Brain metastasis in non-small cell lung cancer (NSCLC)patients with uncommon EGFR mutations: a report of seven cases and literature review
Puchun Er, Tian Zhang, Jing Wang, Qingsong Pang, Ping Wang
Department of Radiotherapy, Tianjin Medical University Cancer Institute and Hospital; National Clinical Research Center for Cancer; Key Laboratory of Cancer Prevention and Therapy, Tianjin; Tianjin’s Clinical Research Center for Cancer, Tianjin,300060, China
CASE REPORT
Brain metastasis in non-small cell lung cancer (NSCLC)patients with uncommon EGFR mutations: a report of seven cases and literature review
Puchun Er, Tian Zhang, Jing Wang, Qingsong Pang, Ping Wang
Department of Radiotherapy, Tianjin Medical University Cancer Institute and Hospital; National Clinical Research Center for Cancer; Key Laboratory of Cancer Prevention and Therapy, Tianjin; Tianjin’s Clinical Research Center for Cancer, Tianjin,300060, China
Brain metastasis (BM) arising from non-small cell lung cancer (NSCLC) with rare epidermal growth factor receptor (EGFR)mutations is quite rare. The prognosis and therapeutic effects of BM remain enigmatic. To the best of our knowledge, this is the first report to make a separate analysis of BM from NSCLC patients with original uncommon EGFR mutations. We retrospectively reviewed 7 cases of BM arising from 42 cases of uncommon EGFR mutated lung cancer in Tianjin Medical University Cancer Institute and Hospital. We also performed a literature review to assess therapeutic features and outcomes.
Brain metastasis; NSCLC; uncommon EGFR mutations; EGFR-TKIs; brain radiotherapy; chemotherapy
Introduction
Brain metastasis (BM) is especially prevalent in patients with common epidermal growth factor receptor (EGFR) mutation positive non-small cell lung cancer (NSCLC)1,2and has been historically considered as a major determinant of overall survival (OS). It is one of the common causes leading to treatment failure. The survival time of these patients is approximately 7–12 months3,4, according to recent reports.EGFR- tyrosine kinase inhibitors (TKIs) are frequently used as a standard treatment of BM from EGFR-mutation positive NSCLC5,6. Patients with uncommon EGFR mutations have lower response rates to EGFR-TKIs than those who have more common mutations. Platinum-based chemotherapy may be relatively effective for NSCLC with uncommon EGFR mutations7. However, reports of BM from NSCLC with uncommon EGFR mutations are extremely rare. Here, we reported 7 cases of BM arising from 42 cases of uncommon EGFR mutated lung cancer in our hospital. We also reviewed the literature to assess therapeutic features and outcomes.
Cases report
Case 1
In April 2012, the patient (stage: T3N1M0 IIIa) had undergone wedge resection of an upper right lung neoplasm.The pathological result was mucous adenocarcinoma with micropapillary involvement. The genetic subtype was EGFR 20: 2369C > T (T790M). The patient received 18 cycles of adjuvant chemotherapy with pemetrexed plus carboplatin.Following the chemotherapy treatment, he received thoracic radiotherapy combined with pemetrexed for 2 cycles.Because of the EGFR-mutation status, we initiated treatment with gefitinib in January 2015. The treatment regimen was changed to afatinib in March 2015, due to the therapeutic effect. Unfortunately, he withdrew from afatinib treatment voluntarily 2 months later for financial reasons.
In September 2015, three and a half years later, brain magnetic resonance imaging (MRI) and positron emission tomography revealed metastasis in the patient's brain, left lung and mediastinal lymph nodes. He received bevacizumab combined with different regimens of chemotherapy for 14 cycles from September 2015 to November 2016. Currently,the patient has no neurologic symptoms, and has survived 5 years since diagnosis (Figure 1).

Figure 1 Case 1: brain magnetic resonance imaging (MRI) showed metastasis in the patient's brain in September 2015.
Case 2
A 69-year-old man with a history of smoking presented with bronchioloalveolar carcinoma of the right lung (stage:T2aN1M0 IIa). He had metastatic lymphadenopathy near the bronchi. A mutation in EGFR exon 18 (2156G > C; G719S)was detected.
In August 2011, he had undergone resection of the inferior lobe of the right lung and lymphadenectomy by videoassisted thoracic surgery. He was administered postoperative targeted therapy by erlotinib, and withdrew after 1 year.When he experienced numbness in the fingers of his right hand in November 2015, brain MRI revealed multiple fronto-parietal metastases. He received brain radiotherapy(42 Gy/10 f). After 6 months, in order to remove compression, he received cyber knife treatment (20 Gy/1 f) in his right brain ventricle (Figure 2).
At the last assessment, chest computed tomography scan and brain MRI suggested the patient was in stable condition.He has survived over 5 years since diagnosis (67+ months).
