Complete pathologic response after chemoradiotherapy in a patient with rectal squamous cell carcinoma: a case report
Zaied Sonia, Daldoul Amira, Bhiri Hanene, Ammar Nouha, Khechine Wiem, Toumi Omar, Abbes Ibtissem,Ben Salem Amina, Njima Manel, Mhabrech HoudaDepartment of Medical Oncology, Fattouma Bourguiba University Hospital of Monastir, Monastir 5000, Tunisia;Department of Surgery, Fattouma Bourguiba University Hospital of Monastir, Monastir 5000, Tunisia; Department of Radiology, El Omrane University Hospital of Monastir, Monastir 5000, Tunisia; Department of Pathological Anatomy,Fattouma Bourguiba University Hospital of Monastir, Monastir 5000, Tunisia
CASE REPORT
Complete pathologic response after chemoradiotherapy in a patient with rectal squamous cell carcinoma: a case report
Zaied Sonia1, Daldoul Amira1, Bhiri Hanene1, Ammar Nouha1, Khechine Wiem1, Toumi Omar2, Abbes Ibtissem1,Ben Salem Amina3, Njima Manel4, Mhabrech Houda31Department of Medical Oncology, Fattouma Bourguiba University Hospital of Monastir, Monastir 5000, Tunisia;2Department of Surgery, Fattouma Bourguiba University Hospital of Monastir, Monastir 5000, Tunisia;3Department of Radiology, El Omrane University Hospital of Monastir, Monastir 5000, Tunisia;4Department of Pathological Anatomy,Fattouma Bourguiba University Hospital of Monastir, Monastir 5000, Tunisia
Squamous cell carcinoma (SCC) of the rectum is a rare disease. A 59-year-old man presented with SCC of the middle rectum located 10 cm from the anus. The stage of the tumor was revealed to be T3N+M0. The patient
a combined treatment with cisplatin and fluorouracil in concomitance with external radiation therapy. He then underwent an anterior resection of the rectum. The postoperative histopathological findings classified the tumor as ypT0N0 with cancer-free margins and lymph nodes.Treatment of SCC remains very challenging, and the acquisition of more consistent data is needed.
Squamous cell carcinoma; rectal neoplasm; surgery; colonoscopy
Introduction
Squamous cell carcinoma (SCC) of the rectum is a rare disease. Its incidence is estimated to be around 0.1 to 0.25 per 1000 colorectal neoplasms1-3. It appears to be associated with chronic inflammatory conditions and infections. Its presentation is nonspecific and patients tend to present with advanced stage disease. Distinction from SCC of the anus can be difficult, but can be facilitated by immunohistochemical staining for cytokeratins4. Knowledge is lacking about its etiology, prognosis, and optimal treatment. The literature is represented essentially by case reports and short series4.
Case report
A 59-year-old man presented with a history of pelvic discomfort and constipation for about 6 months. The patient did not present with a family history of colonic malignancy.A digital rectal examination revealed a mass about 8 cm fromthe anal margin on the right lateral wall of the middle rectum. Colonoscopy revealed an ulcerated, polypoid tumor of the middle rectum located 10 cm from the anus. Biopsies indicated a SCC (Figures 1, 2 and 3).
Magnetic resonance imaging (MRI) of the rectum confirmed the results of colonoscopy and revealed adenomegalia in the pelvis (Figure 4).
The computed tomography (CT) scan demonstrated the absence of distal metastases. The stage of the tumor was found to be T3N+M0.
The case was discussed by the multidisciplinary oncological team who decided that concomitant chemotherapy and radiation therapy followed by surgical excision should be performed. The patient received a combined treatment with cisplatin and fluorouracil (5FU) in concomitance with external radiation therapy. He received 45 Gy with two sessions of chemotherapy (Figure 5).
Then, he underwent an anterior resection of the rectum.The standard technique of mesorectal excision and the concept of sphincter-preserving surgery were achieved.
The postoperative histopathological findings classified the tumor as ypT0N0 with cancer-free margins and lymph nodes(Figure 6).
The postoperative period was uneventful.

Figure 1 Carcinomatous proliferation with organized squamous differentiation (H&E staining, 40×).
