腹主动脉瘤开腹手术与腔内修复术的对照研究
朱锋 戈小虎
·论 著·(腹部血管外科和上消化道出血专题)
腹主动脉瘤开腹手术与腔内修复术的对照研究
朱锋 戈小虎
目的对比分析腹主动脉瘤病人开放手术与腔内修复术的治疗效果。方法收集新疆维吾尔自治区人民医院血管外科2012年7月至2017年6月收治的腹主动脉瘤病人,对比开放手术与腔内治疗病人的一般情况、住院情况、术后及随访期间并发症情况。结果176例接受手术的腹主动脉瘤病人均获成功,其中腔内修复术(endovascular aneurysm repair, EVAR)156例,开放手术(open surgery, OS)20例,平均年龄(68.8±9.9)岁,平均随访时间(25.9±16.2)个月。OS 组住院期间输注红细胞量、输注血浆量、术后重症监护室治疗时间、住院时间明显多于EVAR 组(P<0.05)。EVAR 术后髂支闭塞、支架感染等问题值得重视。结论尽管腔内治疗效果优于开放手术的循证资料十分有限,EVAR仍然是一个令血管外科医生及病人容易接受的手术方式。
腹主动脉瘤; 开放手术; 腔内修复术
腹主动脉瘤(abdominal aortic aneurysm)是腹主动脉局限性永久性扩张(大于正常主动脉管径的50%),年龄、性别、动脉粥样硬化、吸烟和高血压等均与其发病相关[1-2]。在美国,每年有15 000人死于腹主动脉瘤,破裂的死亡率高(80%~90%),围手术期的死亡率高(40%~50%)[3-5]。
早期的研究认为:腔内治疗早、中期效果优于开放手术。然而最近有研究报道:开放手术与腔内治疗5年、10年、15年的生存率无显著差异,并且腔内治疗术后再次干预的风险高于开放手术[6]。应对全球腹主动脉瘤发病率逐年增高的趋势,两种手术方式孰优孰劣,值得探讨。本中心收集近五年的腹主动脉瘤病人,做开放手术与腔内治疗的对比分析,旨在进一步提高腹主动脉瘤的诊疗水平,为今后的研究提供循证资料。
资料与方法
一、一般资料
研究为回顾性研究,收集新疆维吾尔自治区人民医院血管外科2012年7月至2017年6月收治的腹主动脉瘤病人。纳入标准:腹主动脉计算机断层血管造影(CTA)明确诊断的腹主动脉瘤病人,瘤体直径≥5.0 cm,满足手术标准且接受手术治疗。共纳入研究对象176例,其中男性140例、女性36例,平均年龄(68.8±9.9)岁,平均随访时间(25.9±16.2)个月。分组标准以手术方式决定:分为开放手术组157例与腔内手术组20例。两组病人一般情况差异均无统计学意义。(表1)
二、手术方法
1.腔内修复术(endovascular aneurysm repair, EVAR) 采用全身麻醉,术前30 min滴注抗生素,切开显露或穿刺双侧股动脉,静脉滴注普通肝素50 mg,术中造影定位,将支架输送系统送至预定点后再次放大图像造影确定定位是否准确,然后将支架近端释放在肾动脉下方。支架远端定位取决于髂动脉条件,如合并髂总动脉瘤或髂内动脉瘤,支架远端应放置在髂外动脉,否则尽量将髂支远端放置在髂总动脉。支架释放后,用球囊贴覆支架附着处,撤出超硬导丝,再次造影观察支架有无位移、内漏、髂支有无打折等。预先置入GORE 公司的Dryseal大口径的鞘管,在释放支架后拔出鞘管,收紧预置的血管缝合器,闭合穿刺点。
2.开放手术(open surgery, OS) 采用全身麻醉,取腹部正中切口,切口上端自剑突下缘,下端至脐下5~10 cm,全身肝素化,开腹后找到肾动脉下方的腹主动脉进行阻断,阻断位置为肾动脉开口下方正常动脉处,然后显露出瘤体及双侧髂动脉并阻断。将腹主动脉前壁切开,从瘤腔内缝扎腰动脉、肠系膜下动脉及骶中动脉开口,选择能够与病人相匹配的人工血管进行腹主动脉、双髂动脉的吻合。恢复血流后确定吻合口处无漏血,再以动脉瘤的囊壁缝合包裹植入的人工血管。逐层缝合后结束手术。
