Adherence to pharmacological and non-pharmacological treatment of frail hypertensive patients
Beata Jankowska-Polańska, Karolina Zamęta, Izabella Uchmanowicz, Anna Szymańska-Chabowska,Donald Morisky, Grzegorz Mazur
1Department of Clinical Nursing, Wroclaw Medical University, Wroclaw, Poland
2Department of Internal Medicine, Occupational Diseases, Hypertension and Oncology, Wroclaw Medical University, Wroclaw, Poland
3Department of Community Health Sciences, UCLA Fielding School of Public Health, Los Angeles, USA
1 Introduction
According to the World Health Organization (WHO),hypertension is the primary cause of premature mortality. It is estimated that 7.5 million people die annually due to hypertension complications. In the Polish population, the prevalence of hypertension is 29%, and increases in patients aged 65 and over.[1]
The increase in blood pressure (BP) at older ages is due to age-related vascular stiffness caused by the accumulation of calcium, smooth muscle hyperplasia in the arterial media,and the quantitative and qualitative alterations in vascular wall collagen. The most important factor in hypertension treatment in elderly patients is personalization. Avoidance of polypharmacy is another key aspect. In accordance with the European Society of Cardiology/European Society of Hypertension (ESC/ESH) guidelines, hypertensive treatment should be preceded by an in-depth analysis of global cardiovascular risk, while non- pharmacological treatment guidelines for elderly patients are the same as for younger age groups.[2]
The Hypertension in the Very Elderly Trial (HYVET)showed that hypertensive treatment is safe and effective in patients above 80 years of age, and that hypertensive treatment in patients above 90 years of age should be continued if previously effective and well-tolerated.[3,4]
The appropriate lifestyle changes are fundamental for preventing hypertension. They should not justify delaying the start of pharmacological treatment in high-risk patients.Appropriate lifestyle modifications can have a hypertensive effect comparable to that seen with single-agent pharma-cological treatment.[5]The primary problem in non-pharmacological treatment is poor patient adherence in the longterm. The older population with hypertension has been reported to have poorer BP control than younger populations.[6]Appropriate lifestyle changes may reduce BP in patients who are already treated pharmaceutically, which in turn allows for reducing the dosage of hypertensive drugs.[7]
The results of the Trial of Non-pharmacologic Interventions in the Elderly (TONE) indicate that in compliant patients, including the elderly, weight loss and sodium restriction bring about satisfactory decreases in BP.[8,9]The BP drop in response to sodium-restricted diet is particularly marked in the elderly, in diabetic patients, and in patients with chronic kidney disease.[10,11]
Adherence to treatment and consistent medication-taking are key factors in treatment effectiveness, especially in elderly patients. Patient adherence is affected by their involvement in the treatment process, their understanding of its goals, and their overall wellbeing in the process. Approximately 55% of the elderly do not comply with the prescribed treatment.[12,13]Doses are often omitted due to the adverse effects of treatment, financial considerations, age,concurrent diseases, and physical and cognitive impairment affecting vision, hearing, and strength (frailty).[14]
In recent years, frailty syndrome in elderly patients has been widely discussed. It affects 15%–20% of patients older than 60, and 30% of patients older than 80.[15]Frailty and cognitive impairment have been implicated as a causative and prognostic factor in patients with cardiovascular disease(CVD). Frailty syndrome is associated with worse perceived health, more comorbidities, and social isolation of the patient.[15]A few studies investigated the role of the geriatric syndrome in adherence to treatment, and the available studies discussed chronic diseases other than hypertension.[16,17]There is a discussion in the literature regarding the impact of age on adherence.[18-22]
The study aimed at identifying the relationship between frailty syndrome and adherence to pharmacological and nonpharmacological treatment, and at distinguishing the sociodemographic and clinical variables that can affect adherence to hypertensive treatment.
2 Methods
2.1 Patients
The study was performed between January and April 2015, at the general practitioners’ clinic which belongs to the Department of Internal Medicine, Occupational Diseases,Hypertension and Oncology of the Wroclaw University Hospital in Wrocław, Poland. The study was based on anonymous surveys. Participation was voluntary, and each respondent provided informed written consent. All patients were informed about the purpose and course of the study and of their right to withdraw from the study at any time.