Case 3
T2aN0M0 (stage Ib) lung adenocarcinoma was diagnosed in a 56-year-old woman without a history of smoking. EGFR mutation analysis identified a mutation in exon 18 (2156G >C; G719S). BM was found 1 month after radical resection in March 2014. Four cycles of chemotherapy plus icotinib was administered, after which she received erlotinib for 3 months.Her subjective symptoms improved gradually within 7 months of the administration of TKIs. The patient is still alive 3 years after diagnosis.

Figure 2 Case 2: pre-radiotherapy brain MRI revealed multiple fronto-parietal metastases in November 2015.
Case 4
A 53-year-old woman underwent resection of the inferior lobe of the right lung and lymphadenectomy when she was diagnosed with T2aN2M0 (stage- IIIa) lung adenocarcinoma with micropapillary involvement in March 2013. An EGFR mutation in exon 20 (2369C > T; T790M) was discovered.She received four cycles of adjuvant chemotherapy with pemetrexed plus carboplatin. In January 2015, metastasis was discovered in her occipital lobe. Erlotinib and gefitinib were administered until she died due to the primary tumor in October 2015 (Figure 3).
Case 5
A 70-year-old woman was diagnosed with lung adenocarcinoma (Stage: T1bN2M0 IIIa, micropapillary+).An EGFR mutation in exon 20: (2369C > T; T790M) was discovered. She underwent resection of the inferior lobe of the right lung and lymphadenectomy, followed by four cycles of pemetrexed plus carboplatin chemotherapy. Six months later, brain and bones metastases appeared. First-generation TKIs were administered for 1 year. She died in May 2015, 25 months after the diagnosis and 6 months after the withdrawal of TKIs.
Case 6
A 56-year-old man was diagnosed with lung adenocarcinoma(stage: T2aN2M0 IIIa, micropapillary+) with an EGFR mutation in exon 18 (2156G > C; G719S). He underwent excision plus lymphadenectomy. Adjuvant chemotherapy was started in April 2014. In the beginning of 2015, multiple metastases were found in his whole body, including the brain. The patient died on March 31, 2015, 1 year after the diagnosis.
Case 7
A 70-year-old woman with a history of smoking was diagnosed with undifferentiated lung carcinoma (stage:T2bN3M0 IIIb) in August 2013. A mutation in exon 18(2156G > C; G719S) of EGFR was detected. Erlotinib was administered for half a year and chemotherapy with pemetrexed plus lobaplatin was administered through August 2014. Shortly after that, the patient developed bone metastasis and BM. She died due to cerebral hemorrhage in November 2014.
Summary
We observed 7 cases of BM from 42 lung cancer patients with uncommon EGFR mutations (2 men, 5 women). The median age was 62 years old (range, 53–70). Three cases were smokers and 4 were non-smokers. Four cases had mutations in exon 18 while the other 3 had mutation in exon 20. One case had stage I disease, 1 was stage II, and 5 were stage III.Six cases were administered first-generation EGFR-TKIs, and three cases received EGFR-TKIs after developing BM. Case 1 changed to afatinib and only case 2 received brain radiotherapy. The Chi-square test showed that lymph node metastasis and metastasis to other sites were significant factors for developing BM (P=0.018 and P=0.002,respectively). The major information of these cases is presented in Tables 1–4.