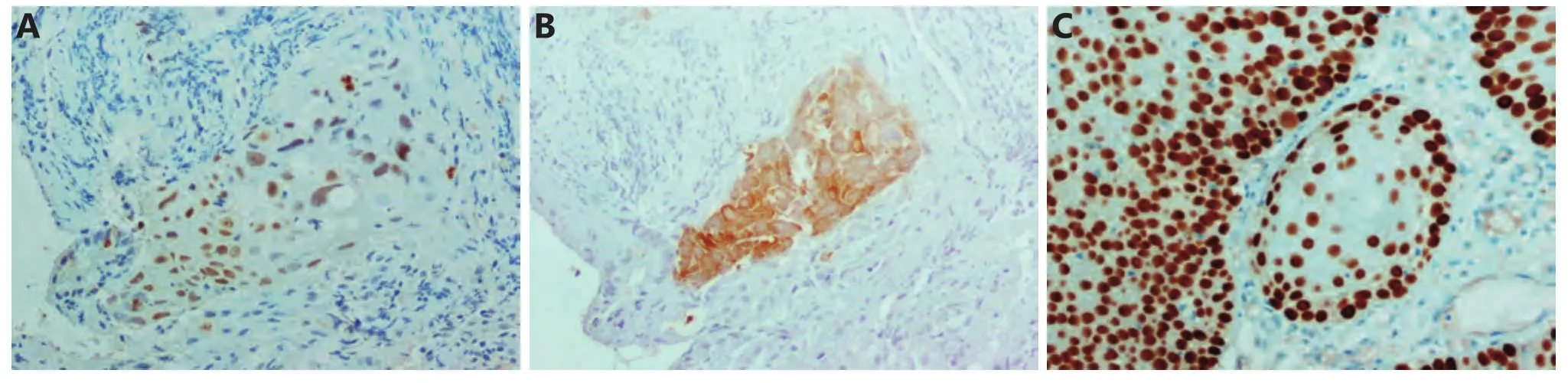
Figure 3 Immunohistochemistry: (A) Nuclear positivity for p63 (IHC staining, 200×). (B) Cytoplasmic positivity for CK5/6 and negativity for CK20 and CDX2. (C) Nuclear positivity for p40.
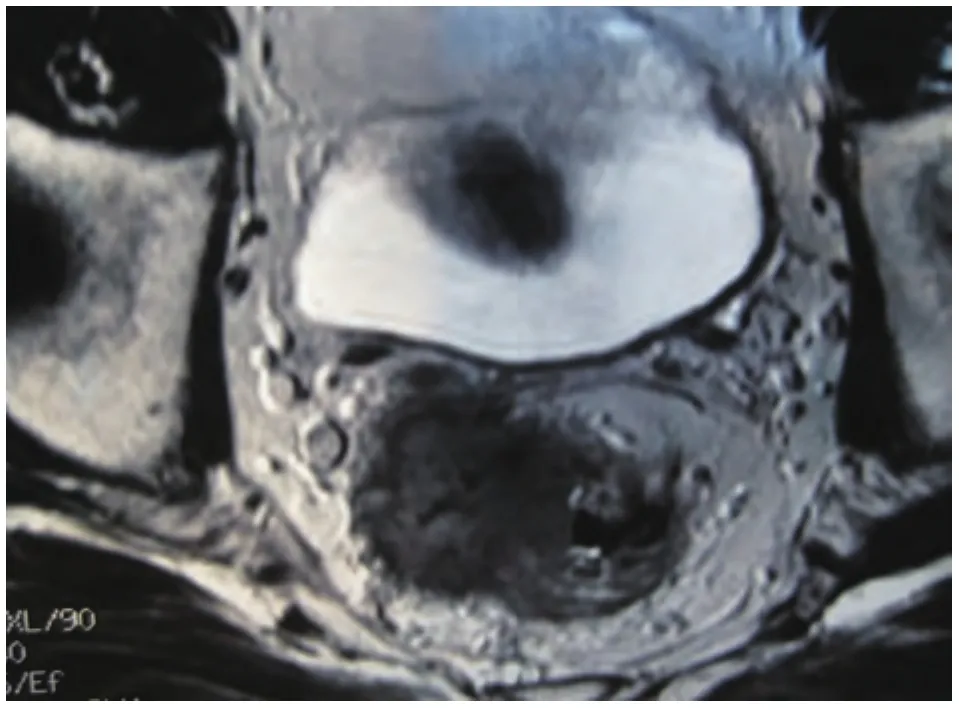
Figure 4 Magnetic resonance imaging before chemoradiotherapy.