During the period of the study, 207 patients over 65 years were fulfilling the criteria. However, after meticulous verification 114 patients were qualified to the study: 14 patients were excluded from the study due to exacerbation of the concomitant diseases, 26 patients refused, and 53 patients were not able to fill out the questionnaires even with the assistance Mini Mental State Examination (MMSE) < 27 points. Out of the group of 114 patients, 8 patients did not fill out their questionnaires properly, and 6 patients withdrew their informed consent. Finally, 100 patients were enrolled into the study. The study group included 100 patients (mean age 73.4 ± 7.5 years) diagnosed with hypertension, with a minimum time from diagnosis of five years, as recommended by the European Society of Hypertension(ESH) guidelines.[23]Another inclusion criterion was treatment with one or more hypertensive drugs. Exclusion criteria were: age under 65 years, severe cardiovascular complications or other severe comorbidities (hemodynamic instability, cancer, severe kidney failure, and dementia questionnaire MMSE result < 27). Patients were selected by a panel consisting of a physician and a nurse–specialist in the field of cardiac nursing. The sample group was homogeneous and suitable for statistical analysis.
2.2 Ethical consideration
The study was approved by the Bioethics Committee(approval No. KB 136/2015); all recruited patients provided their informed and voluntary consent to participate in the study.
2.3 Instruments
Three validated instruments were used: the Tilburg Frailty Indicator (TFI), the Health Behavior Inventory(HBI), and the 8-item Morisky Medication Adherence Scale(MMAS-8). The scales were distributed by a cardiac nurse within two days of admission at the Clinic. The patients answered the questions themselves.
Patient records were analyzed and interviews were conducted by a nurse to gather socio-demographic data (age,sex, education, marital status) and clinical parameters (ESC hypertension grade, comorbidities, time from diagnosis, BP monitoring, medication types and schedule, non- pharmacological treatment methods).
The definitions of both the geriatric syndrome spectrum and its components are constantly evolving and expanding.The present analysis included the components of the geriatric syndrome spectrum having a documented impact on prognosis, namely, frailty and polypharmacy.[11]
Frailty was assessed using the Tilburg Frailty Indicator(TFI),[24]adapted for use in Polish population, which comprises two parts.[25]The first part records socio-demographic characteristics (sex, age, marital status, country of origin,educational level, and monthly income) and potential contributors to frailty (lifestyle, comorbidities, life events, home environment). Part two of the TFI comprises 15 self-reported questions in three domains. The physical component(scored in total between 0 and 8 points) comprises 8 items related to physical health, unexplained weight loss, walking difficulties, balance issues, problems with hearing and eyesight, manual strength, and fatigue. The psychological component (scored between 0 and 4 points) consists of 4 questions regarding cognitive function, symptoms of depression and anxiety, and coping mechanisms. The social component(scored between 0 and 3 points) contains three items concerning living alone, social relationships, and social support.In the second part of the TFI, two response variants are offered in 11 questions (“yes” and “no”), and three response variants are offered in the remaining ones (“yes”, “no”,and “sometimes”). One point is given for “yes” and “sometimes” responses, and 0 points for “no” responses. The total score in the questionnaire ranges between 0 and 15, with higher scores indicating more severe frailty. TFI scores ≥ 5 indicate a diagnosis of frailty. In previous studies, TFI was proven valid and reliable for frailty assessment.[25]
The HBI, developed by Juczyński, comprises 24 items related to various health- related behaviors. Beneficial health-related behaviors and their degrees are assessed in four categories: (1) healthy eating habits, (2) preventive behaviors, (3) health practices, and (4) positive mental attitudes. The category of healthy eating habits includes eating whole meal bread, fruit, and vegetables, and avoiding salt,animal fats, sugar, and preservatives. Preventive behaviors comprise adherence to recommendations, regular medical follow-ups, and seeking health-related information. Health practices are behaviors related to sleep, exercise and leisure in daily life. The criteria for “positive mental attitudes”listed by the author include avoiding extreme emotions,stress, tension, and depressing situations. Patients complete the questionnaire by scoring each behavior using a five-item Likert scale indicating how often they engage in the behaviors (1: almost never, 2: rarely, 3: from time to time, 4: often,5: almost always). HBI scores range from 24 to 120 points.Higher scores indicate more self-reported engagement in the health-related behaviors. The raw total score is standardized using a Sten scale. The author suggested the following Sten ranges: Sten 1–4, low scores; Sten 5–6, moderate scores;and Sten 7–10, high scores. Separate results for each category of health behaviors are also calculated.[26]The internal consistency of the HBI, as indicated by Cronbach’s alpha,was 0.85 for the whole scale, and between 0.60 and 0.65 for each subscale separately. The test-retest correlation coefficient was 0.88. The HBI can be administered both to healthy and ill adults. Its uses include planning prevention and lifestyle interventions, as well as monitoring changes in health-related behaviors. Adherence to treatment was assessed using the self-reported MMAS-8. In a clinical setting,the MMAS-8 is easily administered, reliable and cost-effective. The purpose of the MMAS-8 is to help identify behaviors and barriers related to chronic medication adherence.It was found to be reliable and significantly correlated with BP control in hypertensive patients, and with hypertensive medication fill rates. MMAS-8 scores may range between 0 and 8, with scores of < 6, 6 to < 8, and 8 indicating low,medium, and high adherence, respectively.[27,28]Use of the MMAS©is protected by US and International copyright laws. Permission for use is required. A license agreement is available from Donald Morisky.