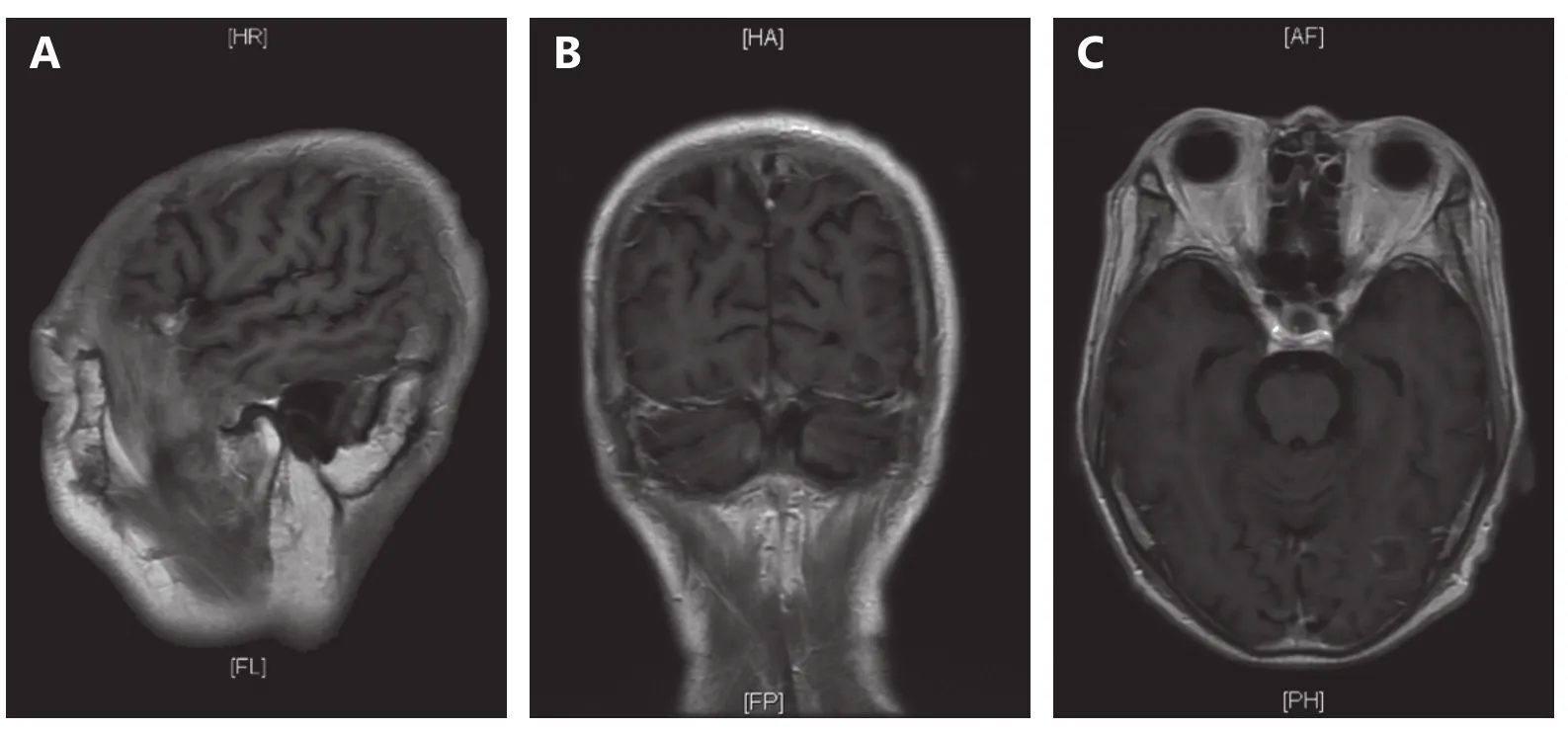
Figure 3 Case 4: metastasis was found in the occipital lobe in January 2015, 21 months after the first diagnosis.
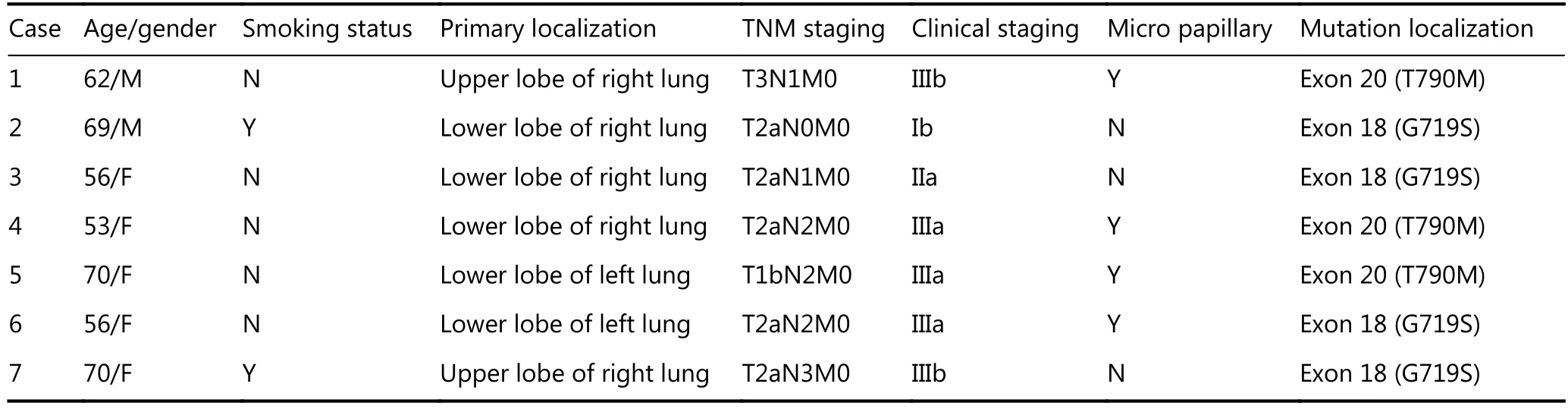
Table 1 Essential information of the 7 cases
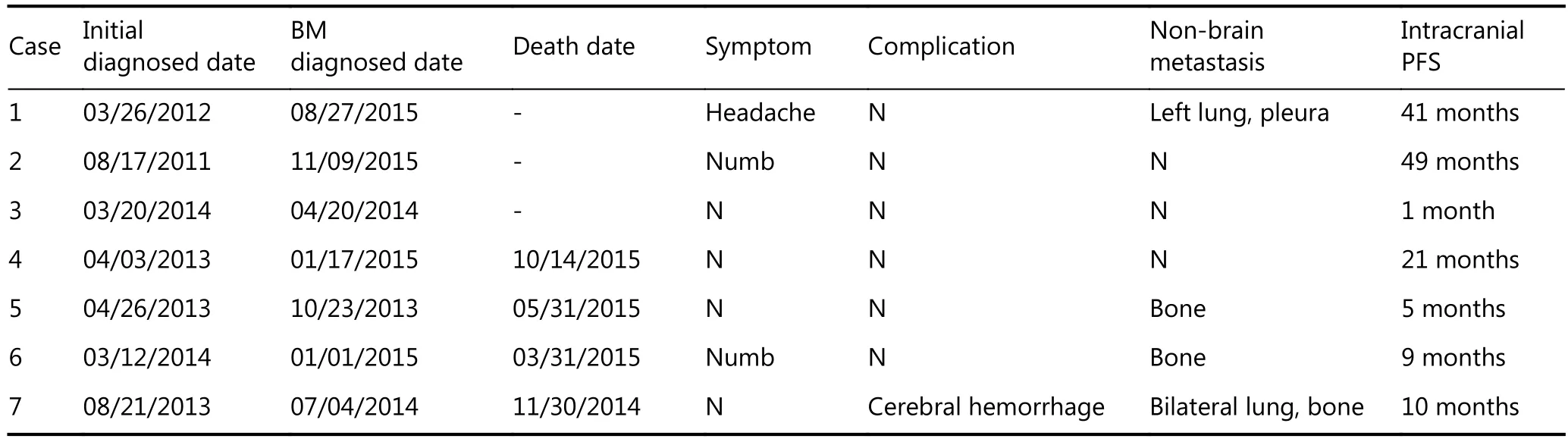
Table 2 Clinical features of the 7 cases
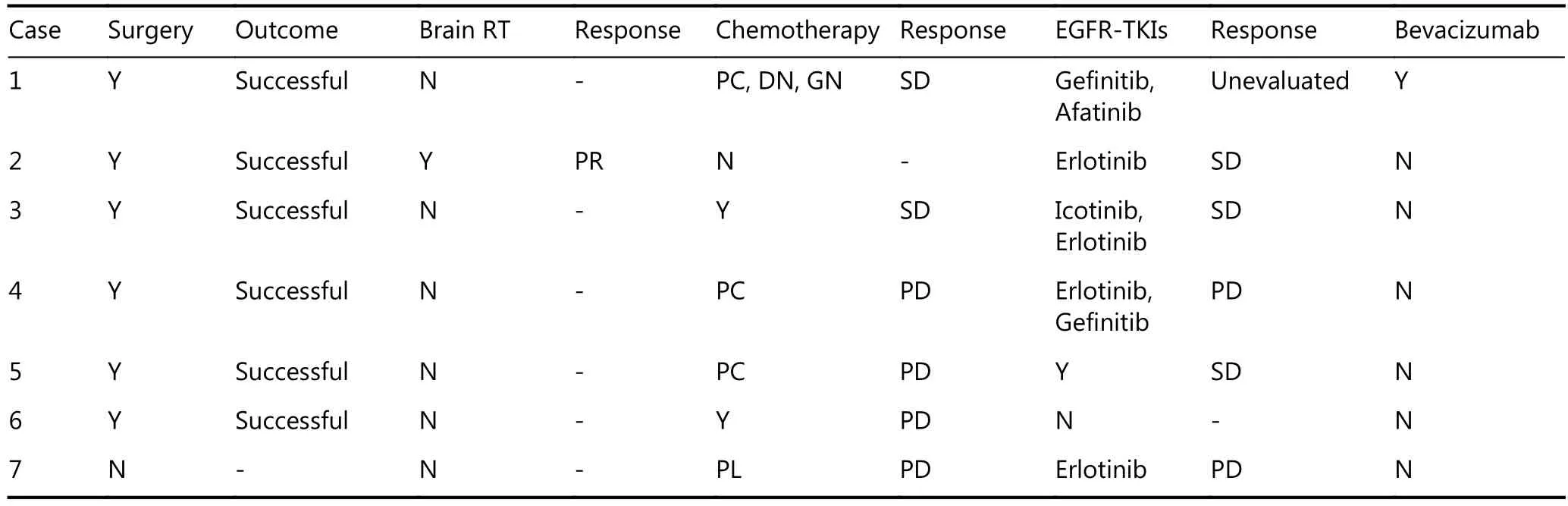
Table 3 Summary of clinical information of treatment
Discussion
To our knowledge, this is the first report to make a separate analysis of BM from NSCLC with rare EGFR mutations.Approximately 20%–50% of NSCLC patients develop BM1-3,8,9, which is associated with poor prognosis. The median survival time for patients with untreated BMs is only about 2 months, and it may increase to 3–6 months following whole-brain radiotherapy (WBRT)3,4,8. Recently, prognosis has been improved by using brain radiotherapy combined with chemotherapy, resulting in a median survival time ranging from 6 to 12 months4,8,10. There is a higher incidenceof BM in NSCLC patients with EGFR mutations (39.2%,compared to 28.2% for those without EGFR mutations, P <0.038)2. Patients with mutation in exon 19 have the highest incidence of BM11. The current mainstream view is that EGFR-mutated NSCLC has a higher incidence of BM, but the survival time may be longer than wild -type EGFR NSCLC because of the use of EGFR-TKIs. Today, thanks to TKIs,NSCLC patients with EGFR mutations with BM at diagnosis achieve a median survival of approximately 18 months10,12,13.Therefore, the higher BM incidence in the EGFR-mutated group might partly be explained with a prolonged survival in the EGFR group. However, for uncommon mutations, the incidence of BM, the survival time and the treatment methods are still unclear. In a study of 4 NSCLC patients with uncommon EGFR mutations (one with a mutation in exon 18 and three with mutations in exon 20), only one had BM, giving a 25% incidence rate11. In our cases, the incidence rate of BM was 16.7% for patients with uncommon EGFR mutations, lower than expected. According to the Chi-square test, BM development was probably associated with lymph node metastasis and metastasis to other sites (P=0.018 and P=0.002, respectively; Table 4). Both are adverse prognostic factors. However, we