针灸联合康复功能训练对周围性面瘫恢复的影响
林华俭 刘鸿
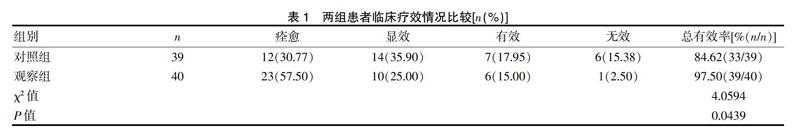
[摘要] 目的 評价针灸结合康复功能训练对周围性面瘫患者恢复的影响。 方法 选择我院2016年1月~2017年4月收治的周围性面瘫患者79例为研究对象,根据随机数字表法将奇数39例设为对照组,偶数40例设为观察组。对照组开展常规康复功能训练,观察组在对照组基础上开展针灸疗法,对两组患者进行随访6个月,对比两组患者恢复情况。 结果 疗效:对照组治疗总有效率为84.62%,观察组治疗总有效率为97.50%,组间比较差异有统计学意义(P<0.05);面神经功能评分:治疗前两组面神经功能评分比较差异无统计学意义(P>0.05),治疗后观察组评分明显优于对照组,差异有统计学意义(P<0.05),两组组内治疗前后比较差异均有统计学意义(P<0.05);生存质量评分:入院时两组患者生存质量评分比较差异无统计学意义(P>0.05),治疗结束后观察组优于对照组(P<0.05),随访6个月时观察组优于对照组(P<0.05),组内比较差异均有统计学意义(P<0.05)。结论 对周围性面瘫患者开展针灸联合康复功能训练能够显著提升治疗效果,改善面部神经功能,提升患者生存质量,值得临床应用与推广。
[关键词] 针灸;康复训练;周围性面瘫;神经功能
[中图分类号] R745.12 [文献标识码] B [文章编号] 1673-9701(2018)36-0110-04
[Abstract] Objective To evaluate the effect of acupuncture combined with rehabilitative functional training on the recovery of peripheral facial paralysis patients. Methods Seventy-nine patients with peripheral facial paralysis admitted to our hospital from January 2016 to April 2017 were enrolled in this study. According to the random number table method, the 39 patients of odd number were divided into the control group and the 40 cases of even number were divided into the observation group. The control group was given routine rehabilitative functional training. The observation group was given acupuncture in addition. The two groups were followed up for 6 months, and the recovery of the two groups was compared. Results Efficacy: The total effective rate of the control group was 84.62%, and the total effective rate of the observation group was 97.50%. There was statistically significant difference between the two groups (P<0.05). Facial nerve function score: There was no significant difference in facial nerve function score between the two groups before treatment(P>0.05), and the score of the observation group was significantly higher than that of the control group after treatment(P<0.05). There were statistically significant differences in the data before and after treatment in both groups (P<0.05). Quality of life score: There was no significant difference in quality of life score between the two groups at admission (P>0.05). The observation group was superior to the control group after treatment (P<0.05), and the observation group was superior to the control group at 6 months follow-up (P<0.05); the differences were statistically significant before and after the treatment(P<0.05). Conclusion Acupuncture combined rehabilitative functional training for patients with peripheral facial paralysis can significantly improve the treatment effect, the facial nerve function, and the quality of life of patients, and is worthy of clinical application and promotion.