三、参考变量
记录病人的一般情况、住院情况、术后及随访期间并发症情况。
四、统计学方法

结 果
一、两组病人住院情况的对比分析
根据手术方式分组的病人住院情况对比分析见表2。OS组和EVAR组病人住院情况中输注红细胞量、输注血浆量、术后重症监护室(SICU)治疗时间、住院时间差异均有统计学意义。
二、两组病人术后及随访期间并发症的对比分析
根据手术方式分组的病人术后及随访期间并发症对比分析见表3。下肢深静脉血栓形成、脑血管疾病(脑梗死、脑出血)、心肌梗死、呼吸系统疾病(肺炎、急性呼吸窘迫综合征)、肾功能不全、髂支闭塞、支架感染发生率在OS组和EVAR组间差异均无统计学意义。
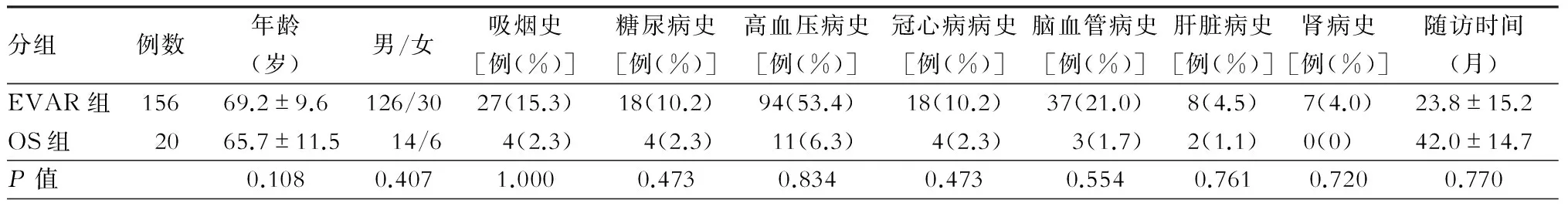
表1 两组病人基线特征

表2 两组病人住院情况对比分析±s)
注:SICU.外科重症监护室

表3 两组病人术后及随访期间并发症的对比分析[例(%)]
讨 论
腔内治疗因操作简单、近期效果好,已成为腹主动脉瘤的首选治疗。随着腔内技术的发展,开窗技术、“烟囱”技术、分支支架技术广泛得应用于解剖异常、病变累及分支动脉的腹主动脉瘤,开放手术已渐渐成为腔内治疗的替代方案[7]。早期的观点认为腔内治疗围手术期的效果优于开放手术,如30 d的死亡率、并发症发生率、住院时间。美国外科医师学会的国家手术质量改进项目(National Surgical Quality Improvement Project,NSQIP)统计,腔内治疗约占腹主动脉瘤择期手术的80%、急诊手术的59.8%[7]。开腹手术围手术期死亡率、并发症发生率在择期手术中是腔内治疗的4倍,在急诊手术中是腔内治疗的1.6~2倍,通过校正变量,主要的危险因素为:高龄、女性、肾功能不全、慢性阻塞性肺疾病等[8]。
本研究OS 组住院期间输注红细胞量、输注血浆量、术后重症监护室治疗时间、住院时间明显高于EVAR 组。对于输血量,腔内治疗相比开放手术创伤小,通常穿刺或局部切开,故出血的风险明显低于开放手术;对于术后重症监护室治疗时间、住院时间,开放手术创伤较大,手术时间长,导致手术应激反应大,全麻病人术后气管插管的拔管问题,术后通气、通便,术后并发症发生,全身恢复情况,往往增加了开放手术病人术后重症监护室治疗时间与住院时间;这与国外相关报告所提及得EVAR较OS在术后有更好的早期效果相似[9]。
有学者通过OS与EVAR的对比研究发现:EVAR术后病人心、脑、肺相关并发症的发生率明显低于OS组[6]。本研究OS组与EVAR组术后及随访期间并发症的发生率无明显差异,这或许与本实验将围手术期并发症与随访期间并发症合并在一起分析相关。有学者报道腔内治疗1年半后的远期效果与开放手术无显著差异(其中包括并发症)[8];相似的研究证实EVAR术后6年生存率(69%)无差异于开放修复(70%)。对于破裂腹主动脉瘤,Yildirim等[10]学者报告:腔内治疗与开放手术除术后重症监护室的天数差异具有统计学意义,其余数据均无统计学意义。腔内治疗在随机试验中未显示出比开放手术更好的长期结果,在EVAR术后5年内,有五分之一病人很有可能出现腔内治疗的相关并发症[11-12]。
