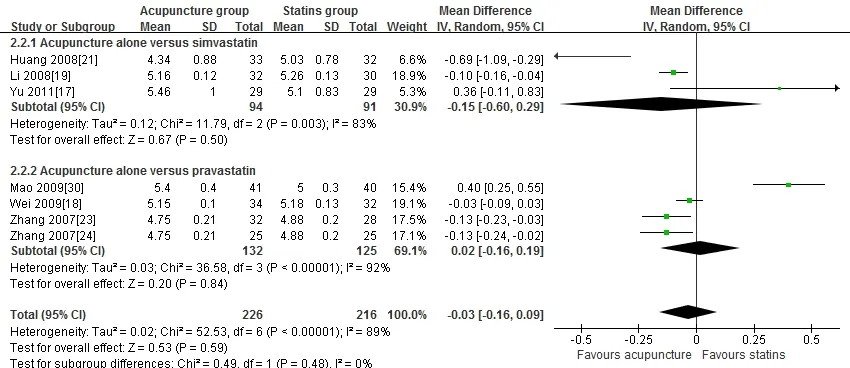
Figure 10 Comparison: acupuncture alone versus statins: outcome 2: TC
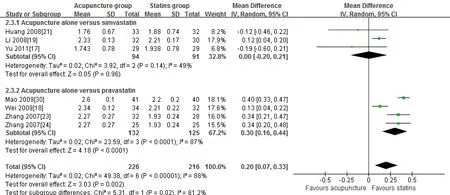
Figure 11: Comparison: acupuncture alone versus statins: outcome 3: TG.
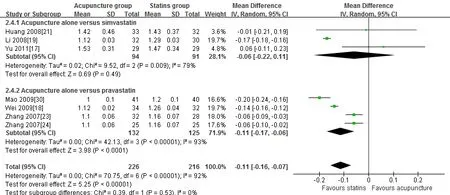
Figure 12 Comparison: acupuncture alone versus statins: outcome 4: HDL-C.
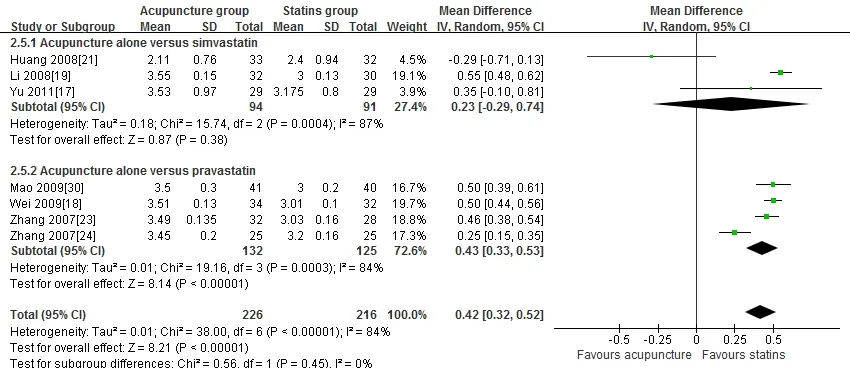
Figure 13 Comparison: acupuncture alone versus statins: outcome 5: LDL-C.
Comparison 3: Acupuncture alone versus Chinese herbal preparations
Four studies compared acupunctureversusChinese herbal preparations. One study [20] assessed needle acupuncture,one [25] assessed electro-acupuncture, one [27] assessed acupoint injection, and one [28] assessed auricular acupoint.
Total effective rate.Studies that compared acupunctureversusChinese herbal preparations reported no significant difference in the total effective rate between the two groups (Figure 14; analysis 3.1; RR, 0.97; 95%CI,0.89-1.06).
TC.One study compared acupunctureversusChinese herbal preparations and reported no significant difference in TC between the two groups (Figure 15; analysis 3.2;MD, -0.10; 95%CI, -0.43-0.23).
TG.One study compared acupunctureversusChinese herbal preparation and reported no significant difference in TG between the two groups (Figure 16; analysis 3.3;MD, -0.05; 95%CI, -0.36-0.26).
HDL-C.One study of acupunctureversusChinese herbal preparations reported no significant difference in HDL-C between the two groups (Figure 17; analysis 3.4; MD,-0.06; 95%CI, -0.08-0.21).
LDL-C.One study compared acupunctureversusChinese herbal preparations and reported no significant difference in LDL-C between the two groups (Figure 18;analysis 3.5; MD, -0.15; 95%CI, -0.37-0.07).