cannot jump to a conclusion due to the limitation of our small sample size. The reason for this low incidence rate might be that many patients have died from the primary tumor and complications before they developed BM. The majority of NSCLC patients who developed BM survive for 3–6 months, and the 1-year survival rate is 10%14.A study showed that the median progression-free survival(PFS) and OS were better in patients with common EGFR mutations than in patients with uncommon mutations (15.5 vs. 3.9 months, P < 0.001; and 37.3 vs. 17.4 months, P <0.001; respectively)7. The median intracranial PFS and OS of the 7 cases in this study were 9 months (1–49 months) and 30 months (12–67+ months). Moreover, the 1-year survival rate in our study was 100%, obviously superior to the expectation. It may predict a better prognosis and therapeutic effects of BM in these cases, especially for case 1 and case 2.Treatment of NSCLC with uncommon EGFR mutations is still controversial. Of these seven cases, six underwent targeted therapy. Case 6 did not undergo targeted therapy,which might explain why he had the shortest survival time (1 year, 18 months shorter than the median OS of 30 months).Three of seven cases underwent EGFR-TKI treatment after developing BM. The median usage time and survival time with BM of these three cases were 10 months (7–12 months)and 20 months (9–35+ months), respectively. The sensitivity to EGFR-TKIs of patients with EGFR mutations differ from those with wild-type EGFR. Patients with uncommon mutations usually have higher sensitivity than those with wild-type EGFR and lower sensitivity than those with common mutations6,7,15-19, particularly with regards to first-
generation EGFR-TKIs (erlotinib, gefitinib, and icotinib)16-18,20-22. However, afatinib seems to be clinically active and well tolerated in many TKI-pretreated NSCLC patients harboring uncommon EGFR mutations23-25. Recent reports suggest that third-generation EGFR-TKIs (AZD9291 and AZD3759) may be an effective treatment for first- or secondgeneration EGFR-TKI-resistant NSCLC with EGFR mutations, depending on their effect as radiosensitizers and the high permeability of the blood brain barrier26-28.However, there are few studies exploring third generation TKIs