2.4 Data analysis
The survey results were recorded in an MS Excel spreadsheet, and then analyzed using the STATISTICA 10 software (StatSoft, Inc. Tulsa, USA). The statistical analysis involved the following operations: (1) for all measurable variables, both continuous (age, years from diagnosis) and discrete (TFI, HBI, and MMAS-8 scores), the basic descriptive statistics were calculated: means (M), standard deviations (SD), medians (Me), lower and upper quartiles (Q1and Q3), and minimum (Min) and maximum (Max) values. For nominal and ordinal variables, numbers (n) and percentages(%) were calculated. The significance of correlations between frailty syndrome and nominal variables was verified using the chi-squared test or Fisher’s exact test. The significance of correlations between frailty syndrome and continuous variables was verified using Student’st-test or the Mann-WhitneyU-test. The strength and direction of correlations between pairs of variables was determined using Spearman’s rank correlation coefficients (rho) and, in single-factor analysis, regression coefficients (b). For all statistical tests, the significance threshold ofP≤ 0.05 was used.
3 Results
The patients clinical data were shown in Table 1. Themean age of the respondents (53% of whom were female)was 73.4 ± 7.5 years. The mean frailty assessment (TFI)scores were: 7.61 ± 3.06 for the total, 3.91 ± 2.05 for the physical component, 2.29 ± 0.84 for the psychological component, and 1.41 ± 0.99 for the social component. Fifty three percents of the respondents were single, and 39% were unhappy with their home environment. The mean time from hypertension diagnosis was 12.4 ± 6.2 years, and most patients had grade I hypertension in accordance with the ESC criteria. The multimorbidity occurred in 83% of respondents.In 63.3% of the respondents, the polytherapy was applied in the treatment of hypertension.
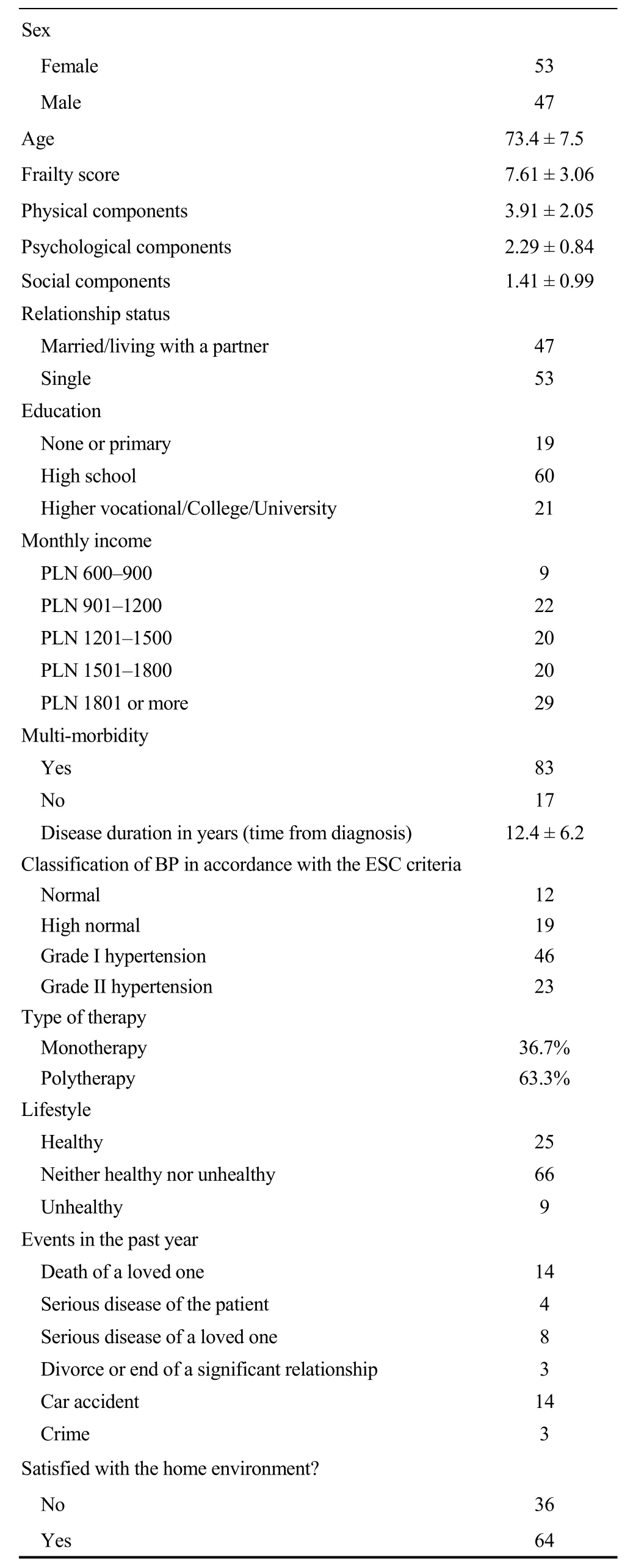
Table 1. Patients’ socio-demographic and clinical data.