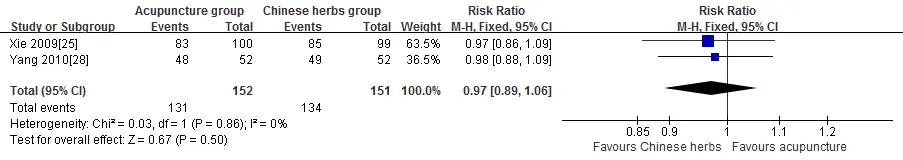
Figure 14 Comparison: acupuncture alone versus Chinese herbal preparations outcome 1: total effective rate
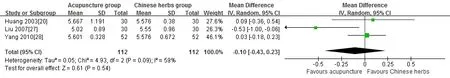
Figure 15 Comparison: acupuncture alone versus Chinese herbal preparation outcome 2: TC
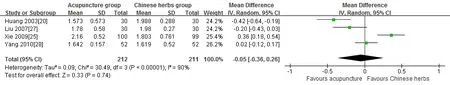
Figure 16 Comparison: acupuncture alone versus Chinese herbal preparation outcome 4: TG
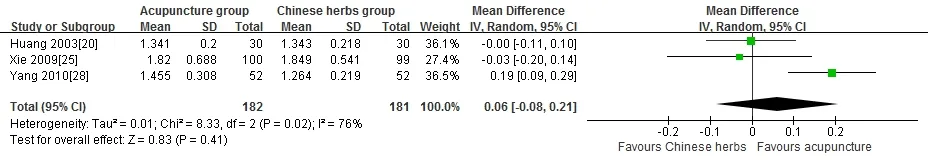
Figure 17 Comparison: acupuncture alone versus Chinese herbal preparations outcome 5: HDL-C
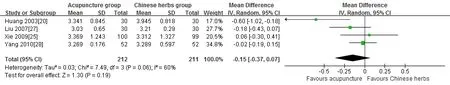
Figure 18 Comparison: acupuncture alone versus Chinese herbal preparations outcome 6: LDL-C
Comparison 4: Acupuncture plus other treatment versus other treatments alone
Three studies compared acupuncture plus other treatmentsversusother treatments. One study [29]assessed auricular acupoints, and two [31, 33] assessed acupoint catgut embedding.
Total effective rate.Studies that compared acupuncture plus other treatmentversusother treatments reported no significant difference in total effective rate between the two groups (Figure 19; analysis 4.1; RR, 1.04; 95%CI,0.87-1.25).
TC.Studies that compared acupuncture plus other treatmentsversusother treatments reported no significant difference in TC between the two groups (Figure 20;analysis 4.2; MD, -0.15; 95%CI, -0.37-0.06).
TG:Studies that compared acupuncture plus other treatmentsversusother treatments reported no significant difference in TG between the two groups (Figure 21;analysis 4.3; MD, -0.19; 95%CI, -0.46-0.08).
HDL-C:Studies that compared acupuncture plus other treatmentsversusother treatments reported no significant difference in HDL-C between the two groups (Figure 22;analysis 4.4; MD, 0.11; 95%CI, -0.04-0.26).
LDL-C:Studies that compared acupuncture plus other treatmentsversusother treatments reported no significant difference in HDL-C between the two groups (Figure 23;analysis 4.5; MD, -0.45; 95%CI, -1.30-0.39).
Other outcomes.Mortality, adverse effects, TCM outcomes, such as the tongue coat and pulse condition,and economic index were not reported by 14 studies.
GRADE quality of evidence.The “GRADEprofiler” of the Cochrane Collaboration Network was used to classify the systematic review results (Table 2). The quality of evidence was low.
