Long term outcomes of drug-eluting stent versus coronary artery bypass grafting for left main coronary artery disease: a meta-analysis
Kong-Yong CUI, Shu-Zheng LYU, Xian-Tao SONG, Fei YUAN, Feng XU, Min ZHANG,Ming-Duo ZHANG, Wei WANG, Dong-Feng ZHANG, Jing DAI, Jin-Fan TIAN, Yun-Lu WANG
1Department of Cardiology, Beijing Anzhen Hospital, Capital Medical University and Beijing Institute of Heart, Lung and Blood Vessel Diseases, Beijing, China
2Department of Anesthesiology, Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
1 Introduction
Significant unprotected left main coronary artery (ULMCA)disease occurs in 5%-7% of patients undergoing coronary angiography.[1,2]For several decades, coronary artery bypass graft surgery (CABG) has been recommended as the standard treatment for ULMCA disease owing to its survival benefit over medical therapy.[1,2]At the same time, the adaptation of drug-eluting stent (DES) in percutaneous coronary intervention (PCI) has led to a significant reduction in the risk of restenosis and repeat revascularization in comparison with bare-metal stent (BMS).[3,4]With the improvement of stent design, procedural technique and adjunctive medical therapy, PCI with DES is increasingly considered as a safe and feasible approach for patients with ULMCA disease.
Previous studies suggested the incidence of long-term death and overall safety endpoint of death, myocardial infarction (MI) or stroke were comparable between PCI and CABG for ULMCA disease.[5-7]In the current guidelines,PCI receives a class I or IIa recommendation for patients with low SYNTAX score, while a class IIa or IIb recommendation for patients with intermediate anatomic complexity.[1,2]Obviously, PCI with DES can be a viable alternative to CABG for ULMCA disease, especially in patients with low to intermediate anatomic complexity.
However, previous meta-analyses had a limited followup duration of ≤ 3 years, while the most recent meta-analysis concentrating on long-term outcomes comparing DES and CABG was restricted to a small sample size and studies using mixtures of BMS and DES were enrolled.[7,8]Recently,the EXCEL trial indicates that PCI with everolimus-eluting stents is noninferior to CABG with respect to the overall combined incidence of death, myocardial infarction (MI) or stroke at three years,[9]while the NOBLE study suggests CABG may be better than biolimus-eluting stent regarding lower rate of 5-year major adverse cardiac or cerebrovascular events (MACCE).[10]Unfortunately, it is still controversial whether DES is safe and effective compared to CABG for ULMCA disease at long-term follow up. We performed a meta-analysis including only trials with a follow-up duration of at least three years to examine the long-term relative safety and efficacy of DES and CABG for ULMCA lesions.
2 Methods
2.1 Search strategy
A comprehensive search of electronic database in Pub-Med, EMBASE, and Cochrane Library up to December 6,2016 was performed to identify the pertinent articles regarding DES versus CABG for ULMCA disease. The following medical subject headings and search terms were used: “percutaneous coronary intervention”, “PCI”, “stent”,“drug-eluting stent”, “DES”, “coronary artery bypass”, and“left main”. The references of the identified articles and relevant reviews were screened to include other potentially suitable trials.
2.2 Study selection
Studies satisfying the following criteria were eligible: (1)randomized controlled trials (RCTs) or adjusted observational studies (propensity-score matching > propensity-score adjusted > multivariable adjusted) regarding ULMCA disease; (2) compared DES to CABG; (3) followed for ≥ 3 years. Studies were excluded if they met any one of the following criteria: (1) not published in English; (2) published as an abstract or conference proceedings; (3) with the same patient sample; (4) using BMS exclusively or mixtures of BMS and DES without outcomes comparing DES with CABG separately. When several reports overlapped with each other, we selected the largest and the latest study. Two independent investigators (MDZ and WW) reviewed the studies to determine whether they met the inclusion criteria and any disagreement was resolved by consensus.
2.3 Data extraction
The following data was independently extracted by two authors (FX and MZ) through a standardized form: study characteristics, patient characteristics, and clinical outcomes.Hazard ratios (HR) of the time-to-event outcomes or odds ratios (OR) calculated from dichotomous outcomes were extracted. The primary endpoint was a composite of death,MI or stroke during the longest follow-up. Death, cardiac death, MI, stroke and repeat revascularization were the secondary outcomes, and they were defined variable in each study (Table 1S).
2.4 Quality assessment
The RCTs were evaluated by following the methodological criteria recommended by the Cochrane Collaboration: sequence generation, concealment of allocation, blinding, incomplete outcome data, selective outcome reporting, and other sources of bias,[11]whereas the observational studies were evaluated by the Newcastle-Ottawa Scale criteria.[12]
2.5 Statistical analysis
Quantitative analysis with the generic inverse variance random-effect model was performed to estimate the pooled HRs or ORs with their 95% confidence internals (CIs). Potential heterogeneity among studies was quantified withI2and a value of > 50% was defined as statistical heterogeneity. Furthermore, we used funnel plots to assess the potential publication bias.
Subgroup analysis was carried out to explore the sources of heterogeneity according to the study design (RCTs or adjusted observational studies). Additionally, sensitivity analysis was conducted by performing a separate analysis according to the following variables: (1) duration of follow up≥ 5 years; (2) SYNTAX score ≤ 32 or > 32. To demonstrate the robustness of the results, we investigated the influence of a single study on the overall effect by omitting one study in each turn. AllPvalues were two-sided, and results were considered statistically significant atP< 0.05.