3.1 Adherence levels (MMAS) and the degree of frailty
Table 2 shows the respondents’ clinical characteristics in relation to frailty. Frail patients (TFI ≥ 5) had a significantly longer time from hypertension diagnosis than non-frail patients (12.9 ± 6.4vs. 9.4 ± 4.0;P= 0.039). In the frail group,pharmacological adherence (MMAS-8) was significantly lower (4.1 ± 2.0vs.6.1 ± 2.1;P= 0.001), which means that frail patients show low adherence to pharmacological treatment for hypertension, while non-frail patients show moderate adherence.
Among the frail patients, as many as 77.9% obtained low adherence scores, and only 5.8% had high adherence to pharmacological treatment. Meanwhile, in the non-frail group,low adherence was found in 35.7% of patients, and high adherence was found in 28.6%. The differences between frail and non-frail patients in terms of adherence to treatment were statistically significant (P= 0.002) (Table 2).
3.2 Health behaviors and the degree of frailty
The analysis of respondents’ health behaviors revealed statistically significant differences between the studied patients in terms of the individual HBI domain scores depending on TFI results. Non-frail patients had higher scores in two out of four domains of the HBI: positive mental attitudes (3.6 ± 0.4vs.3.2 ± 0.5;P= 0.006) and health practices (3.6 ± 0.5vs.3.2 ± 0.5;P< 0.03); as well as higher global scores, both raw (83.3 ± 10.6vs.77.3 ± 9.5;P<0.031) and Sten (6.2 ± 1.6vs.5.2 ± 1.3;P= 0.017); Table 3.No differences were found for the “healthy eating habits”and “preventive behaviors” domains depending on frailty status (Table 2).
3.3 Correlations of socio-demographic and clinical characteristics with HBI and MMAS-8 scores
The impact of the analyzed socio-demographic and clinical characteristics was assessed by calculating Spearman’s rank correlation coefficients for the MMAS and HBI scores and the analyzed predictors. Table 4 shows theSpearman’s rank correlation coefficient values (rho) and significance levels (P).

Table 2. Respondents’ health-related behaviors as measured by the HBI and adherence level measured by MMAS-8 in groups differentiated by frailty status, as measured by the TFI questionnaire.
Single-factor analysis of the selected variables showed that pharmacological adherence as assessed using the MMAS-8 is significantly negatively affected by: age (rho =-0.441;P< 0.001); time from diagnosis (rho = -0.415;P<0.001); the physical (rho = -0.391;P< 0.001), psychological (rho = -0.386;P< 0.001), and social (rho = -0.363;P<0.001) TFI components; and the overall frailty score (rho =-0.486;P< 0.001). The correlation analysis showed a positive impact on pharmacological adherence for the following variables: living with a partner/spouse (rho = 0.292;P=0.004), education (rho = 0.392;P< 0.001), and net income(rho = 0.399;P< 0.001) (Table 3).

Table 3. Spearman’s rank correlation coefficients (rho) and their significance (P) for the analyzed predictors of adherence(MMAS-8) and health-related behaviors (HBI).