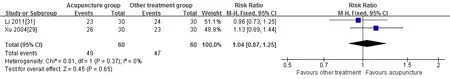
Figure 19 Comparison: acupuncture plus other treatments versus other treatments: outcome 1: total effective rate
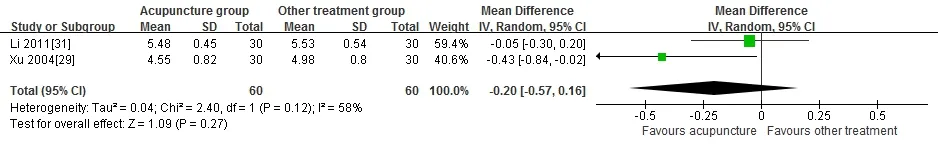
Figure 20 Comparison: acupuncture plus other treatments versus other treatments: outcome 2: TC
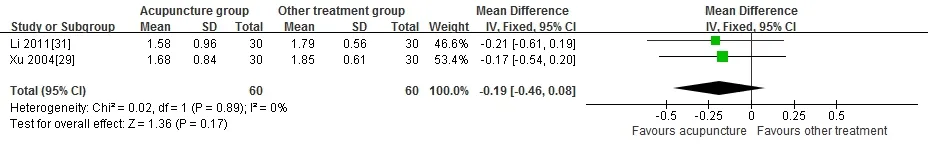
Figure 21 Comparison: acupuncture plus other treatments versus other treatments: outcome 3: TG
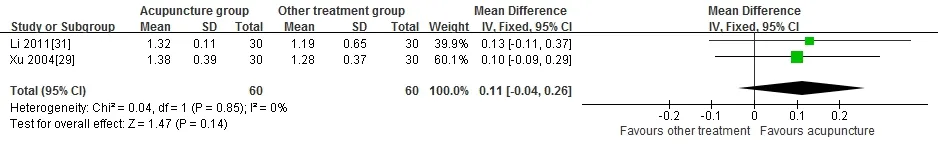
Figure 22: Comparison: plus other treatments versus other treatments: outcome 4: HDL-C
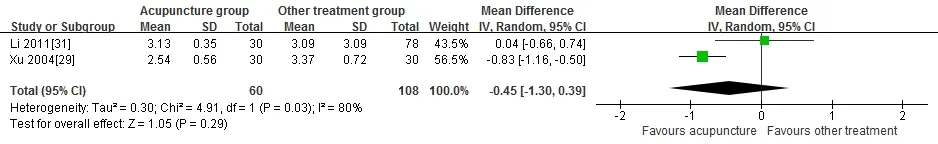
Figure 23 Comparison: acupuncture plus other treatments versus other treatments: outcome 5: LDL-C
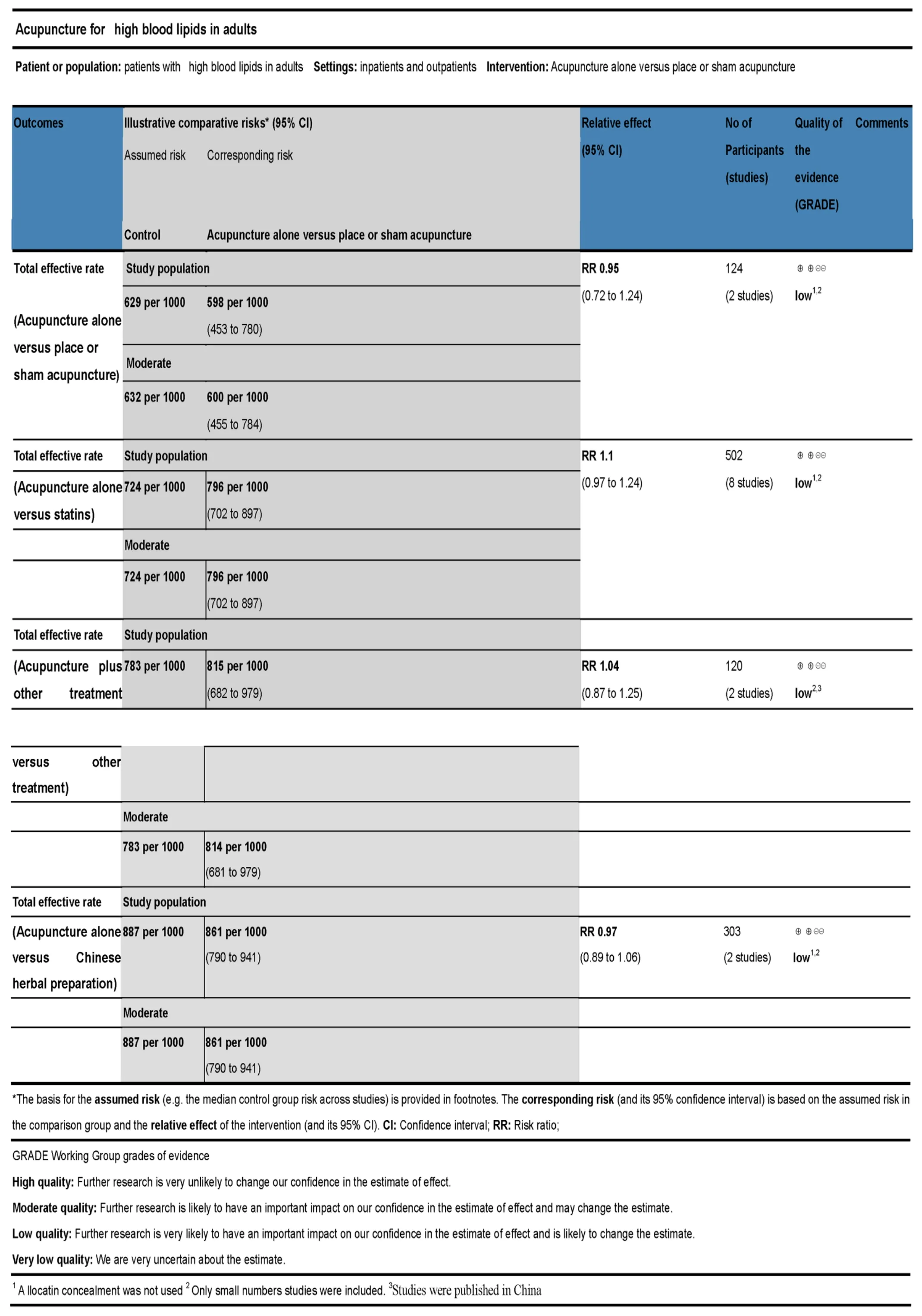
Table 2 GRADE quality of evidence
Discussion
Summary of main results
Seventeen RCTs were included in this review. They assessed different forms of acupuncture (needle acupuncture, moxibustion, electro-acupuncture, magnetic needle, acupoint injection, auricular acupoint, and acupoint catgut embedding) plus other treatments compared to other treatments or without other treatments compared to sham treatments or other treatments.