This study was performed in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement,[13]and Meta-analysis Of Observational Studies in Epidemiology (MOOSE) checklist.[14]All statistical analysis was performed with Review Manager 5.1 (Cochrane Center, Denmark).
3 Results
3.1 Eligible studies
After a comprehensive search, 2103 potentially relevant articles were identified in the initial analysis. One hundred and nineteen articles were chosen for complete review, and finally, 16 studies were included in the present meta-analysis.[9,10,15-28]The process of selecting studies for the metaanalysis is briefly depicted in Figure 1 and the methodology as well as the population characteristics are presented in Table 1.
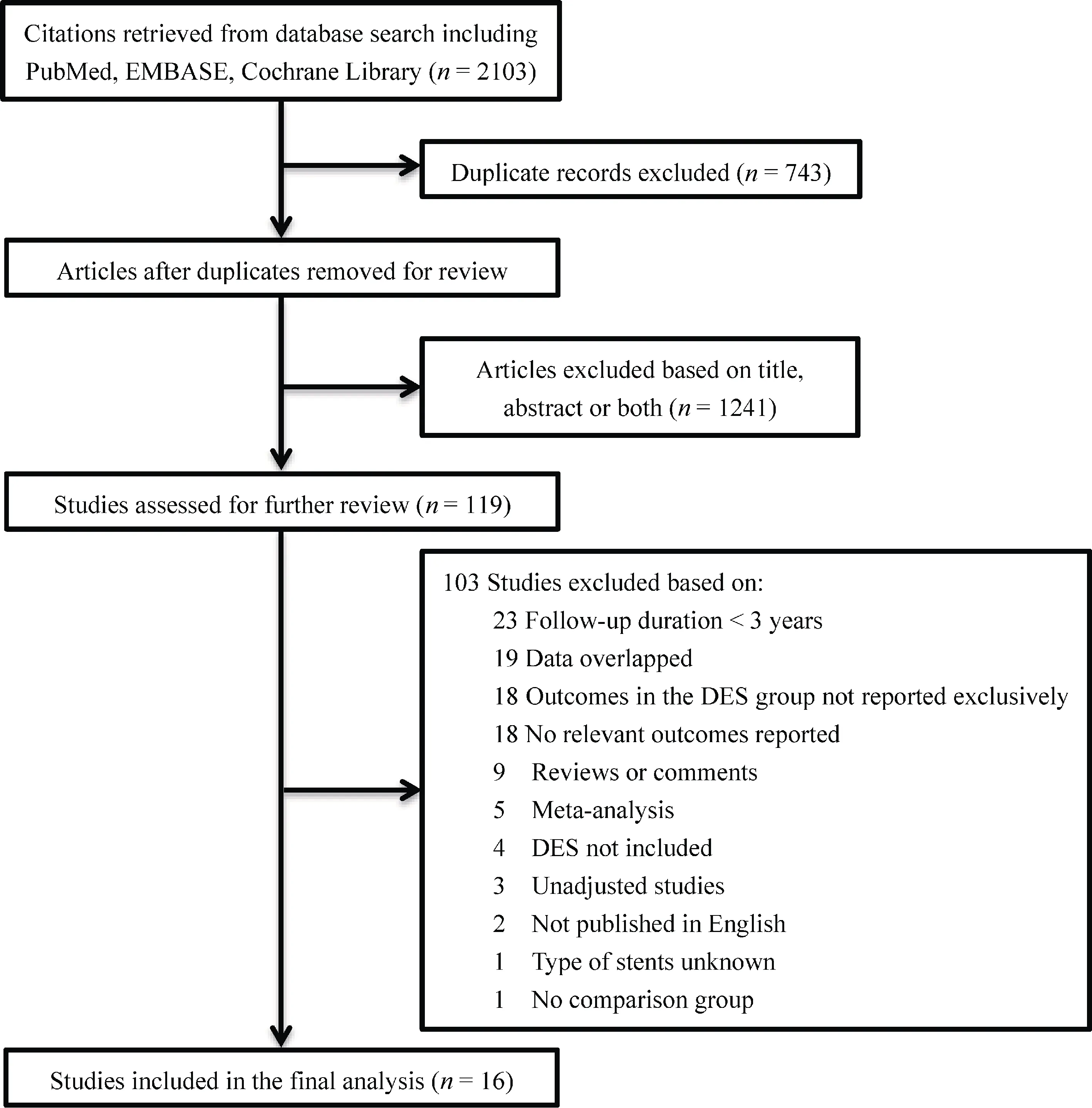
Figure 1. Process for study selection.
Among the 16 trials (four RCTs, six propensity-score matching studies, and six propensity-score adjusted studies),6333 and 7797 patients were treated with DES and CABG,respectively. Odds ratios were reported or calculated in two studies from dichotomous outcomes provided at five year follow-up.[17,26]Eligible studies were published between 2009 and 2016, while the clinical follow-up period ranged from 3 to 8 years. Quality assessment results are described in Table 2S and Table 3S. The funnel plot of the primary endpoint indicates that no publication bias was found(Figure 1S). Overall, intravascular ultrasound (IVUS)guided PCI was performed in 56.1% of the patients. Additionally, 47.6% of the patients underwent CABG with offpump technique, while a left anterior internal mammary artery graft was used in 92.5% of the patients who received CABG (Table 1).