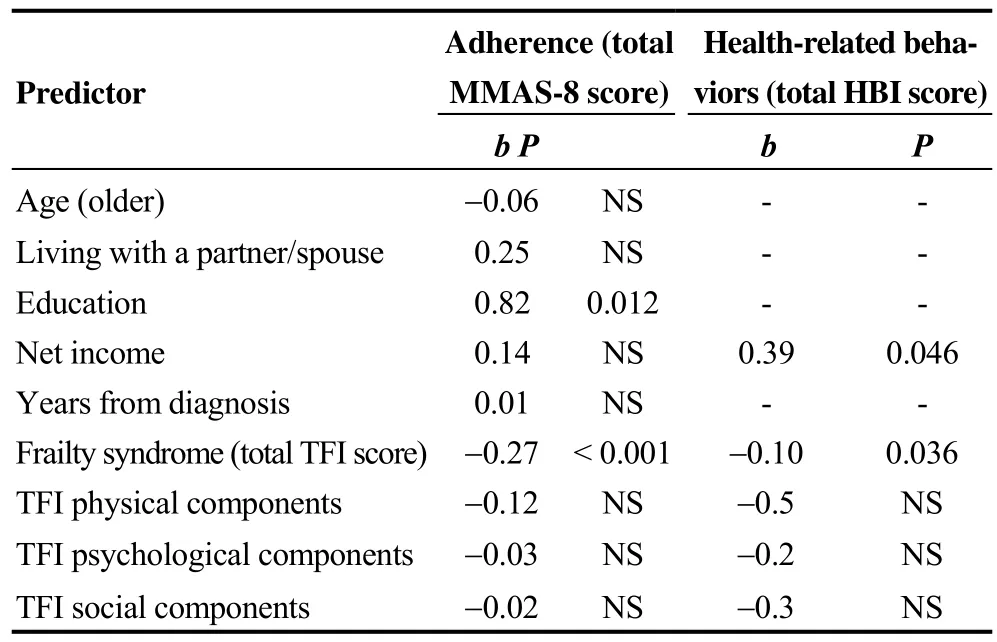
Table 4. Multiple regression coefficients (b) and their significance (P) for the analyzed predictors of adherence (MMAS-8)and health-related behaviors (HBI).
The analysis of correlations between the selected variables and the global HBI score revealed the strongest positive correlation with net income (rho = 0.372;P< 0.001),and a negative correlation with all the frailty components assessed by the TFI: social (rho = -0.307), physical (rho =-0.284), psychological (rho = -0.220), and the overall frailty score (rho = -0.365) (Table 3).
3.3 Determinants of HBI and MMAS-8 scores
Multiple regression analysis of all the factors identified as significant determinants of adherence and health-related behaviors in univariate analysis showed that education was the only determinant of better adherence as measured by the MMAS-8 (β = 0.82;P= 0.012), while net income was a positive determinant of health behaviors in the HBI (β =0.39;P= 0.046). The total TFI score indicating frailty was a statistically significant independent predictor of worse adherence to pharmacological treatment (β = -0.27;P< 0.001)and health behaviors (β = -0.10;P= 0.036) (Table 4).
The multiple-factor analysis yielded two models for estimating the MMAS-8 and HBI scores based on the total TFI score, as well as on education (for MMAS-8) or net income (for HBI). The models have a high statistical significance (P< 0.001). MMAS-8 = 4.8 + 0.82 × Education –0.27 × TFI.
F(2; 97) = 19.0;P< 0.001
HBI = 5.2 – 0.10 × TFI + 0.39 × Net income
F(2; 97) = 8.83;P< 0.001
4 Discussion
The identification of causes of non-adherence to pharmacological treatment is a key factor in planning therapeutic interventions aiming at increasing control, preventing complications, and improving long-term outcomes and any adverse effects of treatment. Precise identification of contributors to low medication adherence is crucial for improving treatment effectiveness and for distinguishing the patients in need of additional supervision in order to decrease the risk of complications from untreated hypertension.[14]
Diagnosis of frailty and of the associated difficulties in adhering to treatment allows for targeting the elderly patients with a poorer prognosis and at risk of complications from untreated or under-treated hypertension, and for planning interventions to improve hypertension control.[24,25]
In the present study, as many as 78% of frail patients failed to adhere to the pharmacological treatment of hypertension or to the recommended health behaviors. Frail patients had lower scores in the “positive mental attitudes” and“health practices” domains, as well as lower global scores in the Health Behavior Inventory, than non-frail patients. In multiple-factor analysis, frailty was an independent predictor of worse adherence to pharmacological treatment and to the recommended lifestyle changes.
