Chinese medicine in the treatment of intracranial vascular stenosis in 1 case
Di Wu, Wei-Ying Dai
1Tianjin Huanhu Hospital, Tianjin, China.
Abstract Intracranial vascular stenosis is closely related to transient ischemic attack (TIA) and cerebral infarction, early prevention and treatment of intracranial vascular stenosis can prevent cerebral infarction and improve the prognosis of stroke. Western medicine employs interventional surgery or vasodilator, antiplatelet drugs, lipid lowering drugs,plaque-stabilizing agents and other drugs for treating intracranial vascular stenosis. No corresponding disease name with“intracranial vascular stenosis” is found in Chinese medicine literature. Based on the characteristics of syndromes,symptoms and diseases, “intracranial vascular stenosis” is summarized as weakened body resistance and prevailed pathogenic factors, phlegm with blood stasis and “obstruction (Bi) syndrome” in the brain. The self-made Chinese herbal“Naomaitong” prescription treating for bilateral middle cerebral artery stenosis in 1 case got satisfactory efficacy by transcranial doppler (TCD) and computed tomography angiography (CTA) examination.
Keywords: Intracranial vascular stenosis, “Naomaitong” prescription, Chinese medicine treatment
Background
Internal carotid artery (intracranial segment, extracranial segment) stenosis is an independent risk factor for ischemic cerebrovascular disease. Western medicine adopts interventional surgery or drug treatment based on the degree of vascular stenosis, location and the patient’s age, physical condition and other assessment results.Western medicine mainly focuses on dilating blood vessels, anti-platelet aggregation, lowering lipid, and stabilizing plaque. The self-made Chinese herbal“Naomaitong” prescription treating for bilateral middle cerebral artery stenosis in 1 case got satisfactory efficacy by transcranial doppler (TCD) and computed tomography angiography (CTA) examination.
Case introduction
Mr Ding, male, 44 years old, went to the traditional Chinese medicine clinic for treatment mainly due to“cerebral vascular stenosis” on April 12th 2017. Course of disease: The patient was admitted to the neurology department of our hospital 3 months ago (2017.1.23) due to “paroxysmal barylalia, weakness of the right limb for half a day”. No abnormality was found in the intraday CT of the head in the emergency department of other hospital.After hospital admission, the patient was rechecked by magnetic resonance imaging (MRI) of the head and reported that: abnormal signal was found in diffusion-weighted imaging of the left basal ganglia and left periventricular, which was considered to be acute cerebral infarction (Figure 1-1 ~ Figure 1-4). After taking symptomatic treatment like anticoagulant therapeutic,fiber reduction, lowering lipid, stabilizing plaque,improving cerebral circulation metabolism, protection of gastrointestinal mucosa, and reducing phlegm and others for 10 days, the patient was discharged when the disease was relatively in stable condition. Relevant inspection results during hospitalization: 2017.1.25 TCD reported that left middle cerebral artery stenosis was severe, right middle cerebral artery stenosis was moderate, the velocity of the blood flow of right vertebral artery slowed down,and systolic notch and frequency spectrum of the blood flow were poor. Cervical ultrasound showed no abnormalities.