and BM with rare mutations. In these seven cases, six were administered first-generation EGFR-TKIs as an important means of outpatient adjuvant therapy. Case 1 stopped using gefitinib and changed to afatinib due to the therapeutic effect. Since the administration time was short,we could not assess its contribution to his survival. His intracranial PFS and OS reached 41 months and 5 years,longer than the median intracranial PFS (9 months) and OS(30 months). As the only case receiving bevacizumab, case 1 also showed that bevacizumab therapy may be beneficial in combined treatment. Additionally, platinum-based chemotherapy may be relatively effective for NSCLC with uncommon EGFR mutations7,22. The addition of pemetrexed to gefitinib seems to provide clinical benefit for PFS compared with gefitinib monotherapy29. Six cases received systemic chemotherapy as the first-line therapy, while case 2 received brain radiotherapy instead. Brain radiotherapy combined with EGFR-TKIs seems to be the standard therapy and is well tolerated in patients with BM of EGFR-mutated NSCLC5,8,12,30-36. Intracranial PFS was improved in patients receiving upfront radiotherapy compared with those receiving upfront EGFR-TKI (37.9 vs. 10.6 months; P <0.001)37. A recent multi-institutional analysis showed that using upfront EGFR-TKI and deferral of radiotherapy is related to shorter OS in EGFR mutated NSCLC patients with BM. The OS of patients who received stereotactic body radiation therapy followed by EGFR-TKIs was longer than patients who received WBRT followed by EGFR-TKIs38.However, for uncommon EGFR mutations, there is very little evidence to support the use of radiation therapy to treat BMs.Case 2 is the only stage I case and the only that received brain radiotherapy. The intracranial PFS and OS reached 49 months and 67 months, respectively, longer than the median 9 months and 30 months, respectively. Despite the interference of stage, this case with a desired response to brain radiotherapy might have important clinical implications. Neurological symptoms and comorbidities did not result in worse overall prognosis for patients with BM39.Even though cases 1 and 2 had symptoms like headache or numbness, they are still alive with ideal treatment effect.