Deery等[13]报告:EVAR术后再次干预的比例(0.3%)高于OS手术(0%),其中髂支闭塞的中位数高于OS组。Majd等[14]在对腹主动脉瘤10年的随访研究中发现:EVAR术后再次手术的比例(16.7%)明显高于OS组(6.5%),P=0.018,原因可能是内漏与髂支闭塞。本研究EVAR 组术后髂支闭塞病人明显高于OS组,但差异无统计学意义。原因一:近5年的回顾性研究中纳入的OS组病人较少,统计分析可能存在偏倚;原因二:本中心在2015年总结EVAR术后髂支闭塞的高危因素后,EVAR术中刻意规避了可控的危险因素,从而降低了髂支闭塞的发生。有报道:髂支闭塞是EVAR术后再次入院的第三大常见原因,值得重视[15-16]。髂支闭塞通常发生在术后3~6个月内,致病因素主要包括两类:第一类是解剖因素,第二类是设备因素。解剖因素包括:髂动脉直径较小(特别是女性病人)、动脉瘤角度≥60°、主动脉分叉处成锐角、髂动脉扭曲;设备因素包括:移植物移位,移植物直径较小、支架径向力低、支架连接处扭曲成角。传统的观点认为:主体支架的分支交叉可能会引起髂支闭塞,但Dattani等[17]学者通过研究证实:EVAR术中主体支架的分支交叉不会增加髂支闭塞的风险,但应当重视术后2型内漏的可能。虽然髂支闭塞在EVAR术后的发生率较高,但再次手术通过球囊扩张、血栓抽吸、支架植入、直接置管溶栓等腔内治疗的方法,通常能够达到预期效果[18-19]。
本研究EVAR 组术后支架感染病人明显高于OS组,但差异无统计学意义。然而,Dakour等[20]在腹主动脉瘤术后30 d的并发症中报道:EVAR术后血管移植物炎症和感染反应的相关并发症明显高于OS(6.7%比4.1%;P=0.01)。支架感染是腹主动脉瘤术后的罕见病,在文献中通常被称为Disastrous complications(灾难性的并发症),预后很差,值得重视[21]。支架感染较常见于EVAR术后,发生率相关系列报告为0.2%~0.9%,感染通常来源于术中无菌操作不严格所致的早期感染或术后阑尾炎、肾盂肾炎等感染蔓延所致的晚期感染[22]。本研究支架感染3例:其中1例拒绝手术,死于脓毒血症;1例自动出院,治疗情况不详;1例通过穿刺置管引流治愈,随访至今。穿刺引流应用于支架感染的治疗早在1990年就有学者提出,打破传统的开放手术,已渐渐应用于支架感染、感染性腹主动脉瘤[23]。由于支架感染的临床资料有限,且预后较差,术前完善的评估、围手术期抗生素的预防,术后定期复查CTA是十分必要的[22]。
内漏在EVAR术后的发生率高(10%~40%),其中最常见的是Ⅱ型内漏[24]。而开腹手术在直视下切开瘤腔、缝扎分支动脉、吻合血管,内漏的发生率很低[25]。美国血管外科学会(Society for Vascular Surgery,SVS)建议:如瘤腔持续增大,Ⅱ型内漏需进一步治疗[25]。欧洲血管外科学会(European Society for Vascular Surgery,ESVS)建议:Ⅱ型内漏可通过腔内或腹腔镜手术进一步处理,如未能成功,可考虑开放手术治疗(level 2b, recommendation B)[25]。早期的Ⅰ型内漏通常在术中可以检测到,无论是ⅠA型还是ⅠB型,均可通过腔内的方式解决;晚期的Ⅰ型内漏主要由于支架移位或主动脉瘤颈进行性扩张,因此术后密切的随访是必要的。Ⅲ、Ⅳ型内漏的发生率均小于2%,相关研究报告较少,但值得注意的是Ⅲ型内漏的出现是发生支架破裂的前兆,随访的目标之一就是对组件分离的诊断,以便能及时干预[26]。
腔内技术治疗腹主动脉瘤至今已有26年的历史,时间虽然短暂,但对血管外科领域有着重要的影响。尽管腔内治疗效果优于开放手术的循证资料十分有限,但EVAR仍然是一个令血管外科医生及病人容易接受的手术方式。
1 Sidloff DA,Saratzis A,Sweeting MJ,et al.Sex differences in mortality after abdominal aortic aneurysm repair in the UK.Br J Surg,2017,104:1656-1664.DOI:10.1002/bjs.10600.