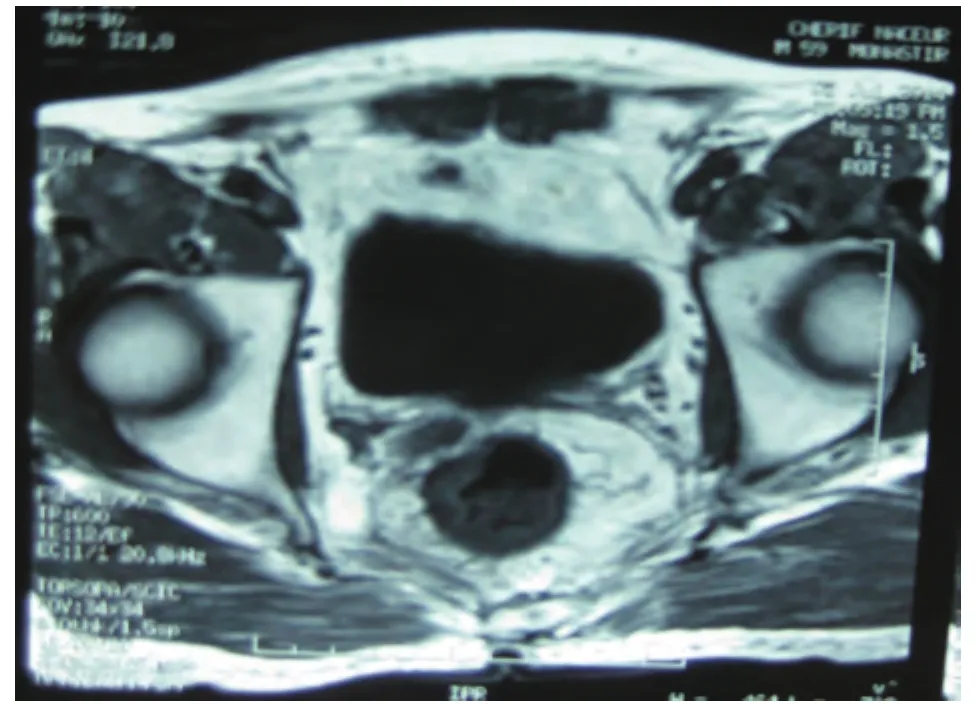
Figure 5 Magnetic resonance imaging after chemoradiotherapy.
Discussion
Colorectal SCC is a rare disease. The incidence of the disease is approximately 0.10 to 0.25 per 1000 colorectal cancers1-3and the first case of SCC of the rectum was described by Raiford in 19335. We have little knowledge about its etiology,prognosis, and optimal treatment.

Figure 6 Complete pathologic response after neoadjuvant chemoradiotherapy (H&E staining, 40×).
SCC of the rectum appears to affect women more than men between the ages of 39 and 93 years, with a mean age of 57 years. In the literature, 66% of cases occur in women and 34% in men6.
Regarding the pathophysiology of the disease, four hypotheses have been developed over the years.
Some suggest that chronic irritation may be caused by radiation exposure that can cause squamous metaplasia7,8, or by colitic infections due to Entamoeba histolytica and schistosomiasis9-11. Ouban et al.12suggested that pluripotent stem cells have the ability of squamous differentiation.
While some authors have described the possibility of squamous differentiation in adenoma and adenocarcinoma13,others have reported some case reports of rectal SCC in association with prostate, ovarian, and endometrial cancers10,13.
The association between human papilloma virus (HPV)and SCC of the anus has been clearly established with the most common subclasses of pathogenic viruses, including HPV-16, -18, -31, and -3314. However, the relation between HPV and rectal SCC has not yet been established11,15,16.
Symptoms of SCC are similar to those of adenocarcinoma of the rectum, such as bleeding, abdominal pain, changes in bowel habits, and weight loss6,11.