3.2 Primary endpoint
In summary, the composite of death, MI or stroke was reported in 13 studies. Treatment with DES was comparable to that of CABG regarding the incidence of a composite of death, MI or stroke without heterogeneity for ULMCA disease (HR = 0.94, 95% CI: 0.86-1.03,P= 0.20,I2= 0)(Figure 2).
3.3 Secondary endpoints
There was no significant difference in the incidence of all-cause death (HR = 1.11; 95% CI: 0.92-1.32,P= 0.28)(Figure 3) as well as the risk of cardiac death (HR = 1.13,95% CI: 0.75-1.72,P= 0.55) (Figure 4) between the two strategies. Nevertheless, signs of statistical heterogeneity regarding cardiac death were found across trials (I2= 73%).Subgroup analysis by excluding observational studies showed the rate of cardiac death was comparable between the two groups without statistical heterogeneity (HR = 1.00, 95% CI:0.72-1.39,P= 0.99,I2= 21%).
Overall, the risk of MI was significantly higher in the DES group in comparison with the CABG group (HR =1.56, 95% CI: 1.09-2.22,P= 0.01,I2= 69%) (Figure 5).Subgroup analysis showed treatment with DES was associated with increased risk of MI in observational studies (HR= 1.67, 95% CI: 1.05-2.63,P= 0.03,I2= 56%), whereas no significant difference was found between the two groups in RCTs (HR = 1.48; 95% CI: 0.85-2.58,P= 0.17,I2= 67%).

Table 1. The methodology and the population characteristics of studies.

Figure 2. Forest plot of the composite of death, myocardial infarction or stroke. CABG: coronary artery bypass graft surgery; DES:drug-eluting stent.
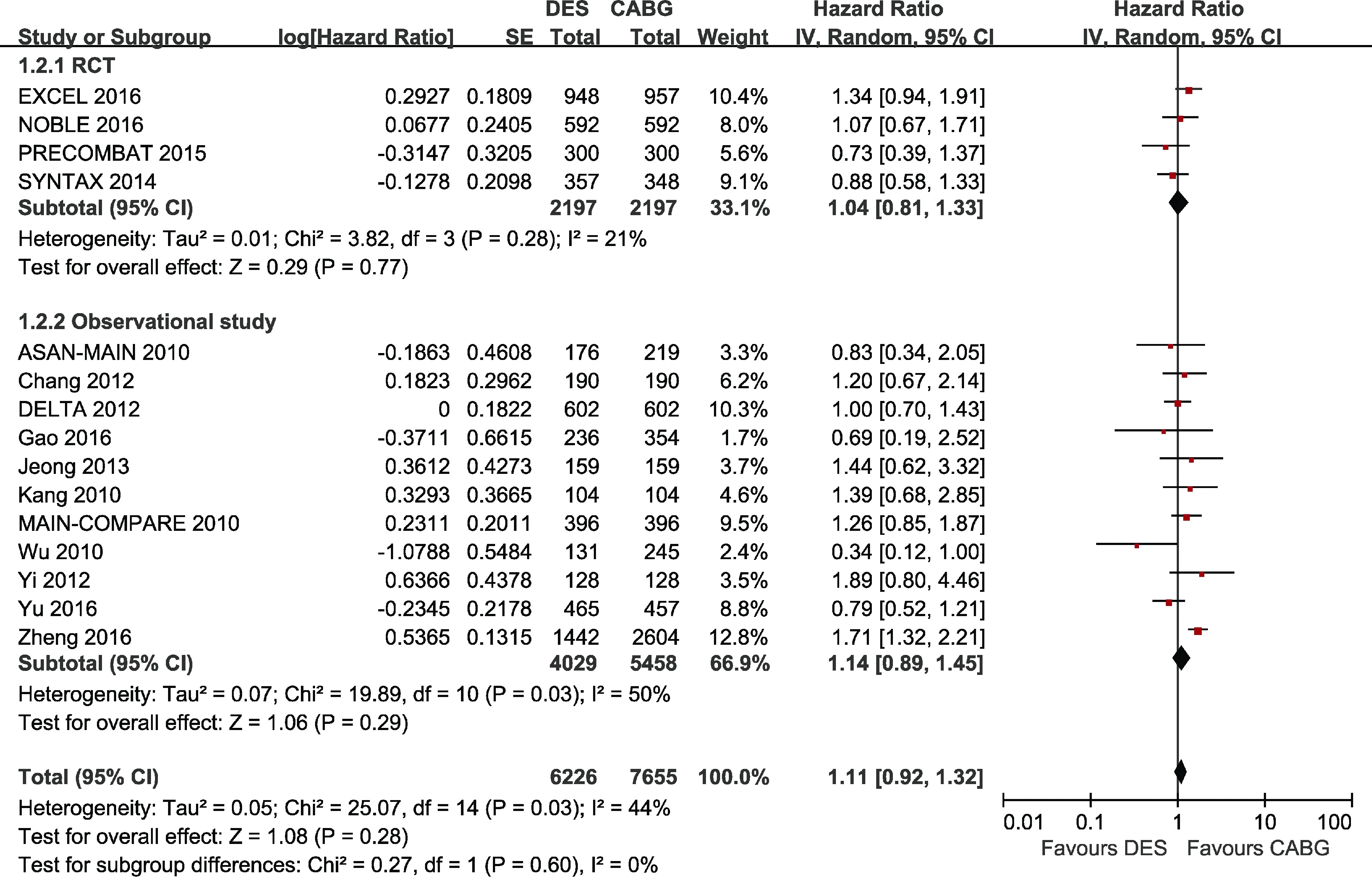
Figure 3. Forest plot of all-cause death. CABG: coronary artery bypass graft surgery; DES: drug-eluting stent.