Table 4 Association of BM status with clinicopathological variables
In summary, in addition to lymph node metastasis and metastasis to other sites, patients with uncommon EGFR mutations are more likely to develop BM. Prognosis and the therapeutic effects on BM from NSCLC with uncommon EGFR mutations are probably better than expected. Brain radiotherapy might offer a clinical benefit in the treatment of BM arising from NSCLC patients harboring uncommon EGFR mutations. First-generation EGFR-TKIs and afatinib might also represent effective treatment options for patients with uncommon EGFR mutations with BM. The effect of the third-generation TKIs is worth more examination. Future studies are needed to evaluate the effect of bevacizumab therapy in this combined treatment. Unfortunately, the limited number of cases in our study weakens the solidity and impact of our findings and we were unable to address some of our objectives more clearly. Thus, more randomized controlled clinical trials with a larger number of cases are warranted.
Conflict of interest statement
No potential conflicts of interest are disclosed.
1.Chi A, Komaki R. Treatment of brain metastasis from lung cancer.Cancers (Basel). 2010; 2: 2100-37.
2.Hsu F, De Caluwe A, Anderson D, Nichol A, Toriumi T, Ho C.EGFR mutation status on brain metastases from non-small cell lung cancer. Lung Cancer. 2016; 96: 101-7.
3.Ma SL, Xu YP, Deng QH, Yu XM. Treatment of brain metastasis from non-small cell lung cancer with whole brain radiotherapy and Gefitinib in a Chinese population. Lung Cancer. 2009; 65: 198-203.
4.Wei HP, Su M, Lin RF, Li HF, Zou CL. Prognostic factors analysis in EGFR mutation-positive non-small cell lung cancer with brain metastases treated with whole brain-radiotherapy and EGFR-tyrosine kinase inhibitors. Oncol Lett. 2016; 11: 2249-54.
5.Bogdanowicz BS, Hoch MA, Hartranft ME. Flipped script for gefitinib: A reapproved tyrosine kinase inhibitor for first-line treatment of epidermal growth factor receptor mutation positive metastatic nonsmall cell lung cancer. J Oncol Pharm Pract. 2017;23: 203-14.
6.Xu JL, Jin B, Chu TQ, Dong X, Yang HT, Zhang YW, et al. EGFR tyrosine kinase inhibitor (TKI) in patients with advanced non-small cell lung cancer (NSCLC) harboring uncommon EGFR mutations:A real-world study in China. Lung Cancer. 2016; 96: 87-92.
7.Arrieta O, Cardona AF, Corrales L, Campos-Parra AD, Sánchez-Reyes R, Amieva-Rivera E, et al. The impact of common and rare EGFR mutations in response to EGFR tyrosine kinase inhibitors and platinum-based chemotherapy in patients with non-small cell lung cancer. Lung Cancer. 2015; 87: 169-75.
8.Zheng MH, Sun HT, Xu JG, Yang G, Huo LM, Zhang P, et al.Combining whole-brain radiotherapy with gefitinib/erlotinib for brain metastases from non-small-cell lung cancer: A meta-analysis.Biomed Res Int. 2016; 2016: 5807346.
9.Yamanaka R. Medical management of brain metastases from lung cancer (Review). Oncol Rep. 2009; 22: 1269-76.