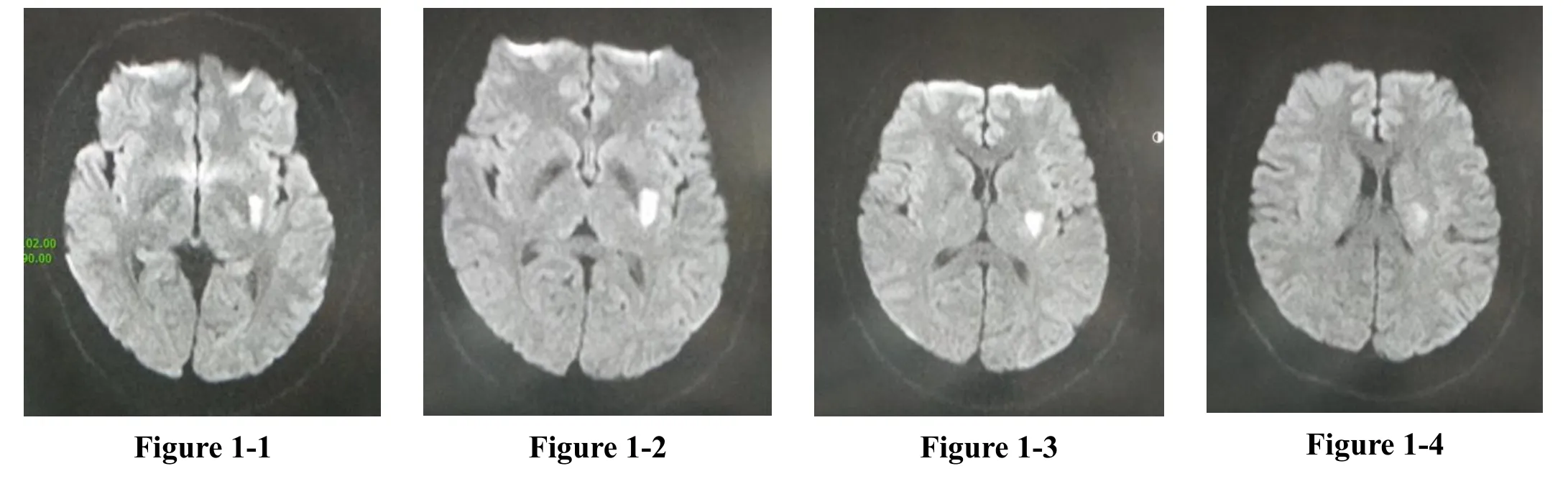
Figure 1 2017.1.23 head MRI: acute cerebral infarction in left basal ganglia and left periventricular area
2017.1.26 Aortic arch-intracranial CTA reported that no abnormalities were found in aortic arch-carotid artery,the extracranial segment of vertebral artery system. The bilateral MCA M1 segment was moderately stenotic(Figure 2-1 ~ Figure 2-3). When taking consultation with neurosurgery, the patient had no indications of surgical intervention, it was recommended to strengthen the drug treatment to prevent recurrent strokes.
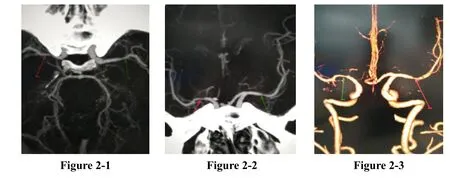
Figure 2 2017.1.26 aortic arch-intracranial CTA: aortic arch-carotid artery and extracranial segment of vertebral artery system showed no abnormalities, bilateral MCA M1 was moderate stenosic
The patient experienced occasional dizziness, tinnitus cerebri, anxiety and fatigue and restless sleep without taking any medication after hospital discharge in three months. The patient was a Hepatitis B virus carrier with moderate fatty liver, was reluctant to take western medicine, and sought medical advice from Chinese medicine. Physical examination: Bp133/74 mmHg, lung sounds were clear, and no rhonchi and moist rales were heard. The patient had strong heart sounds and regular heart rhythm, and pathological murmur was not heard in auscultatory value areas. Abdomen was soft and non-tender, both liver and spleen under ribs were not felt,and lower extremities were not swollen and without deformity of extremities and spine. Physical examination in neurology department: consciousness, language fluency, equal size and round pupils, left: right = 3mm: 3 mm, light response (+), full eye movement, no nystagmus,symmetric bilateral nasolabial fold, tongue lolls unbiasedly, soft neck, muscle strength of limbs was grade V, normal muscle tone, tendon reflexes (++), Babinski sign bilaterally (-) and symmetric bilateral superficial sensibility. Coordination of four limbs can be checked by.TCD reported: severe left middle cerebral artery stenosis,moderate right middle cerebral artery stenosis, flow velocity of right posterior cerebral artery, right vertebral artery slowed down, and blood flow spectrum was poor.Compared with TCD on 25thJanuary 2017, blood flow velocity of left anterior cerebral artery (LMCA) and right middle cerebral artery (RMCA) were faster, suggesting the exacerbation of vascular stenosis (Table 1).