Colonoscopy with biopsies of any visible abnormalities is crucial to the diagnosis of rectal SCC. A polyp or an ulcerated obstructing bulk is generally revealed during endoscopy examinations14.
Williams et al.10have suggested some criteria that are necessary for the diagnosis of colorectal SCC: no evidence of SCC of any other primary site, absence of extension of the tumor from the anal squamous epithelium, and absence of a squamous-lined fistula tract to the affected bowel. In addition to these criteria, histology results consistent with a squamous carcinoma without glandular differentiation is also required17,18.
In immunohistochemistry analysis, the most useful cytokeratins required to differentiate rectal from anal SCC are AE1/AE3, CAM 5.2, and 34B12. The cytokeratins AE1/AE3 stain positively for cells of squamous origin; the cytokeratin CAM 5.2 is able to stain for rectal SCC, but not for anal SCC1,9.
MRI of the rectum and trans-rectal endoscopic ultrasound(R-EUS) are necessary before therapeutic approach. R-EUS provides improved local lymph node evaluation4.
Surgery is the gold standard treatment for colorectal SCC according to most authors19. Nahas1demonstrated that the addition of radiation therapy before surgery increased sphincter preservation from 67% to 71%. Rasheed et al.20and Clark et al.21evaluated the success of chemoradiotherapy for the treatment of SCC of the rectum in two separate populations; using 5FU based treatment with either mitomycin-C or cisplatin. Our patient received a combined treatment with cisplatin and 5FU in concomitance with external beam radiation therapy, followed by anterior resection of the rectum.
Local excision is appropriate in selected stage T1 cases and for more advanced disease. Two surgical techniques can be performed depending on tumor location: lower rectal anterior resection or abdomino-perineal resection. The abdomino-perineal resection of the rectum is associated with high morbidity rates and low patients’ satisfaction22,23. In the present case, low anterior resection was performed.
Comer et al.19have suggested a poorer prognosis for colorectal SCC than for adenocarcinoma. In fact, the overall 5-year survival rate of SCC is 32%, with significant variation by stage: Duke B, 50%; Duke C, 33%; and Duke D, 0%.Studies have suggested improved outcomes with preoperative CRT4.
SCC of the rectum is a rare malignancy. The available information is clouded by a lack of uniformity in diagnosing and staging the disease4. Treatment of SCC remains very challenging, and the acquisition of more consistent data is needed.
Conflict of interest statement
No potential conflicts of interest are disclosed.
1.Nahas CS, Shia J, Joseph R, Schrag D, Minsky BD, Weiser MR, et al.Squamous-cell carcinoma of the rectum: a rare but curable tumor.Dis Colon Rectum. 2007; 50: 1393-400.
2.Crissman JD. Adenosquamous and squamous cell carcinoma of the colon. Am J Surg Pathol. 1978; 2: 47-54.
3.Juturi JV, Francis B, Koontz PW, Wilkes JD. Squamous-cell carcinoma of the colon responsive to combination chemotherapy:report of two cases and review of the literature. Dis Colon Rectum.1999; 42: 102-9.
4.Dyson T, Draganov PV. Squamous cell cancer of the rectum. World J Gastroenterol. 2009; 15: 4380-6.
5.Raiford TS. Epitheliomata of the lower rectum and anus. Surg Gynecol Obstet. 1933; 57: 21-35.
6.Lafreniere R, Ketcham AS. Primary squamous carcinoma of the rectum. Report of a case and review of the literature. Dis Colon Rectum. 1985; 28: 967-72.
7.Pemberton M, Lendrum J. Squamous-cell carcinoma of the caecum following ovarian adenocarcinoma. Br J Surg. 1968; 55: 273-6.
8.Yurdakul G, de Reijke TM, Blank LE, Rauws EA. Rectal squamous cell carcinoma 11 years after brachytherapy for carcinoma of the prostate. J Urol. 2003; 169: 280.
9.Wiener MF, Polayes SH, Yidi R. Squamous carcinoma with schistosomiasis of the colon. Am J Gastroenterol. 1962; 37: 48-54.
10.Williams GT, Blackshaw AJ, Morson BC. Squamous carcinoma of the colorectum and its genesis. J Pathol. 1979; 129: 139-47.