10.Noronha V, Joshi A, Gokarn A, Sharma V, Patil V, Janu A, et al.The importance of Brain metastasis in EGFR mutation positive NSCLC patients. Chemother Res Pract. 2014; 2014: 856156
11.Li B, Sun SZ, Yang M, Shi JL, Xu W, Wang XF, et al. The correlation between EGFR mutation status and the risk of brain metastasis in patients with lung adenocarcinoma. J Neuro-Oncol.2015; 124: 79-85.
12.Chen YM. Usage of EGFR-TKI and WBRT in NSCLC patients with brain metastases. Ann Palliat Med. 2013; 2: 108-10.
13.Jain A, Lim C, Gan EM, Ng DZ, Ng QS, Ang MK, et al. Impact of smoking and brain metastasis on outcomes of advanced EGFR mutation lung adenocarcinoma patients treated with first line epidermal growth factor receptor tyrosine kinase inhibitors. PLoS One. 2015; 10: e0123587.
14.Huang HQ, Zhu SL, Wang SB, Li W. Quick regression of brain metastases from lung adenocarcinoma with epidermal growth factor receptor-tyrosine kinase inhibitor treatment: A case report and literature review. Mol Clin Oncol. 2016; 5: 380-2.
15.Yang X, Chen HX, Zhang H, Duan JC, An TT, Zhao J, et al.Effectiveness of tyrosine kinase inhibitors on uncommon epidermal growth factor receptor mutations in non-small cell lung cancer.Chin J Lung Cancer. 2015; 18: 493-9.
16.Wu J-Y, Yu C-J, Chang Y-C, Yang C-H, Shih J-Y, Yang P-C.Effectiveness of tyrosine kinase inhibitors on "uncommon"epidermal growth factor receptor mutations of unknown clinical significance in non-small cell lung cancer. Clin Cancer Res. 2011;17: 3812-21.
17.Klughammer B, Brugger W, Cappuzzo F, Ciuleanu T, Mok T, Reck M, et al. Examining treatment outcomes with erlotinib in patients with advanced non-small cell lung cancer whose tumors harbor uncommon EGFR mutations. J Thorac Oncol. 2016; 11: 545-55.
18.Massarelli E, Johnson FM, Erickson HS, Wistuba II,Papadimitrakopoulou V. Uncommon epidermal growth factor receptor mutations in non-small cell lung cancer and their mechanisms of EGFR tyrosine kinase inhibitors sensitivity and resistance. Lung Cancer. 2013; 80: 235-41.
19.Cheng C, Wang R, Li Y, Pan YJ, Zhang Y, Li H, et al. EGFR exon 18 mutations in East Asian patients with lung adenocarcinomas: A comprehensive investigation of prevalence, clinicopathologic characteristics and prognosis. Sci Rep. 2015; 5: 13959
20.Chen D, Song Z, Cheng G. Clinical efficacy of first-generation EGFR-TKIs in patients with advanced non-small-cell lung cancer harboring EGFR exon 20 mutations. Onco Targets Ther. 2016; 9:4181-6.
21.Kempf E, Lacroix L, Soria J-C. First reported case of unexpected response to an epidermal growth factor receptor tyrosine kinase inhibitor in the I744M uncommon EGFR mutation. Clin Lung Cancer. 2015; 16: e259-61.
22.Watanabe S, Minegishi Y, Yoshizawa H, Maemondo M, Inoue A,Sugawara S, et al. Effectiveness of gefitinib against non-small-cell lung cancer with the uncommon EGFR mutations G719X and L861Q. J Thorac Oncol. 2014; 9: 189-94.
23.Heigener DF, Schumann C, Sebastian M, Sadjadian P, Stehle I,Marten A, et al. Afatinib in non-small cell lung cancer harboring uncommon EGFR mutations pretreated with reversible EGFR inhibitors. Oncologist. 2015; 20: 1167-74.
24.Yang JC-H, Sequist LV, Geater SL, Tsai C-M, Mok TSK, Schuler M,et al. Clinical activity of afatinib in patients with advanced nonsmall-cell lung cancer harbouring uncommon EGFR mutations: a combined post-hoc analysis of LUX-Lung 2, LUX-Lung 3, and LUX-Lung 6. Lancet Oncol. 2015; 16: 830-8.
25.Yatabe Y, Pao W, Jett JR. Encouragement to submit data of clinical response to EGFR-TKIs in patients with uncommon EGFR mutations. J Thorac Oncol. 2012; 7: 775-6.
26.Zeng QB, Wang JB, Cheng ZQ, Chen K, Johnström P, Varnäs K, et al. Discovery and evaluation of clinical candidate AZD3759, a potent, oral active, central nervous system-penetrant, epidermal growth factor receptor tyrosine kinase inhibitor. J Med Chem.2015; 58: 8200-15.