2 Wang G,Zhai S,Li T,et al.Limb graft occlusion following endovascular aortic repair: Incidence, causes, treatment and prevention in a study cohort.ExpTher Med,2017,14:1763-1768.DOI:10.3892/etm.2017.4658.
3 张征,陈忠,吴章敏,等.腹主动脉瘤开放手术和腔内修复术的短期随访研究.心肺血管病杂志,2012,31:658-662.DOI: 10.3969/j.issn.1007-5062.2012.06.007.
4 谷涌泉,郭连瑞,齐立行,等.复杂腹主动脉瘤腔内修复65例经验.中国微创外科杂志,2016,16:224-227.DOI:10.3969 /j.issn.1009-6604.2016.03.009.
5 Ascoli MA,Pratesi G,Di Giulio L,et al.EVAR and OPEN treatment of abdominal aortic aneurysm: What is the role of MMP-9 in the follow-up?.J Med Vasc,2017,42:21-28.DOI:10.1016/j.jdmv.2017.01.004.
6 Patel R,Sweeting MJ,Powell JT,et al.Endovascular versus open repair of abdominal aortic aneurysm in 15-years' follow-up of the UK endovascular aneurysm repair trial 1 (EVAR trial 1): a randomised controlled trial.Lancet,2016,388:2366-2374.DOI: 10.1016/S0140-6736(16)31135-7.
7 Kalra K, Arya S. A comparative review of open and endovascular abdominal aortic aneurysm repairs in the national operative quality improvement database.Surgery,2017,162:979-988.DOI:10.1016/j.surg.2017.04.010.
8 Brahmbhatt R,Gander J,Duwayri Y,et al.Improved trends in patient survival and decreased major complications after emergency ruptured abdominal aortic aneurysm repair.J Vasc Surg,2016,63:39-47.DOI:10.1016/j.jvs.2015.08.050.
9 Powell JT,Sweeting MJ,Ulug P,et al.Meta-analysis of individual-patient data from EVAR-1, DREAM, OVER and ACE trials comparing outcomes of endovascular or open repair for abdominal aortic aneurysm over 5 years.Br J Surg,2017,104:166-178.DOI:10.1002/bjs.10430.
10Yildirim H,van Lammeren GW,Unlu C,et al.Long-term outcome and quality of life after ruptured abdominal aortic aneurysm repair. Vascular,2017:127378560.DOI:10.1177/1708538117727360.
11Karthikesalingam A,Vidal-Diez A,De Bruin JL,et al.International validation of a risk score for complications and reinterventions after endovascular aneurysm repair.Br J Surg,2015,102:509-515.DOI:10.1002/bjs.9758.
12Bahia SS,Holt PJ,Jackson D,et al.Systematic review and meta-analysis of long-term survival after elective infrarenal abdominal aortic aneurysm repair 1969-2011: 5 year survival remains poor despite advances in medical care and treatment strategies. Eur J Vasc Endovasc Surg,2015,50:320-330.DOI:10.1016/j.ejvs.2015.05.004.
13Deery SE,O’Donnell T,Bodewes T,et al. Early reintervention after open and endovascular abdominal aortic aneurysm repair is associated with high mortality.J Vasc Surg,2017,pii:S0741-5214(17)31894-3.DOI:10.1016/j.jvs.2017.06.104.
14Majd P,Ahmad W,Becker I,et al.Ten-year single-center results of abdominal aortic aneurysm treatment:endovascular versus open repair.Ann Vasc Surg,2017,44:113-118.DOI:10.1016/j.avsg.2017.05.008.
15Scali ST,Feezor RJ,Huber TS,et al.Acute bilateral renal artery chimney stent thrombosis after endovascular repair of a juxtarenal abdominal aortic aneurysm.J Vasc Surg,2015,61:1058-1061.DOI:10.1016/j.jvs.2013.10.037.
16Lim S,Halandras PM,Park T,et al.Outcomes of endovascular abdominal aortic aneurysm repair in high-risk patients.J Vasc Surg,2015,61:862-868.DOI:10.1016/j.jvs.2014.11.081.
17Dattani N,Wild J,Sidloff D,et al.Outcomes following limb crossing in endovascular aneurysm repairs.Vasc Endovascular Surg,2015,49:52-57.DOI:10.1177/1538574415587512.