Literature features conflicting reports on the relationship between frailty and adherence. A study of chronic dialysis patients by Chao,et al.[16]demonstrated, contrary to the present findings, significantly poorer medication adherence in non-frail patients, whereas Talegawkar,et al.[29]investigating the relationship between frailty and adherence to the Mediterranean diet, reported that non-frail patients showed better adherence to diet recommendations than frail patients.Similarly as reported by Jankowska,et al.,[30]higher severity of frailty among elderly patients may be considered a determinant of lower adherence. However, some publications report no correlation between frailty and adherence.[16,31,32]
Chao,et al.[16]links better adherence found in frail patients to their older age, stating that elderly patients pay more attention to their illness and symptoms, and are thus more compliant with the prescribed treatment plans. Other authors suggest that the differences in adherence between frail elderly patients and younger individuals can be associated with cognitive impairment and with the less accurate reporting of adherence by the elderly.[33]
In literature, there is also a discussion on the relationship between patient age and adherence. In the present study,older age (> 70 years) was a predictor of worse adherence to medication in hypertension. Similar results were reported by Karakut,et al.[34]and Jassim,et al.,[35]with patients above 70 years taking their medication less consistently than younger patients. In research by Jankowska-Polańska,et al.,[30]younger age was associated with better reported health behaviors in the “health practices” domain. Also Jackevicius,et al.[36]and Lam,et al.[37]report a correlation between younger age and better pharmacological adherence. Some publications, though, indicate older age as a predictor of better adherence to medication.[38-40]In elderly patients,factors decreasing adherence can also include multimorbidity and polypharmacy, adverse effects of treatment, unfulfilled expectations regarding treatment outcomes, and adverse drug interactions. Treatment outcomes do not always match patient expectations, which can result in discontinuation of the prescribed medication. A high pill burden is expectedly another important barrier to adherence, as a systematic review revealed that the prescribed number of daily doses and dosing frequencies are inversely associated with treatment and medication adherence.[41]Literature proves the benefits in terms of adherence brought about by decreasing the number of drugs prescribed. Patients taking a single pill or a single daily dose show better adherence.[20,42]
Duration of illness is another predictor of worse pharmacological adherence. This is another aspect where the present study contributes to the literature discussion. In single-factor analysis, longer duration of illness (time from diagnosis) was associated with worse pharmacological adherence. Meanwhile, in a study by Hyre,et al.,[43]lower adherence was correlated with durations of illness shorter than 10 years, and in a study by Lee,et al.,[22]shorter than five years. These author link the better adherence in patients who have lived with the disease longer to their better understanding of the illness, better relationship with the prescribing physician, and greater faith in their physician’s advice.[44]
In the single-factor analysis in the present study, significant stimulants of better pharmacological adherence included living with a partner/spouse, education, and net income. Better adherence to health behaviors was associated with net income only. Literature often describes the positive impact of social support on adherence.[30,45]Patients living in happy families also show better adherence than those with conflicted families. Marriage or living with a partner is reported as another factor improving adherence.[46]In the present study, single-factor analysis identified living with a partner/spouse as a statistically significant predictor of better pharmacological adherence. In a study by Marcum,et al.,[47]being single was an independent predictor of nonadherence.
In our multiple-factor analysis, net income indicating a good financial standing was a significant independent determinant of better adherence to lifestyle changes and health behavior recommendations. The WHO[48]emphasizes that in 15% of 167 investigated states, antihypertensive treatment is too expensive. In a study by Karakut,et al.,[34]patients with low incomes did not adhere to treatment, although income was not reported as an independent determinant of adherence. In Poland, pharmacological treatment costs are a significant challenge for hypertensive patients,which may cause them to disregard the recommended lifestyle changes, as seemingly less important. Alghuriar,et al.[49]state that financial barriers can be a problem in adherence, but are rarely investigated in studies.
4.1 Study limitations
This study has many limitations. The most important limitation is the fact that the study sample was very small and recruited from a single center. We plan to extend our research on this subject in the future. Another limitation is the fact that the level of adherence in our study was only measured using a direct method based on a self-reported questionnaire. The results were not verified by indirect methods, such as the use of physiological markers, pharmacy records or drug concentrations in bodily fluids for monitoring the treatment, which could be significant in elderly patient. The other limitation of this study was the lack of knowledge about the reasons of why the questionnaires were not filled out properly.
The analysis of treatment of chronic diseases other than hypertension, as well as possible polypharmacy, drug interactions, and side effects was not included, though these factors may also contribute to the level of adherence and severity of frailty among elderly patients with hypertension.
4.2 Conclusions
Frailty is associated with poor adherence to pharmacological treatment and health-related behaviors in hypertension. Frailty syndrome is a significant independent factor contributing to worse adherence to pharmaceutical and nonpharmacological treatment of hypertension. Better education significantly improves patients’ adherence to the prescribed pharmacological treatment, while a good financial standing evidenced by high net income is a determinant of better adherence to health-related behaviors recommended in hypertension treatment.
Acknowledgements
The MMAS (8-item) content, name, and trademarks are protected by US copyright and trademark laws. Permission for use of the scale and its coding is required. A license agreement is available from Donald E. Morisky, ScD, ScM,MSPH, 14725 NE 20th St Bellevue, WA 98007, USA;dmorisky@gmail.com. Professor Donald E Morisky receives honorarium from use of the MMAS-8 scales. The authors report no other conflicts of interest in this work. The authors declare that they have no competing interests.
References
1 Zdrojewski T, Bandosz P, Szpakowski P. The prevalence of major risk factors for cardiovascular disease in Poland. The results of the NATPOL-PLUS study.Kardiol Pol2004; 61(Supl. IV): S15–S17.
2 Mancia G., De Backer G., Dominiczak A,et al. 2007 Guidelines for the Management of Arterial Hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC).J Hypertens2007; 25:1105–1187.
3 Beckett NS, Peters R, Fletcher AE,et al. Treatment of hypertension in patients 80 years of age or older.N Engl J Med2008; 358: 1887–1898.