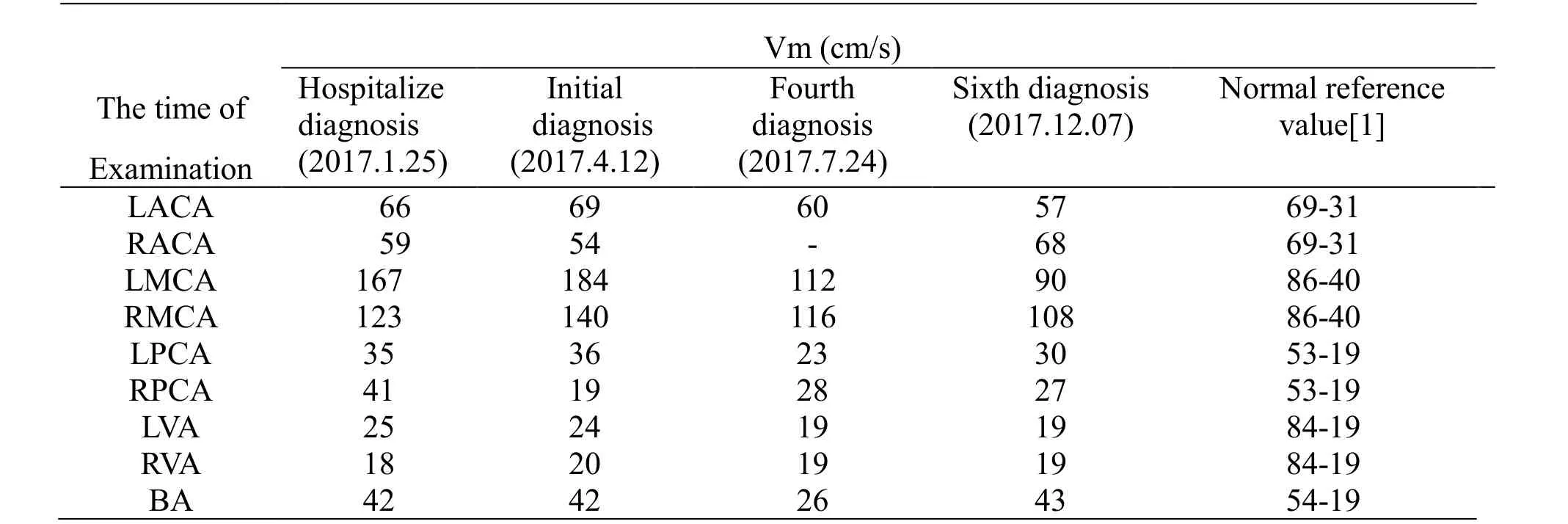
Table I Average blood flow velocity (Vm) examined by TCD for three times before and after treatment and the normal reference value
Cervical vascular ultrasound showed no abnormalities.Blood glucose, blood lipids, hemorheology, fibrinogen,homocysteine, liver and kidney function were all normal.Tongue and pulse condition: tongue was dull, the edge of tongue was with shallow tooth marks, coating on the tongue was white, and wiry pulse was deep. Diagnosis of traditional Chinese medicine: impediment of vessels(obstruction of cerebral vein). Diagnosis of western medicine: cerebral vascular stenosis (bilateral MCA M1 segment was moderate stenosis). The disease is treated by“Naomaitong” prescription: Tianma (Gastrodiae Rhizoma)10 g, Chuanxiong (Chuanxiong Rhizoma) 10 g,Shichangpu (Acori Tatarinowii Rhizoma) 10 g, Danshen(Salviae Miltiorrhizae Radix Et Rhizoma) 15 g, Gegen(Puerariae Lobatae Radix) 10 g, Shuizhi (Hirudo) 10 g,Chishao (Paeoniae Radix Rubra) 10 g, Sanqi(Notoginseng Radix Et Rhizoma) 6 g, Renshen (Ginseng Radix Et Rhizoma) 10 g, Ruxiang (Olibanum) 10 g,Xiebai (Allii Macrostemonis Bulbus) 10 g, Shanzha(Crataegi Fructus) 10 g, Jianghuang (Curcumae Longae Rhizoma) 10 g, Jiangcan (Bombyx Batryticatus) 10 g,Chantui (Cicadae Periostracum) 6 g, Dahuang (Rhei Radix Et Rhizoma) 10 g, Yujin (Curcumae Radix) 10 g,Yuanzhi (Polygalae Radix), Zhenzhumu (Margaritifera Concha) 30 g, a total of 14 doses. Instructions: 2 packages of all ingredients of Chinese medicine granules per dose, 1 bag dissolved and taken with 200 mL warm water for each morning and evening. Second ambulatory treatment on 25thApril 2017: the patient complained in half a month he had no dizziness and tinnitus cerebri, and the spirit was better than before, the fatigue improved and he can have a good sleep at night and work normally. BP:110/85mmHg, physical examination was accordance with the former, the tongue was pale, the edge of the tongue has a shallow tooth mark, coating on the tongue was yellow and white, and wiry pulse was deep.“Naomaitong” prescription plus Lianzixin (Nelumbinis Plumula) and Danzhuye (Lophatheri Herba) 10g were continued to take by 30 doses. Third ambulatory treatment on 25thMay 2017: The patient had good spirit.The chief complaint was that in recent one month he didn’t develop dizziness and tinnitus cerebri and had good appetite. He could sleep soundly, and his defecate and urinate harmonized. BP: 