Figure 4. Forest plot of cardiac death. CABG: coronary artery bypass graft surgery; DES: drug-eluting stent.

Figure 5. Forest plot of myocardial infarction. CABG: coronary artery bypass graft surgery; DES: drug-eluting stent.
In the pooled estimate, the risk of stroke was not significantly different between the two treatment strategies with statistical heterogeneity (HR = 0.61, 95% CI: 0.29-1.29,P= 0.20,I 2= 84%) (Figure 6). However, CABG was inferior to DES in terms of higher rate of stroke in observational studies (HR = 0.39, 95% CI: 0.17-0.91,P= 0.03,I2= 73%).
The data in Figure 7 indicated that the pooled HR of DES for repeat revascularization was significantly higher in the overall analysis (HR = 3.09, 95% CI: 2.33-4.10,P< 0.00001,I2= 79%), RCTs (HR = 1.70, 95% CI: 1.42-2.05,P<0.00001,I2= 0) and observational studies (HR = 3.92, 95%CI: 3.05-5.04,P< 0.00001,I2= 48%).
3.4 Sensitivity analysis
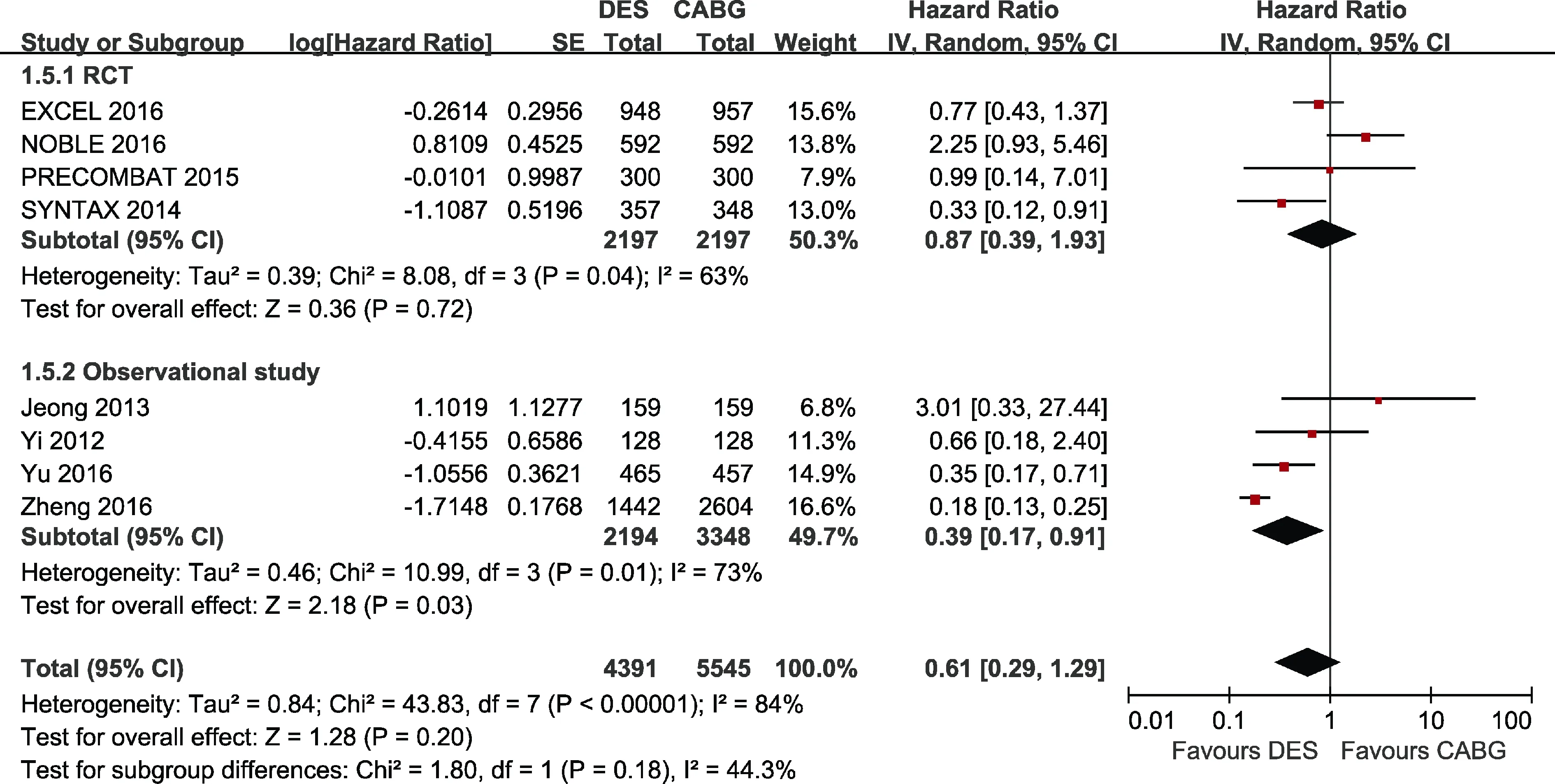
Figure 6. Forest plot of stroke. CABG: coronary artery bypass graft surgery; DES: drug-eluting stent.