Sham acupuncture and acupressure treatment were equally effective (including one electro-acupuncture and one magnetic needle study). Acupressure was as effective as statin treatment (three needle acupuncture studies, two electro-acupuncture studies, one moxibustion study, and one acupoint catgut embedding study). However,acupuncture treatment was not as effective as pravastatin treatment but was as effective as simvastatin or atorvastatin treatment. Acupuncture treatment was as effective as Chinese herbal preparation treatment (one electro-acupuncture study and one auricular acupoint study). Acupuncture treatment was not effective compared with acupuncture plus other treatments (one electro-acupuncture study and one auricular acupoint study).
We found limited evidence to suggest that acupressure decreased TC, LDL-C, and increased HDL-C compared with either placebo or sham acupuncture. Acupressure may increase HDL-C, but insufficient evidence was available to determine an effect on TG.
Acupressure may increase HDL-C to a greater degree than statin treatment, but there was no statistical difference. No sufficient evidence was available to determine whether acupressure decreased TC, TG;however, two electro-acupuncture studies reported decreased TC. Acupuncture may increase total effective rate when compared against pravastatin, but no difference in total effective rate when compared against simvastatin and atorvastatin.
Insufficient evidence was available to determine whether acupressure decreased TC, TG, and LDL-C compared with Chinese herbal preparation treatment.There was also insufficient evidence to determine whether acupressure increased HDL-C; however, one acupoint injection study [27] reported decreased TC, one acupuncture study [20] reported decreased TG, and one auricular acupoint study [28] reported an increase in HDL-C. There was insufficient evidence to determine whether acupressure decreased TC, TG, and LDL-C compared with acupuncture plus other treatments.Insufficient evidence was available to determine whether acupressure increased HDL-C.
Overall completeness and applicability of evidence
No evidence suggested that acupressure treatment of adults with high blood lipids was ineffective. Further studies are needed to validate the findings of this review and to determine the efficacy of acupuncture in patients with high blood lipids in comparison with other therapies.
RCTs should be conducted in accordance with the internationally recognized CONSORT and STRICTA criteria [34].
Quality of evidence
The quality of the evidence was low because the findings were from small, single-center studies.
Conclusion
Acupuncture serve as a feasible option for high blood lipids in adults. However, there is insufficient evidence to confirm a decrease in adverse effects, mortality, or TCM outcomes (such as tongue coat and pulse condition). The quality of the evidence was low. Thus, larger, multicenter,high-methodological-quality studies of acupuncture treatment of high blood lipids in adults are needed. These should include patients with high blood lipids and who are undergoing acupuncture interventions. More data,particularly concerning adverse events, need to be reported to guide clinical application. Future studies should determine the most suitable acupuncture forms and acupoints for treatment of high blood lipids.
Acknowledgments
We thank the Second Outpatient Department, First Affiliated Hospital, Guangzhou University of Chinese Medicine
 TMR Modern Herbal Medicine2018年2期
TMR Modern Herbal Medicine2018年2期
- TMR Modern Herbal Medicine的其它文章
- A meta-analysis of randomized controlled trials of Yiyiren Decoction in the treatment of rheumatoid arthritis
- Chinese medicine in the treatment of intracranial vascular stenosis in 1 case
- Clinical evaluation of Xiaoyao Jieyu prescription in the treatment of persistent postural-perceptual dizziness
- Shenxian Shengmai Oral Liquid for treatment of slow arrhythmia: a randomized controlled trial
- Metabolites identification and quantification of antcin H in mice tumors after oral administration of the anticancer mushroom Antrodia camphorata
- Progress of Alzheimer’s disease related glucose metabolism regulating hormones and a research perspective in nootropics of herbal medicine