105/75 mmHg, physical examination was accordance with the former, tongue was dark with white coating on the tongue, and wiry pulse was deep. The patient was treated with “Naomaitong”prescription for two month. Fourth ambulatory treatment on 24thJuly 2017: the patient complained he had no discomfort. BP: 130 / 85mmHg, physical examination was accordance with the former, the tongue was dark with white coating on the tongue, and wiry pulse was deep.TCD reported that his bilateral middle cerebral artery was slightly stenotic and the spectrum of blood flow was poor.Compared with the TCD reports on 25thJanuary 2017 and 12thApril 2017, the blood flow of LMCA and RMCA decreased significantly (Table 1), suggesting that the degree of vascular stenosis reduced. Taking“Naomaitong” prescription for another two month, the patient made an appointment to have a reexamination by CTA. On 4thSeptember 2017 aortic arch-intracranial was checked by CTA and reported that no abnormalities were found in the extracranial segment of the aortic arch-carotid artery and vertebral artery system. The right MCA M1segment was slightly stenosed (Figure 3-1 to Figure 3-3). Blood glucose, blood lipids, hemorheology,fibrinogen, homocysteine, liver and kidney function were all normal. Fifth ambulatory treatment on 12thOctober 2017: the patients had no complaints. BP: 110/80 mmHg,physical examination was accordance with the former,tongue was pale with red coating on the tongue, and wiry pulse was deep. “Naomaitong” prescription was taken for another two month. Sixth ambulatory treatment on 7thDecember 2017: the patients had no complaint. BP:120/80 mmHg, physical examination was accordance with the former, tongue was light red with white coating,and wiry pulse was deep. No abnormality was found by checking the neck vascular ultrasound. TCD reported:blood flow velocity of bilateral middle cerebral artery got slightly faster. Compared with TCD reports on 25thJanuary 2017, 12thApril 2017 and 24thJuly 2017, the blood flow velocity of LMCA and RMCA decreased significantly, which was close to the normal value (Table 1). Blood sugar, blood lipids, hemorheology, fibrinogen,homocysteine, liver and kidney function were normal.
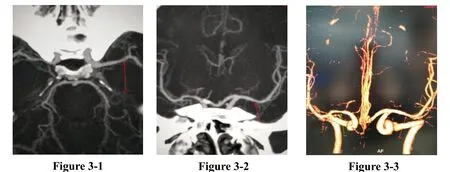
Figure 3 2017.9.4 aortic arch - intracranial CTA: no abnormality was found in aortic arch - carotid and extracranial segment of vertebral artery system, right MCA M1 segment was slightly stenosis.