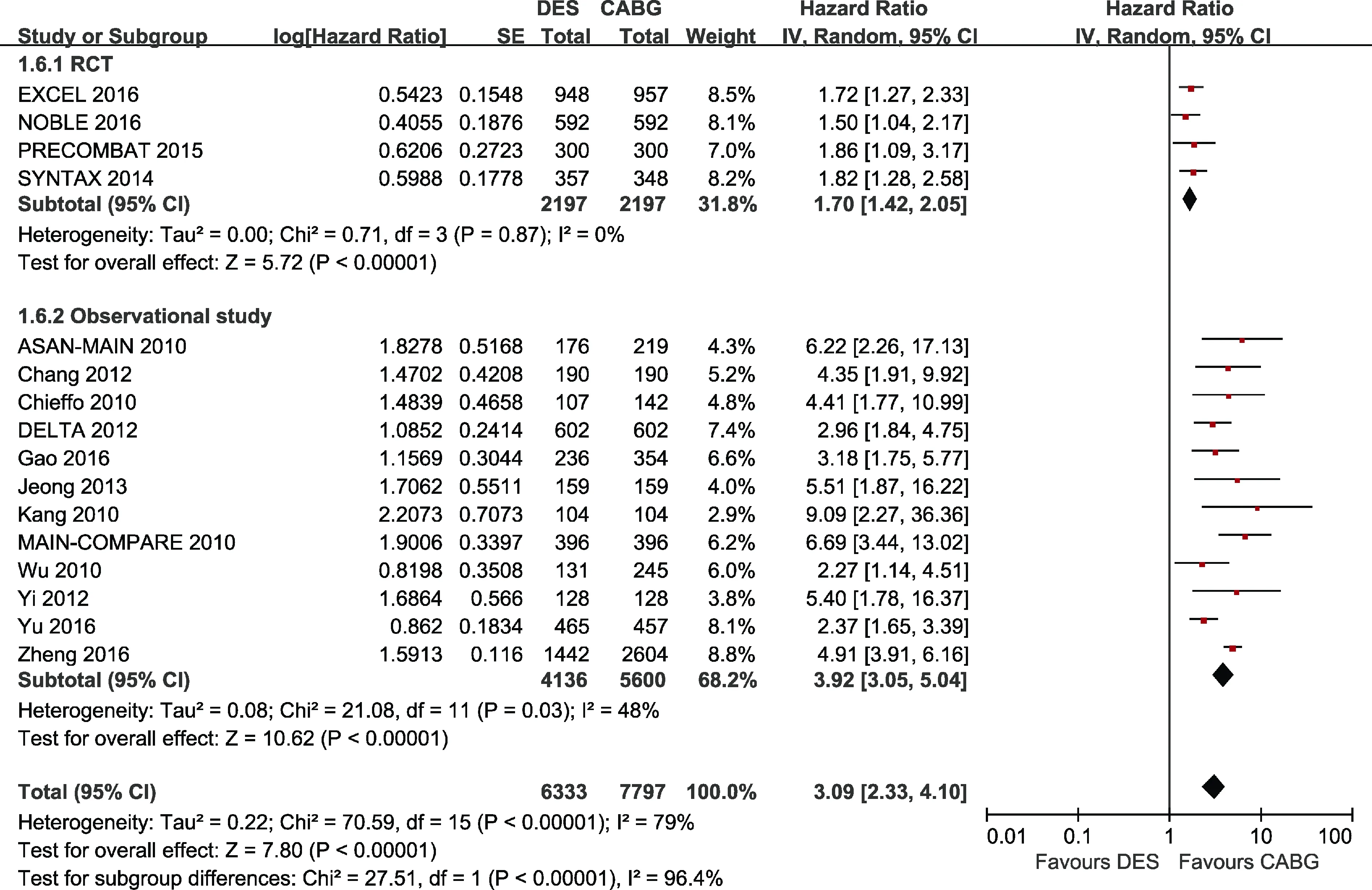
Figure 7. Forest plot of repeat revascularization. CABG: coronary artery bypass graft surgery; DES: drug-eluting stent.
Sensitivity analyses conducted through the removal of any single trial showed that it did not essentially affect the overall pooled estimate. Furthermore, when the study by Zheng,et al.[28]was removed, no statistical heterogeneity was found regarding cardiac death (HR = 0.99, 95% CI:0.74-1.32,P= 0.92,I2= 24%) (Data not shown), while statistical heterogeneity was not existed any more by excluding the EXCEL study[9]in terms of MI (HR = 1.78, 95% CI:1.33-2.37,P< 0.0001,I2= 33%) (Data not shown).
Besides, sensitivity analyses according to the follow-up duration (≥ 5 years) obtained mostly similar results compared to the overall analysis. Analysis after excluding the trials with follow-up duration < 5 years showed DES was associated with higher rate of MI compared with CABG without heterogeneity (HR= 1.92, 95% CI: 1.37-2.69,P=0.0002,I2= 0) (Figure S2).
