Thyrotoxicosis induced cardiogenic shock rescued by extracorporeal membrane oxygenation
Seunghwan Kim, Sang-Hoon Seol, Yun-Seok Kim, Dong-Kie Kim, Ki-Hun Kim, Doo-Il Kim
Department of Internal Medicine, INJE University College of Medicine, Haeundae Paik hospital, Busan, South Korea
Cardiomyopahty is one of complications of thyrotoxicosis. About 6% of thyrotoxic patients develop heart failure,but less than 1% of the patients progress dilated cardiomyopathy with systolic left ventricular dysfunction.[1]Thyrotoxicosis induced cardiogenic shock has mortality as high as 30%.[2]Extracorporeal membrane oxygenation (ECMO)is an essential management tool to save the patient with cardiopulmonary collapse. A 52-year-old man with diabetes was referred to our hospital for evaluation of increasing cough, chest pain, and dyspnea on exertion. On admission,vital signs were as follows: temperature of 36.5°C; respiration 32; pulse, 108 and irregular; and blood pressure, 120/80 mmHg. There were no complaints of fever or weight loss.ECG was atrial fibrillation with rapid ventricular rate (Figure 1A). Chest X-ray revealed cardiomegaly with right sided pleural effusion (Figure 2A). Blood test was performed.Amino-transferase/alanine amino-transferse (AST/ALT):95/77 mg/dL, lactate dehydrogenase (LDH): 354 mg/dL,creatinine: 0.9 mg/dL, glucose: 345 mg/dL, cardiac enzyme(CK-MB/TNI: 54.6/2.72 ng/mL), and Pro-BNP: 2351 pg/mL were elevated. Transthoracic echocardiography showed severe left ventricular (LV) systolic dysfunction (< 20%) with no valvular dysfunction. Thyroid function tests were performed showing a suppressed serum thyrotropin (TSH): <0.01 mIU/L (0.27– 4.2) and elevated free thyroxine (FT4): >7.77 ng/dL (0.93–1.70). He was treated with anti-thyroid drug (methimazole), low dose beta blocker (propranolol).The patient’s condition progressively worsened and took a downhill course despite aggressive hemodynamic support with high doses of inotropic agents (dopamine, dobutamine,norepinephrine). Eighteen hours later, he developed cardiogenic shock with blood pressure 60/30 mmHg. Laboratory findings revealed multi-organ failure (AST/ALT: 1762/1043 mg/dL, creatinine: 2.5 mg/dL, LDH: 1895 mg/dL, lactic acid:8.6 mmol/L). Ventilator and venous-arterial ECMO was started. He was weaned from ECMO six days. ECG recovered normal sinus rhythm (Figure 2A). Coronary angiography showed normal coronary artery. Echocardiography showed improvement in LV function (ejection fraction increased from 19% to 40%) two weeks later. And chest X-ray showed improvement of cardiomegaly (Figure 2B).The patient was discharged with beta blocker, anti-thyroid drug. Hyperthyroidism is a very rare cause of dilated cardiomyopathy. Low cardiac output heart failure is one of complications of thyrotoxicosis. Thyrotoxic cardiomyopathy may occur in patients with underlying heart disease such as ischemic, hypertensive or valvular disease or atrial fibrillation due to the effects of increased cardiac preload, impaired left ventricular filling, rapid ventricular rate, and decreased contractile reserve.[3]Atrial fibrillation is the most important trigger factor for decompensated heart failure.[4]There is a high incidence of atrial fibrillation in thyrotoxicosis.[5]A thyroid hormone causes systolic and diastolic dysfunction due to direct toxic effect.[6]Main purpose of the management of heart failure is to restore a euthyroid state and to maintain state. Treatment should be initiated with an antithyroid drug, either propylthiouracil or methimazole.Beta-blockers can be a useful management for heart failure related hyperthyroidism, but should be used cautiously since it occasionally exacerbates symptoms. The treatment of atrial fibrillation should be limited to control ventricular rate, since cardioversion and maintenance of sinus rhythm usually cannot be lasted as long as the thyrotoxicosis continues.[7]The management of heart failure related hyperthyroidism is difficult and sometimes requires invasive monitoring. Though hyperthyroidism related cardiomyopathy is usually thought to be reversible, some patients might progress cardiogenic shock. Therefore, early detection and effective treatment of cardiac symptoms in patients with hyperthyroidism is crucial. The patients with multi-organ failure including heart failure, hepatic failure, renal failure, lactic acidosis are potentially fatal.[8,9]Blood lactic acid level is useful as the prognostic factor for critical care patients in intensive care unit.[10]ECMO is a kind of cardiopulmonary bypass system that maintains tissue oxygenation for a while in patient with severe cardiopulmonary disease. ECMO is usually indicated in those with compromised hemodynamic status as a bridging therapy to heart transplantation, but also to allow cardiovascular recovery.[11–13]Thyrotoxicosis-induced cardiogenic shock is frequently very critical. Mechanical hemodynamic support such as ECMO should be considered during the earlier stage of circulatory collapse.