18Wang Y,Joannic D,Delassus P,et al.Comparison of the strain field of abdominal aortic aneurysm measured by magnetic resonance imaging and stereovision:a feasibility study for prediction of the risk of rupture of aortic abdominal aneurysm.J Biomech,2015,48:1158-1164.DOI:10.1016/j.jbiomech.2015.01.017.
19Tornqvist P,Dias N,Sonesson B,et al.Intra-operative cone beam computed tomography can help avoid reinterventions and reduce CT follow up after infrarenal EVAR.Eur J Vasc Endovasc Surg,2015,49:390-395.DOI:10.1016/j.ejvs.2015.01.009.
20Dakour AH,Locham S,Nejim B,et al.Indications, risk factors, and outcomes of 30-day readmission after infrarenal abdominal aneurysm repair.J Vasc Surg,2017,pii:S0741-5214(17)31930-4.DOI:10.1016/j.jvs.2017.07.106.
21Argyriou C,Georgiadis GS,Lazarides MK,et al.Endograft infection after endovascular abdominal aortic aneurysm repair:A systematic review and meta-analysis.J Endovasc Ther,2017,24:688-697.DOI:10.1177/1526602817722018.
22Montelione N,Menna D,Sirignano P,et al.Open conversion after aortic endograft infection caused by colistin-resistant, carbapenemase-producing klebsiellapneumoniae.Tex Heart Inst J,2016,43:453-457.DOI:10.14503/THIJ-15-5265
23Chino S,Kato N,Noda Y,et al.Treatment of infected aneurysms of the abdominal aorta and iliac artery with endovascular aneurysm repair and percutaneous drainage. Ann Vasc Surg,2016,36:211-289.DOI: 10.1016/j.avsg.2016.02.026.
24Quinn AA,Mehta M,Teymouri MJ,et al. The incidence and fate of endoleaks vary between ruptured and elective endovascular abdominal aortic aneurysm repair. J Vasc Surg,2017,65:1617-1624.DOI: 10.1016/j.jvs.2016.10.092.
25Moulakakis KG,Klonaris C,Kakisis J,et al. Treatment of type II endoleak and aneurysm expansion after EVAR. Ann Vasc Surg,2017,39:56-66. DOI: 10.1016/j.avsg.2016.08.029.
26Li J,Tian X,Wang Z,et al.Influence of endoleak positions on the pressure shielding ability of stent-graft after endovascular aneurysm repair (EVAR) of abdominal aortic aneurysm (AAA). Biomed Eng Online,2016,15:135.DOI: 10.1186/s12938-016-0249-z.
Comparisonofopensurgerywithendovasculartreatmentforabdominalaorticaneurysms
ZhuFeng,GeXiaohu.
DepartmentofVascularSurgery,XinjiangUygurAutonomousRegionPeople’sHospital,Wurumuqi830001,China
GeXiaohu,Email:gexiaohu_xj@163.com
ObjectiveTo comparatively analyze open surgery with endovascular treatment for abdominal aortic aneurysms.MethodsThe patients with abdominal aortic aneurysms were collected from July 2012 to June 2017 in the Department of Vascular Surgery, Xinjiang Autonomous RegionPeople'sHospital.The general condition, hospitalization andcomplications postoperation and during the follow-up period were compared between open surgery and endovascular treatment.ResultsOf 176 patients with abdominal aortic aneurysms successfully undergoing surgical operations, 26 patients were treated with endovascular therapy (EVAR) and 20 patients were treated with open surgery(OS). Of all patients, the mean age was 68.8±9.9 years, and the mean follow-up period was 25.9±16.2 months. The infusion of erythrocytes and the amount of infusion in the OS group were significantly increased as compared with those in the EVAR group (P<0.05). Theattention should be paid to iliac artery occlusion and stent infection following EVAR.ConclusionsWhether the efficacy of endovascular treatment is superior to open surgery is unclear,but EVAR is an accepted surgical procedure for vascular surgeons and patients.Early effect of endovascular treatment may be better than open surgery during hospitalization,and the long-term effect should be studied further.
Abdominal aortic aneurysm; Open surgery; Endovascular treatment
R654.3
A
10.3969/j.issn.1003-5591.2017.06.006
830001 乌鲁木齐,新疆维吾尔自治区人民医院血管外科
戈小虎,Email:gexiaohu_xj@163.com
2017-10-09)