11.Audeau A, Han HW, Johnston MJ, Whitehead MW, Frizelle FA.Does human papilloma virus have a role in squamous cell carcinoma of the colon and upper rectum? Eur J Surg Oncol. 2002;28: 657-60.
12.Ouban A, Nawab RA, Coppola D. Diagnostic and pathogenetic implications of colorectal carcinomas with multidirectional differentiation: a report of 4 cases. Clin Colorectal Cancer. 2002; 1:243-8.
13.Jaworski RC, Biankin SA, Baird PJ. Squamous cell carcinoma in situ arising in inflammatory cloacogenic polyps: report of two cases with PCR analysis for HPV DNA. Pathology. 2001; 33: 312-4.
14.Nebesio CL, Mirowski GW, Chuang TY. Human papillomavirus:clinical significance and malignant potential. Int J Dermatol. 2001;40: 373-9.
15.Sotlar K, Köveker G, Aepinus C, Selinka HC, Kandolf R, Bültmann B. Human papillomavirus type 16-associated primary squamous cell carcinoma of the rectum. Gastroenterology. 2001; 120: 988-94.
16.Kong CS, Welton ML, Longacre TA. Role of human papillomavirus in squamous cell metaplasia-dysplasia-carcinoma of the rectum.Am J Surg Pathol. 2007; 31: 919-25.
17.Carroll D, Rajesh PB. Colonic metastases from primary squamous cell carcinoma of the lung. Eur J Cardiothorac Surg. 2001; 19:719-20.
18.Cooper HS. Carcinoma of the colon and rectum. In: Norris HT,editor. Pathology of the colon, small intestine, and anus. 2nd ed.New York: Churchill Livingstone; 1989. p.201.
19.Comer TP, Beahrs OH, Dockerty MB. Primary squamous cell carcinoma and adenocanthoma of the colon. Cancer. 1971; 28:1111-7.
20.Rasheed S, Yap T, Zia A, McDonald PJ, Glynne-Jones R. Chemoradiotherapy: an alternative to surgery for squamous cell carcinoma of the rectum-report of six patients and literature review.Colorectal Dis. 2009; 11: 191-7.
21.Clark J, Cleator S, Goldin R, Lowdell C, Darzi A, Ziprin P.Treatment of primary rectal squamous cell carcinoma by primary chemoradiotherapy: should surgery still be considered a standard of care? Eur J Cancer. 2008; 44: 2340-3.
22.Townsend CM, Beauchamp RD, Evers BM, Mattox K. Sabiston textbook of surgery: the biological basis of modern surgical practice. 17th ed. Philadelphia: Saunders; 2004.
23.Bossema E, Stiggelbout A, Baas-Thijssen M, van de Velde C,Marijnen C. Patients' preferences for low rectal cancer surgery. Eur J Surg Oncol. 2008; 34: 42-8.
Cite this article as: Sonia Z, Amira D, Hanene B, Nouha A, Wiem K, Omar T,et al. Complete pathologic response after chemoradiotherapy in a patient with rectal squamous cell carcinoma: a case report . Cancer Biol Med. 2017; 14:414-7. doi: 10.20892/j.issn.2095-3941.2017.0010
Daldoul Amira
E-mail: amira.krir@outlook.com
January 22, 2017; accepted April 24, 2017.
Available at www.cancerbiomed.org
Copyright © 2017 by Cancer Biology & Medicine
 Cancer Biology & Medicine2017年4期
Cancer Biology & Medicine2017年4期
- Cancer Biology & Medicine的其它文章
- Brain metastasis in non-small cell lung cancer (NSCLC)patients with uncommon EGFR mutations: a report of seven cases and literature review
- Increased expression of YAP1 in prostate cancer correlates with extraprostatic extension
- Thermogenic protein UCP1 and UCP3 expression in nonsmall cell lung cancer: relation with glycolysis and anaerobic metabolism
- Profile of the breast cancer susceptibility marker rs4245739 identifies a role for miRNAs
- Promoter methylation of Wnt/β-Catenin signal inhibitor TMEM88 is associated with unfavorable prognosis of nonsmall cell lung cancer
- Brain metastasis in advanced colorectal cancer: results from the South Australian metastatic colorectal cancer (SAmCRC)registry