Figure 1. Electrocardiogram showing atrial fibrillation with rapid ventricular response (A) and spontaneous restored normal sinus rhythm five days later (B).
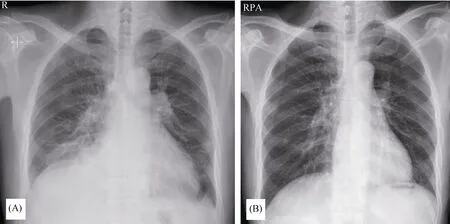
Figure 2. Chest X-ray showing cardiomegaly with right pleural effusion (A) and decreased cardiac chamber two weeks later (B).
References
1 Dahl P, Danzi S, Klein I. Thyrotoxic cardiac disease.CurrHeart Fail Rep2008; 5: 170–176.
2 Nayak B, Burman K. Thyrotoxicosis and thyroid storm.Endocrinol Metab Clin North Am2006; 35: 663–686.
3 Biondi B. Mechanisms in endocrinology: Heart failure and thyroid dysfunction.Eur J Endocrinol2012; 167: 609–618.
4 Siu CW, Yeung CY, Lau CP,et al. Incidence, clinical characteristics and outcome of congestive heart failure as the initial presentation in patients with primary hyperthyroidism.Heart2007; 93: 483–487.
5 Frost L, Vestergaard P, Mosekilde L. Hyperthyroidism and risk of atrial fibrillation or flutter: a population-based study.Arch Intern Med2004; 164: 1675–1678.
6 Marti V, Ballester M, Obrador D,et al. Active myocardial damage in hyperthyroidism. A concurrent mechanism of heart failure reversed by treatment.Eur Heart J1995; 16: 1014–1016.
7 Woeber KA. Thyrotoxicosis and the heart.N Engl J Med1992;327: 94–98.
8 Chong H, See K, Phua J. Thyroid storm with multiorgan failure.Thyroid2010; 20: 333–336.
9 Jiang YZ, Hutchinson KA, Bartelloni P,et al. Thyroid storm presenting as multiple organ dysfunction syndrome.Chest2000; 118: 877–879.
10 Smith I, Kumar P, Molloy S,et al. Base excess and lactate as prognostic indicators for patients admitted to intensive care.Intensive Care Med2001; 27: 74–83.
11 Chen YS, Yu HY, Huang SC,et al. Experience and result of extracorporeal membrane oxygenation in treating fulminant myocarditis with shock: what mechanical support should be considered first?J Heart Lung Transplant2005; 24: 81–87.
12 Allencherril J, Birnbaum I. Heart failure in thyrotoxic cardiomopathy: extracorporeal membrane oxygenation treatment for graves' disease.J Extra Corpor Technol2015; 47: 231–232.
13 Hsu LM, Ko WJ, Wang CH. Extracorporeal membrane oxygenation rescues thyrotoxicosis-related circulatory collapse.Thyroid2011; 21: 439–441.
 Journal of Geriatric Cardiology2018年2期
Journal of Geriatric Cardiology2018年2期
- Journal of Geriatric Cardiology的其它文章
- Intravascular ultrasound guided retrograde guidewire true lumen tracking technique for chronic total occlusion intervention
- Repetitive narrow QRS tachycardia in a 61-year-old female patient with recent palpitations
- Prediction of sudden death in elderly patients with heart failure
- Treatment of coronary in-stent restenosis: a systematic review
- Long term outcomes of drug-eluting stent versus coronary artery bypass grafting for left main coronary artery disease: a meta-analysis
- Adherence to pharmacological and non-pharmacological treatment of frail hypertensive patients