In patients with SYNTAX score ≤ 32, DES was superior to CABG in terms of the composite of death, MI or stroke (HR = 0.80, 95% CI: 0.67-0.95,P= 0.01,I2= 0).Nevertheless, treatment with DES was inferior to CABG regarding the primary endpoint (HR = 1.45, 95% CI: 1.06-1.97,P= 0.02,I2= 42%) in patients with SYNTAX score >32 (Figure S3).
4 Discussion
The present meta-analysis with approximately 15,000 patients comparing the long-term safety and efficacy between DES and CABG for ULMCA disease demonstrated that: (1) PCI with DES was comparable to CABG regarding the rate of the primary endpoint compositing death, MI or stroke; (2) The incidence of MI and repeat revascularization were higher in the DES group compared with the CABG group, while no significant difference was found between the two treatment strategies regard as the risk of death, cardiac death and stroke; and (3) DES might be a safe and effective alternative to CABG for ULMCA disease with low to intermediate anatomic complexity.
Studies with small sample size demonstrated that no difference for the safety endpoint compositing death, MI or stroke between the two strategies for patients with ULMCA lesions.[7,8]Nevertheless, one study mixed BMS in the PCI group,[7]while the other enrolled study with outcomes at only 1 year follow-up,[8]therefore severe heterogeneity could not be avoided under the circumstances. In our study, the occurrence of the primary endpoint composite of death, MI or stroke in the DES group was comparable to the CABG group without heterogeneity.
All-cause mortality remained similar between the two strategies, which was in accordance with the studies with short-term data[5,6]and meta-analyses with long-term follow up.[7,8]Furthermore, we found that there was no difference between the two strategies regard as long-term cardiac mortality which was not reported in prior studies.
Previous meta-analyses concluded that the risk of MI was comparable between the two revascularization approaches,[5,7,8]whereas Athappan,et al.[6]reported that there was a trend in favor of CABG regard as the lower risk of MI at 1 year, 2 years and 3 years. Although with statistical heterogeneity, the occurrence of long-term MI also showed a trend towards a lower risk in patients received CAGB in the present study. Nonetheless, the result should be interpreted with caution as no difference was found in RCTs. The predominantly used first-generation DES and the insufficiency antiplatelet therapies may have contributed to this finding.Recently, Palmerini,et al.[29]has demonstrated that newergeneration DES, especially cobalt-chromium everolimuseluting stents, can reduce stent thrombosis as well as MI in comparison with first-generation DES. Therefore, the introduction of newer-generation DES and more potent antiplatelet therapies will likely reduce the occurrence of MI for patients received PCI.
In the current study, the long-term risk of stroke was reported to be comparable between the two groups which was consistent with other studies.[7,8]Nonetheless, the rate of stroke in the CABG group was reported to be significantly more frequent in adjusted observational studies. Notably,off-pump CABG could reduce the incidence of adverse neurological sequelae in contrast with cardiopulmonary bypass.[30]In addition, the lower incidence of dual antiplatelet therapy after revascularization with CABG might have resulted in this result. Overall, off-pump technique and dual antiplatelet therapy should be applied to reduce the risk of stroke for patients received CABG.
Over the past few years, CABG has improved the outcomes by the adaption of off-pump technique and arterial grafting. The internal mammary arteries have been widely used as the conduit to the left anterior descending coronary artery due to its long-term patency.[31]Interestingly, 92.5%of patients received a left internal mammary artery to left anterior descending coronary artery graft and complete artery grafting was performed in 53.6% of patients treated with CABG in our meta-analysis. Furthermore, the left internal mammary artery clearly exhibited less downstream coronary disease progression in the left anterior descending coronary artery compared with DES.[32]
First-generation DES was used in most of the studies,while it has been postulated that newer-generation DES with novel stent materials, platforms, as well as more biocompatible polymers could reduce the incidence of revascularization.[33]With the development of the stent design,the gap will be narrowed between the two strategies. Furthermore, it should be noted that routine angiographic follow-up was performed to detect early left main in-stent restenosis rather than clinically driven in most of the studies,which may cause higher rate of revascularization in the DES group. For patients treated with CABG, clinical symptoms may not occur with graft occlusion if the blood to left ventricle myocardium was partly supplied through the native vessel, which may underestimate the repeat revascularization discrepancy.
IVUS plays an important role in assessing lesion severity,selecting treatment strategy, optimizing stent implantation and subsequently obtaining better clinical and angiographic results.[34]Furthermore, previous studies have demonstrated intravascular ultrasound-guided DES implantation is associated with a greater benefit in patients with complex lesions such as bifurcations and ULMCA disease[35]in that it supplies beneficial effect on stent expansion in complex settings. Although optical coherence tomography with high resolution has emerged as an alternative imaging modality in suitable patients, it is challenging to create a blood-free environment for clear image especially in the left main ostium.[36]Fractional flow reserve is a well-established adjunct for assessing the physiological significance of stenosis.In clinical scenarios, these new interventional techniques should be given a full consideration when performing PCI with DES in ULMCA lesions.