4 Grodzicki T. We treat hypertension in 80-year-olds, but cautiously? Comment on the results of the HYVET study.Kardiol Pol2008; 66: 7. 807.
5 Huisman M, Kunst AE, Mackenbach JP. Inequalities in the prevalence of smoking in the European Union: comparing education and income.Prev Med2005; 40: 756–764.
6 Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000.JAMA2003; 290: 199–206.
7 Frisoli TM, Schmieder RE, Grodzicki T,et al. Beyond salt:lifestyle modifications and blood pressure.Eur Heart J2011;32: 3081–3087.
8 Dickinson HO, Mason JM, Nicolson DJ,et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials.J Hypertens2006; 24:215–233.
9 Kostis JB, Espeland MA, Appel L. Does withdrawal of antihypertensive medication increase the risk of cardiovascular events? Trial of Nonpharmacologic Interventions in the Elderly (TONE) Cooperative Research Group.Amer J Cardiol1998; 82: 1501–1508.
10 He FJ, Markandu ND, MacGregor GA. Importance of the renin system for determining blood pressure fall with acute salt restriction in hypertensive and normotensive whites.Hypertension2001; 38: 321–325.
11 Kostis JB, Wilson AC, Shindler DM. Persistence of normotension after discontinuation of lifestyle intervention in the trial of TONE. Trial of Nonpharmacologic Interventions in the Elderly.Am J Hypertens2002; 15: 732–734.
12 Rajpura J, Nayak R. Medicationadherencein a sample ofelderlysuffering fromhypertension: evaluating the influence of illness perceptions, treatment beliefs, and illness burden.J Manag Care Pharm2014; 20: 58–65.
13 Ross S, Walker A, MacLeod MJ. Patient compliance in hypertension: role of illness perceptions and treatment beliefs.J Hum Hypertens2004; 18: 607–613.
14 Corrao G, Rea F, Ghirardi A,et al. Adherencewith antihypertensive drug therapy and the risk of heart failure in clinical practice.Hypertension2015; 66: 742–749.
15 Fried LP, Tangen CM, Walston J. Frailty in older adults: evidence for a phenotype.J Gerontol Biol Sci Med Sci2001; 56:M146–M157.
16 Chao CT, Huang JW; COGENT (COhort of GEriatric Nephrology in NTUH) study group. Geriatric syndromes are potential determinants of the medication adherence status in prevalent dialysis patients.Peer J2016; 14: e2122.
17 Jankowska-Polańska B, Lomper K, Alberska L,et al. Cognitive function and adherence to anticoagulation treatment in patients with atrial fibrillation.J Geriatr Cardiol2016; 13:559–565.
18 Burnier M. Medication adherence and persistence as the cornerstone of effective antihypertensive therapy.Am J Hypertens2006; 19: 1190–1196.
19 Krousel-Wood MA, Islam T, Webber LS,et al. New medication adherence scale versus pharmacy fill rates in seniors with hypertension.Am J Manag Care2009; 15: 59–66.
20 Kamran A, Sadeghieh Ahari S,et al. Determinants of patient’s adherence to hypertension medications: application of health belief model among rural patients. Ann Med Health Sci Res2014; 4: 922–927.
21 Irvin MR, Shimbo D, Mann DM,et al. Prevalence and correlates of low medication adherence in apparent treatment―resistant hypertension.J Clin Hypertens (Greenwich)2012; 14:694–700.
22 Lee GK, Wang HH, Liu KQ,et al. Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky Medication Adherence Scale.PLoS One2013; 8: e62775.
23 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH)and of the European Society of Cardiology (ESC).Eur Heart J2013; 34: 2159–2219.
24 Uchmanowicz I, Jankowska-Polańska B, Łoboz-Rudnicka M,et al. Cross-cultural adaptation and reliability testing of the Tilburg frailty indicator for optimizing care of polish patients with frailty syndrome.Clin Interv Aging2014; 9: 997–1001.
25 Gobbens RJ, van Assen MA, Luijkx KG, Schols JM. The predictive validity of the Tilburg frailty indicator: disability,health care utilization, and quality of life in a population at risk.Gerontologist2012; 52: 619–631.
26 Juczyński Z. Measurement instruments in the promotion and psychology of health.Polish Psychological Society; 2001:110–115; 162–167.
27 Morisky DE, Ang A, Krousel-Wood M,et al. Predictive validity of a medication adherence measure in an outpatient setting.J Clin Hypertens(Greenwich)2008; 10: 348–354.
28 Jankowska-Polanska B, Uchmanowicz I, Chudiak A. Psychometric properties of the Polish version of the eight-item Morisky Medication Adherence Scale in hypertensive adults.Patient Prefer Adherence2016; 10: 1759–1766.