Discussion
In this case, there was no abnormality in head CT examination when there was a symptom of “paroxysmal barylalia and weakness of the right limb” occurred. After 11 hours, MRI showed left basal ganglia and left cerebral ventricle had acute cerebral infarction (Figure 1-1 –Figure 1-4), and the disease progressed rapidly. The patient had a history of smoking for 10 years with an average of 3-4 boxes/day and quitted for 6 years. And he had a history of drinking for 20 years with an average of 5 taels/day. Blood pressure, blood glucose, blood lipids,hemorheology, fibrinogen, homocysteine and related indicators were normal. He denied the family history of genetic disease. Severe (moderate) bilateral MCA stenosis were found by TCD and CTA. Cerebrovascular stenosis, long-term smoking and drinking history may be the main risk factors for TIA and cerebral infarction of the patient.
The middle cerebral artery is a branch of the internal carotid artery that continues directly. Most of the blood in the internal carotid artery flowed into MCA The bilateral MCA M1 segment, namely posterior orbit segment,extended horizontally outward about 3 cm long in the front and back of the radiography [2]. Studies had shown that CTA and digital subtraction angiography can show the stenosis of MCA accurately, though TCD had limitations, nevertheless the accuracy of the three methods for the diagnosis of MCA M1 stenosis had no significant difference (P> 0.05) [3]. Intracranial stenosis can reduce the perfusion pressure of distal vascular, make the watershed area have insufficient blood supply, and the low perfusion infarction or watershed infarction was formed [4]. Intracranial vascular stenosis is closely related to TIA and cerebral infarction [5]. Early prevention and treatment of intracranial vascular stenosis can effectively reduce the probability of TIA transforming into cerebral infarction within a week [6] and improve stroke prognosis [4].
“Intracranial vascular stenosis” has no corresponding name in Chinese medicine literature. The writer summarized it as vessel impediment which location was in the brain with weakened body resistance and pathogenic stagnation, phlegm with blood stasis, based on the characteristics of its symptoms, syndromes and disease. “Suwen-Bilunpiandisishisan” recorded “when the impediment was in the vessel, the blood clotted and stopped flowing” [7]. “Yixuezhengzhuan” recorded “Qi is Yang, blood is Yin, blood flows in the vessels, Qi goes outside of arteries and veins, and they circulate mutually,……Qi gets pathogenic factor and forms stagnation. Body fluid is sticky, can become phlegm and fluid retention, and seeps into the vein for a long time accumulation. It makes blood turbid, which suggests Yin stagnates Yang. Blood turns stagnation when gets pathogenic factor, and vessels were blocked, then it overflows or knots, it seeps out of the vessels for a long time accumulation, it makes Qi disordered, which suggests Yang stagnates Yin” [8]. It suggests the etiology and pathogenesis of “cerebral artery block disease”formation were due to weakened body resistance and pathogenic stagnation, the mutual stagnation of Yin and Yang, disorder of qi movement, the mutual interference of clear Qi and foul Qi, phlegm with blood stasis, and congestion of the vessels. At the initial stage, patients with intracranial vascular stenosis often has no obvious clinical symptoms. With the degree of vascular stenosis increasing, dizziness, headache, tinnitus cerebri, TIA and even stroke symptoms gradually appear.“Suwen-Bilunpiandisishisan” said “patients without painness and numbness falls ill and gets deeply gradually;defensive Qi and Ying Qi were obscure, main and collateral channels were blocked, and skin has no nutrition, which means disturbance of perception” [7] .