Our meta-analysis presents a number of limitations that cannot be ignored. First, this study included both, RCTs and adjusted observational studies which can introduce a potential bias. Second, the definition of clinical endpoints slightly differed across the individual trials, although no signs of heterogeneity were observed for the primary endpoint. In fact, stratified analysis limited to more homogeneous subgroups of patients was performed and random effects model was used to account for the heterogeneity. Third, the duration of follow-up across trials was variable, and subset analysis (≥ 5 years) was performed. Fourth, different types of DES in the various trials had become an important source of heterogeneity. Although first-generation DES was predominantly applied, newer-generation DES was used in some lesions. Among the CABG strategies, the rates of left internal mammary artery to left anterior descending coronary artery graft adaption, complete artery grafting and cardiopulmonary bypass adaption were different across the studies. Fifth, subset analyses to evaluate the effect of SYNTAX score on clinical endpoints were performed in our study. Nevertheless, available data was scarce and incomplete reporting may result in underpowered analyses for certain outcomes.
In conclusion, the current meta-analysis shows that treatment with DES appears to be as safe as CABG for ULMCA disease at long-term follow up, although with higher risk of repeat revascularization. In addition, PCI with DES could be an alternative interventional strategy to CABG for ULMCA lesions with low to intermediate anatomic complexity. More large-scale RCTs with long-term outcomes are needed.
Acknowledgements
The study was funded by the Key Project in the National Science and Technology Pillar Program during the Twelfth 5-Year Plan Period of China, Beijing, China (2011BAI11B05)and Beijing Lab for Cardiovascular Precision Medicine,Beijing, China (PXM2017_014226_000037). The authors declare no commercial conflicts of interest.
References
1 Windecker S, Kolh P, Alfonso F,et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI).Eur Heart J2014; 35:2541–2619.
2 Fihn SD, Gardin JM, Abrams J,et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease:a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons.J Am Coll Cardiol2012; 60: e44–e164.
3 Kim YH, Park DW, Lee SW,et al. Long-term safety and effectiveness of unprotected left main coronary stenting with drug-eluting stents compared with bare-metal stents.Circulation2009; 120: 400–407.
4 Fokkema ML, James SK, Albertsson P,et al. Population trends in percutaneous coronary intervention: 20-year results from the SCAAR (Swedish Coronary Angiography and Angioplasty Registry).J Am Coll Cardiol2013; 61: 1222–1230.
5 Capodanno D, Stone GW, Morice MC,et al.Percutaneous coronary intervention versus coronary artery bypass graft surgery in left main coronary artery disease: a meta-analysis of randomized clinical data.J Am Coll Cardiol2011; 58:1426–1432.
6 Athappan G, Patvardhan E, Tuzcu ME,et al.Left main coronary artery stenosis: a meta-analysis of drug-eluting stents versus coronary artery bypass grafting.JACC Cardiovasc Interv2013; 6: 1219–1230.
7 Gargiulo G, Tamburino C, Capodanno D. Five-year outcomes of percutaneous coronary intervention versus coronary artery bypass graft surgery in patients with left main coronary artery disease: An updated meta-analysis of randomized trials and adjusted observational studies.Int J Cardiol2015; 195:79–81.
8 Nerlekar N, Ha FJ, Verma KP,et al.Percutaneous coronary intervention using drug-eluting stents versus coronary artery bypass grafting for unprotected left main coronary artery stenosis: a meta-analysis of randomized trials.Circ Cardiovasc Interv2016; 9: e004729.
9 Stone GW, Sabik JF, Serruys PW,et al. Everolimus-eluting stents or bypass surgery for left main coronary artery disease.N Engl J Med2016; 375: 2223–2235.
10 Makikallio T, Holm NR, Lindsay M,et al. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomised, open-label, non-inferiority trial.Lancet2016; 388: 2743–2752.
11 Lundh A, Gotzsche PC. Recommendations by Cochrane Review Groups for assessment of the risk of bias in studies.BMC Med ResMethodol2008; 8: 22.
12 Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses.Eur J Epidemiol2010; 25: 603–605.
13 Moher D, Liberati A, Tetzlaff J,et al.Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement.BMJ2009; 339: b2535.
14 Stroup DF, Berlin JA, Morton SC,et al.Meta-analysis of observational studies in epidemiology: a proposal for reporting.JAMA2000; 283: 2008–2012.
15 Park DW, Kim YH, Yun SC,et al. Long-term outcomes after stenting versus coronary artery bypass grafting for unprotected left main coronary artery disease: 10-year results of bare-metal stents and 5-year results of drug-eluting stents from the ASAN-MAIN (ASAN Medical Center-Left MAIN Revascularization) Registry.J Am Coll Cardiol2010; 56:1366–1375.
16 Chang K, Koh YS, Jeong SH,et al. Long-term outcomes of percutaneous coronary intervention versus coronary artery bypass grafting for unprotected left main coronary bifurcation disease in the drug-eluting stent era.Heart2012; 98: 799–805.
17 Chieffo A, Magni V, Latib A,et al. 5-year outcomes following percutaneous coronary intervention with drug-eluting stent implantation versus coronary artery bypass graft for unprotected left main coronary artery lesions the Milan experience.JACC Cardiovasc Interv2010; 3: 595–601.
18 Chieffo A, Meliga E, Latib A,et al. Drug-eluting stent for left main coronary artery disease. The DELTA registry: a multicenter registry evaluating percutaneous coronary intervention versus coronary artery bypass grafting for left main treatment.JACC Cardiovasc Interv2012; 5: 718–727.
19 Gao F, Zhou YJ, Wang ZJ,et al.Transradial coronary intervention versus coronary artery bypass grafting for unprotected left main and/or multivessel disease in patients with acute coronary syndrome.Angiology2016; 67: 83–88.