27.Nanjo S, Ebi H, Arai S, Takeuchi S, Yamada T, Mochizuki S, et al.High efficacy of third generation EGFR inhibitor AZD9291 in a leptomeningeal carcinomatosis model with EGFR-mutant lung cancer cells. Oncotarget. 2016; 7: 3847-56.
28.Kelley K, Knisely J, Symons M, Ruggieri R. Radioresistance of Brain Tumors. Cancers (Basel). 2016; 8: 42.
29.Cheng Y, Murakami H, Yang P-C, He JX, Nakagawa K, Kang Jin H,et al. Randomized phase II trial of gefitinib with and without pemetrexed as first-line therapy in patients with advanced nonsquamous non-small-cell lung cancer with activating epidermal growth factor receptor mutations. J Clin Oncol. 2016; 34: 3258-66.
30.Zeng Y-D, Zhang L, Liao H, Liang Y, Xu F, Liu J-L, et al. Gefitinib alone or with concomitant whole brain radiotherapy for patients with brain metastasis from non-small-cell lung cancer: A retrospective study. Asian Pac J Cancer Prev. 2012; 13: 909-14.
31.Jiang T, Min WJ, Li YN, Yue ZJ, Wu CY, Zhou CC. Radiotherapy plus EGFR TKIs in non-small cell lung cancer patients with brain metastases: an update meta-analysis. Cancer Med. 2016; 5: 1055-65.
32.Couñago F, Rodríguez A, Calvo P, Luna J, Monroy JL, Taboada B,et al. Targeted therapy combined with radiotherapy in non-smallcell lung cancer: a review of the Oncologic Group for the Study of Lung Cancer (Spanish Radiation Oncology Society). Clin Transl Oncol. 2016; 19: 31-43.
33.Halasz LM, Uno H, Hughes M, D’Amico T, Dexter EU, Edge SB, et al. Comparative effectiveness of stereotactic radiosurgery versus whole-brain radiation therapy for patients with brain metastases from breast or non-small cell lung cancer. Cancer. 2016; 122: 2091-100.
34.Ricciardi S, de Marinis F. Multimodality management of non-small cell lung cancer patients with brain metastases. Curr Opin Oncol.2016; 22: 86-93.
35.Ulahannan D, Lee SM. Erlotinib plus concurrent whole-brain radiation therapy for non-small cell lung cancers patients with multiple brain metastases. Transl Lung Cancer Res. 2016; 5: 208-11.
36.Lu YY, Fan Y. Combined action of EGFR tyrosine kinase inhibitors and whole-brain radiotherapy on EGFR-mutated non-small-cell lung cancer patients with brain metastasis. Onco Targets Ther.2016; 9: 1135-43.
37.Magnuson WJ, Yeung JT, Guillod PD, Gettinger SN, Yu JB, Chiang VL. Impact of deferring radiation therapy in patients with epidermal growth factor receptor-mutant non-small cell lung cancer who develop brain metastases. Int J Radiat Oncol Biol Phys.2016; 95: 673-9.
38.Magnuson WJ, Lester-Coll NH, Wu AJ, Yang TJ, Lockney NA,Gerber NK, et al. Management of brain metastases in tyrosine kinase inhibitor–naïve epidermal growth factor receptor–mutant non–small-cell lung cancer: A retrospective multi-institutional analysis. J Clin Oncol. 2017; 35: 1070-7.
39.Paydar I, Oermann EK, Knoll M, Lee J, Collins BT, Ewend M, et al.The Value of the history and physical for patients with newly diagnosed brain metastases considering radiosurgery. Front Oncol.2016; 6: 40.
Cite this article as: Er P, Zhang T, Wang J, Pang Q, Wang P. Brain metastasis in non-small cell lung cancer (NSCLC) patients with uncommon EGFR mutations: a report of seven cases and literature review. Cancer Biol Med.2017; 14: 418-25. doi: 10.20892/j.issn.2095-3941.2017.0079
Qingsong Pang and Ping Wang
E-mail: pangqingsong2013@126.com and wangping@tjmuch.com
June 20, 2017; accepted October 13, 2017.
Available at www.cancerbiomed.org
Copyright © 2017 by Cancer Biology & Medicine
 Cancer Biology & Medicine2017年4期
Cancer Biology & Medicine2017年4期
- Cancer Biology & Medicine的其它文章
- A race to uncover a panoramic view of primary liver cancer
- The ascent of immune checkpoint inhibitors: is the understudy ready for a leading role?
- Cell cycle regulation and anticancer drug discovery
- Camptothecin-based nanodrug delivery systems
- Brain metastasis in advanced colorectal cancer: results from the South Australian metastatic colorectal cancer (SAmCRC)registry
- Promoter methylation of Wnt/β-Catenin signal inhibitor TMEM88 is associated with unfavorable prognosis of nonsmall cell lung cancer