29 TalegawkarSA, Bandinelli S, Bandeen-Roche K,et al. A higher adherence to a Mediterranean-style diet is inversely associated with the development of frailty in community-dwelling elderly men and women.J Nutr2012; 142: 2161–2166.
30 Jankowska-Polańska B, Dudek K, Szymanska-Chabowska A,Uchmanowicz I. The influence of frailty syndrome on medication adherence among elderly patients with hypertension.Clin Interv Aging2016; 11: 1781–1790.
31 Corsonello A, Pedone C, Lattanzio F, et al. Regimen complexity and medication nonadherence in elderly patients.Ther Clin Risk Manag2009; 5: 209–221.
32 Chudiak A, Jankowska-Polańska B, Uchmanowicz I. Effect of frailty syndrome on treatment compliance in older hypertensive patients.Clin Interv Aging2017; 12: 805–814.
33 Wu YH, Liu LK, Chen WT,et al. Cognitive function in individuals with physical frailty but without dementia or cognitive complaints: results from the I-lan longitudinal Aging Study.J Am Med Dir Assoc2015; 16: 899.e9–e16.
34 Karakurt P, Kaşikçi M. Factors affecting medication adherence in patients with hypertension.J Vasc Nurs2012; 30:118–126.
35 Jassim Al Khaja KA, Sequeira RP, Mathur VS. Rational pharmacotherapy of hypertension in the elderly: analysis of the choice and dosage of drugs.J Clin Pharm Therapeut2001;26: 33–42.
36 Jackevicius CA, Mamdani M, Tu JV. Adherence with statin therapy in elderly patients with and without acute coronary syndromes.JAMA2002; 288: 462–467.
37 Lam PW, Lum CM, Leung MF. Drug non-adherence and associated risk factors among Chinese geriatric patients in Hong Kong.Hong Kong Med J2007; 13: 284–292.
38 Kang M, Kim S, Yoon SJ,et al. Association between frailty and hypertension prevalence, treatment, and control in the elderly korean population.Sci Rep2017; 7: 7542.
39 Krousel-Wood M, Thomas S, Muntner P,et al. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients.Curr Opin Cardiol2004; 19: 357–362.
40 Carter BL, Foppe van Mil JW. Comparative effectiveness research: evaluating pharmacist interventions and strategies to improve medication adherence.Am J Hypertens2010; 23: 949–955.
41 Claxton AJ, Cramer J, Pierce C.A systematic review of the associations between dose regimens and medication compliance.Clin Ther2001; 23: 1296–1310.
42 Oliveira-FilhoAD, Barreto-Filho JA, Neves SJ, Lyra Junior DP. Association between the 8-item Morisky Medication Adherence Scale (MMAS-8) and blood pressure control.Arq Bras Cardiol2012; 99: 649–658.
43 HyreAD, Krousel-Wood MA, Muntner P,et al. Prevalence and predictors of poor antihypertensive medication adherence in an urban health clinic setting.J Clin Hypertens(Greenwich)2007; 9: 179–186.
44 Svensson S, Kjellgren KI, Ahlner J, Saljo R. Reasons for adherence with antihypertensive medication.Int J Cardiol2000;76: 157–163.
45 Scheurer D, Choudhry N, Swanton KA,et al. Association between different types of social support and medication adherence.Am J Manag Care2012; 18: e461–e467.
46 Morisky DE, DiMatteo MR. Improving the measurement of self-reported medication nonadherence: Final response.J Clin Epidem2011; 64: 258–263.
47 Marcum ZA, Zheng Y, Perera S,et al. Health ABC Study.Res Social Adm Pharm2013; 9: 817–827.
48 Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension.J Clin Hypertens(Greenwich) 2014; 16: 14–26.
49 Alghurair SA, Hughes CA, Simpson SH, Guirguis LM. A systematic review of patient self-reported barriers of adherence to antihypertensive medications using the world health organization multidimensional adherence model.J Clin Hypertens Greenwich2012; 14: 877–886.
 Journal of Geriatric Cardiology2018年2期
Journal of Geriatric Cardiology2018年2期
- Journal of Geriatric Cardiology的其它文章
- Thyrotoxicosis induced cardiogenic shock rescued by extracorporeal membrane oxygenation
- Intravascular ultrasound guided retrograde guidewire true lumen tracking technique for chronic total occlusion intervention
- Repetitive narrow QRS tachycardia in a 61-year-old female patient with recent palpitations
- Prediction of sudden death in elderly patients with heart failure
- Treatment of coronary in-stent restenosis: a systematic review
- Long term outcomes of drug-eluting stent versus coronary artery bypass grafting for left main coronary artery disease: a meta-analysis