20 Jeong DS, Lee YT, Chung SR,et al.Revascularization in left main coronary artery disease: comparison of off-pump coronary artery bypass grafting vs percutaneous coronary intervention.Eur J Cardiothorac Surg2013; 44: 718–724.
21 Kang SH, Park KH, Choi DJ,et al.Coronary artery bypass grafting versus drug-eluting stent implantation for left main coronary artery disease (from a two-center registry).Am J Cardiol2010; 105: 343–351.
22 Park DW, Seung KB, Kim YH,et al. Long-term safety and efficacy of stenting versus coronary artery bypass grafting for unprotected left main coronary artery disease: 5-year results from the MAIN-COMPARE (Revascularization for Unprotected Left Main Coronary Artery Stenosis: Comparison of Percutaneous Coronary Angioplasty Versus Surgical Revascularization) registry.J Am Coll Cardiol2010; 56: 117–124.
23 Ahn JM, Roh JH, Kim YH,et al. Randomized Trial of stents versus bypass surgery for left main coronary artery disease:5-year outcomes of the PRECOMBAT study.J Am Coll Cardiol2015; 65: 2198–2206.
24 Morice MC, Serruys PW, Kappetein AP,et al. Five-year outcomes in patients with left main disease treated with either percutaneous coronary intervention or coronary artery bypass grafting in the synergy between percutaneous coronary intervention with taxus and cardiac surgery trial.Circulation2014;129: 2388–2394.
25 Wu X, Chen Y, Liu H,et al. Comparison of long-term(4-year) outcomes of patients with unprotected left main coronary artery narrowing treated with drug-eluting stents versus coronary-artery bypass grafting.Am J Cardiol2010;105: 1728–1734.
26 Yi G, Youn YN, Hong S,et al.Midterm outcome of off-pump bypass procedures versus drug-eluting stent for unprotected left main coronary artery disease.Ann Thorac Surg2012; 94:15–22.
27 Yu XP, Wu CY, Ren XJ,et al. Very Long-term outcomes and predictors of percutaneous coronary intervention with drugeluting stents versus coronary artery bypass grafting for patients with unprotected left main coronary artery disease.Chin Med J (Engl)2016; 129: 763–770.
28 Zheng Z, Xu B, Zhang H,et al. Coronary artery bypass graft surgery and percutaneous coronary interventions in patients with unprotected left main coronary artery disease.JACC Cardiovasc Interv2016; 9: 1102–1111.
29 Palmerini T, Benedetto U, Biondi-Zoccai G,et al. Long-term safety of drug-eluting and bare-metal stents: evidence from a comprehensive network meta-analysis.J Am Coll Cardiol2015; 65: 2496–2507.
30 Newman MF, Mathew JP, Grocott HP,et al.Central nervous system injury associated with cardiac surgery.Lancet2006;368: 694–703.
31 Tatoulis J, Buxton BF, Fuller JA. Patencies of 2127 arterial to coronary conduits over 15 years.Ann Thorac Surg2004; 77:93–101.
32 Zhang M, Guddeti RR, Matsuzawa Y,et al. Left internal mammary artery versus coronary stents: impact on downstream coronary stenoses and conduit patency.J Am Heart Assoc2016; 5: e003568.
33 Bangalore S, Toklu B, Amoroso N,et al.Bare metal stents,durable polymer drug eluting stents, and biodegradable polymer drug eluting stents for coronary artery disease: mixed treatment comparison meta-analysis.BMJ2013; 347: f6625.
34 Ahn JM, Kang SJ, Yoon SH,et al. Meta-analysis of outcomes after intravascular ultrasound-guided versus angiography-guided drug-eluting stent implantation in 26,503 patients enrolled in three randomized trials and 14 observational studies.Am J Cardiol2014; 113: 1338–1347.
35 De la Torre HJ, Baz AJ, Gomez HJ,et al. Clinical impact of intravascular ultrasound guidance in drug-eluting stent implantation for unprotected left main coronary disease: pooled analysis at the patient-level of 4 registries.JACC Cardiovasc Interv2014; 7: 244–254.
36 Fujino Y, Bezerra HG, Attizzani GF,et al. Frequency-domain optical coherence tomography assessment of unprotected left main coronary artery disease-a comparison with intravascular ultrasound.Catheter Cardiovasc Interv2013; 82: e173–e183.
 Journal of Geriatric Cardiology2018年2期
Journal of Geriatric Cardiology2018年2期
- Journal of Geriatric Cardiology的其它文章
- Comparison of the safety and efficacy of two types of drug-eluting balloons(RESTORE DEB and SeQuent® Please) in the treatment of coronary in-stent restenosis: study protocol for a randomized controlled trial (RESTORE ISR China)
- Comparison of in-hospital outcomes between octogenarians and nonagenarians undergoing transcatheter aortic valve replacement: a propensity matched analysis
- Patterns of in-hospital mortality and bleeding complications following PCI for very elderly patients: insights from the Dartmouth Dynamic Registry
- New predictors of in-stent restenosis in patients with diabetes mellitus undergoing percutaneous coronary intervention with drug-eluting stent
- Obstructive sleep apnea is associated with severity and long-term prognosis of acute coronary syndrome
- Adherence to pharmacological and non-pharmacological treatment of frail hypertensive patients