Chinese medicine “Naomaitong” prescription was established based on the combination of syndromes,symptoms and disease to form prescriptions and selected drugs aiming at the main pathogenesis of intracranial vascular stenosis. In the prescription, Tianma (Gastrodiae Rhizoma), Chuanxiong (Chuanxiong Rhizoma), Gegen(Puerariae Lobatae Radix), and Shichangpu (Acori Tatarinowii Rhizoma) are monarch, dispelling wind and removing obstruction in the meridians, eliminating phlegm and inducing resuscitation, dredging blood vessel of brain, and directing the medicine to the sick place;Renshen (Ginseng Radix Et Rhizoma) and Ruxiang(Olibanum) are minister, tonifying Qi and dredging meridian and dredging aperture of brain; Danshen(Salviae Miltiorrhizae Radix Et Rhizoma), Shuizhi(Hirudo), Chishao (Paeoniae Radix Rubra), Sanqi(Notoginseng Radix Et Rhizoma) can promote blood circulation and clear and activate the channels and collaterals, invigorate pulse-beat and disperse obstruction;Xiebai (Allii Macrostemonis Bulbus) and Shanzha(Crataegi Fructus) were assistant, promoting qi circulation and removing obstruction in the collaterals,eliminating accumulation and resolving turbidity;Jianghuang (Curcumae Longae Rhizoma), Jiangcan(Bombyx Batryticatus), Chantui (Cicadae Periostracum),Dahuang (Rhei Radix Et Rhizoma) are guide, exerting“rising and falling” effect, promoting blood circulation and attacking accumulation, reducing phlegm and resolving masses, elevating clear qi to lower turbid, and draining the vessels of brain. A total of sixteen herbs of Chinese medicine can drain the vessels of brain, eliminate accumulation and resolve turbidity, the treatment of“cerebral palsy resistance” has a significant effect.
Modern pharmacological studies have shown that:Renshen (Ginseng Radix Et Rhizoma), Chuanxiong(Chuanxiong Rhizoma) and Gegen (Puerariae Lobatae Radix) can dilate cerebrovascular and increase cerebral blood flow [9-11]; Shichangpu (Acori Tatarinowii Rhizoma) resists cerebral ischemia-reperfusion injury,reduces cerebral cortical neuronal apoptosis and protects neurons [12]: Tianma (Gastrodiae Rhizoma) can promote the generation of endogenous vasodilators and inhibit the release of endogenous vasoconstrictor substances, and have a good antihypertensive effect [13]; Chishao(Paeoniae Radix Rubra) and Jianghuang (Curcumae Longae Rhizoma) exert anti-platelet aggregation effect,Jianghuang (Curcumae Longae Rhizoma) can also prevent PTCA postoperative restenosis [14, 15]; Shuizhi(Hirudo) and Jiangcan (Bombyx Batryticatus) can reduce the content of fibrinogen [16, 17]; Xiebai (Allii Macrostemonis Bulbus) and Shanzha (Crataegi Fructus)regulate lipid [18, 19]; Sanqi (Notoginseng Radix Et Rhizoma) and Danshen (Salviae Miltiorrhizae Radix Et Rhizoma) can improve microcirculation, and have anti-atherosclerosis action [20, 21]; Dahuang (Rhei Radix Et Rhizoma) can scavenge free radicals and antioxidant effect [22]. This case shows that “Naomaitong”prescription can exactly reduce the degree of cerebral vascular stenosis, prevent TIA and cerebral infarction,and have the effect of regulating blood lipid and lowering blood pressure. Long-term use has no adverse effect on liver and kidney function. Its mechanism is worth further study.
 TMR Modern Herbal Medicine2018年2期
TMR Modern Herbal Medicine2018年2期
- TMR Modern Herbal Medicine的其它文章
- Acupuncture for hyperlipidaemia in adults: A systematic review and meta-analysis
- A meta-analysis of randomized controlled trials of Yiyiren Decoction in the treatment of rheumatoid arthritis
- Clinical evaluation of Xiaoyao Jieyu prescription in the treatment of persistent postural-perceptual dizziness
- Shenxian Shengmai Oral Liquid for treatment of slow arrhythmia: a randomized controlled trial
- Metabolites identification and quantification of antcin H in mice tumors after oral administration of the anticancer mushroom Antrodia camphorata
- Progress of Alzheimer’s disease related glucose metabolism regulating hormones and a research perspective in nootropics of herbal medicine
