颈动脉粥样硬化斑块无创性高分辨力磁共振成像研究进展
高鹏 杨斌 焦力群 张鸿祺 朱凤水
·综述·
颈动脉粥样硬化斑块无创性高分辨力磁共振成像研究进展
高鹏 杨斌 焦力群 张鸿祺 朱凤水
颈动脉粥样硬化性狭窄与脑卒中复发密切相关。目前颈动脉狭窄的治疗方法主要包括药物治疗和外科手术(颈动脉支架成形术和颈动脉内膜切除术)。脑卒中预防在于识别颈动脉狭窄危险因素,筛查脑卒中复发高危患者,从而使其从药物治疗或外科手术中获益,然而目前仅根据颈动脉狭窄程度制定治疗方案,缺乏个体化治疗。近年来,新型影像学技术如无创性高分辨力磁共振成像(HRMRI)等,可以检测出颈动脉易损斑块。与传统数字减影血管造影术测量的颈动脉狭窄程度相比,无创性HRMRI可以根据颈动脉斑块特征准确预测同侧脑卒中风险,从而指导个体化治疗。
颈动脉狭窄; 动脉粥样硬化; 磁共振成像; 综述
颈动脉狭窄程度和粥样硬化斑块稳定性均与脑卒中发生和复发密切相关。目前主要采用数字减影血管造影术(DSA)定量检测颈动脉狭窄程度,而较少关注颈动脉斑块稳定性。近年来,无创性高?分辨力磁共振成像(HRMRI)逐渐用于检测颈动脉斑块的稳定性。与DSA相比,HRMRI具有无创性、安全、费用相对较低和可重复性等优点,在DSA显示血管狭窄的同时,HRMRI可以检测斑块稳定性,提供更敏感和客观信息,具有较高的个体化预测价值,是一项极具潜力的影像学技术。本文拟对近年HRMRI检测颈动脉斑块稳定性研究进展进行综述。
一、颈动脉狭窄相关临床试验的缺陷
根据美国心脏协会(AHA)/美国卒中协会(ASA)指南[1],颈动脉狭窄药物治疗和外科手术[包括颈动脉支架成形术(CAS)和颈动脉内膜切除术(CEA)]的治疗决策主要依靠两方面:(1)颈动脉狭窄程度,狭窄率<50%,轻度狭窄;50%~69%,中度狭窄;≥70%,重度狭窄。(2)是否存在临床症状。结合上述两方面,近20年涌现出大量颈动脉狭窄相关临床试验,例如,1991年的北美症状性颈动脉内膜切除术试验(NASCET)显示,对于颈动脉狭窄程度>70%患者,随访2年CEA组脑卒中复发率为9%,远低于单纯药物组的26%[2]。2004年针对无症状性颈动脉狭窄患者的无症状性颈动脉外科手术试验(ACST)显示,当颈动脉狭窄程度>60%时,随访5年CEA组脑卒中复发率为6.4%,低于单纯药物组的11.8%;该项研究还显示,对于>75岁的颈动脉狭窄程度>70%患者,随访5年脑卒中复发率和病死率显著下降[3];2010年,ACST试验10年长期随访结果发表于Lancet,CEA组脑卒中复发率为13.4%,低 于 单 纯 药 物 组 的 17.9%[4]。 Abbott 等[5]和Nicolaides等[6]报告的无症状性颈动脉狭窄患者单纯药物治疗后同侧脑卒中年复发率为0.6%~1.3%,低于ACST试验的CEA组(5年脑卒中复发率为6.4%,脑卒中年复发率约1.3%[3])和无症状性颈动脉粥样硬化研究(ACAS)的CEA组(5年脑卒中复发率为5.1%,脑卒中年复发率为1.0%[7])。因此,积极药物治疗仍是颈动脉狭窄的主要治疗方法,主要表现为:(1)部分高危患者并不能从颈动脉支架成形术和颈动脉内膜切除术中获益。(2)无论症状性(颈动脉狭窄程度<70%)或无症状性颈动脉狭窄患者,均无证据显示颈动脉支架成形术和颈动脉内膜切除术疗效优于单纯药物治疗[8]。因此,仅根据颈动脉狭窄程度进行危险程度分层是远远不够的,准确评价颈动脉狭窄程度和检测斑块稳定性以预测同侧脑卒中风险的个体化分析具有潜在的临床价值。
二、易损斑块定义
颈动脉斑块性状的判断和易损斑块的辨别,应借鉴“冠状动脉易损斑块”定义。“冠状动脉易损斑块”的定义最早由Virmani等[9]于2002年提出,他在尸检中发现冠状动脉粥样硬化斑块存在较大的富脂坏死核心(LRNC)和菲薄的纤维帽(FC),并确定其与心源性猝死有关。经临床、病理学、分子生物学和影像学研究,一致认为典型易损斑块的病理学特征为[7,10]:(1)较大的富脂坏死核心。(2)菲薄的纤维帽。(3)炎症反应,如巨噬细胞浸润。(4)斑块裂隙(fissured plaque)。(5)斑块表面钙化结节。(6)斑块内出血(IPH)。然而,上述“易损斑块”定义仅限于病理学层面,实际工作中难以获得活体斑块,因此需要影像学技术以实现体外无创性斑块成像。鉴于此,基于MRI的冠状动脉和颈动脉易损斑块成像技术和影像学分型应运而生[11]。1995年,AHA/ASA指南基于尸体解剖提出冠状动脉粥样硬化斑块病理学分型,分为Ⅰ~Ⅷ型[12],并在此基础上衍生出基于HRMRI的颈动脉易损斑块影像学分型,亦分为Ⅰ~Ⅷ型(表1)[13]。
三、颈动脉斑块无创性HRMRI在预测脑卒中风险方面优于单纯DSA测量颈动脉狭窄程度
1.较大的富脂坏死核心和菲薄的纤维帽显著增加脑卒中复发风险 (1)HRMRI可以识别和定量检测颈动脉斑块富脂坏死核心。既往大量研究显示,富脂坏死核心体积较大和(或)纤维帽菲薄或破裂与近期脑卒中事件、同侧动脉⁃动脉栓塞性缺血性卒中事件、颈动脉斑块去稳定化、纤维帽破裂、斑块内出 血 和 斑 块 体 积 扩 大 显 著 相 关[9,14⁃18]。 一 项 针 对 颈动脉狭窄程度50%~99%患者的横断面临床研究显示,HRMRI显示的同侧短暂性脑缺血发作(TIA)和(或)脑卒中与较大的富脂坏死核心和(或)菲薄或破裂的纤维帽显著相关,而与颈动脉狭窄程度无关联性[14]。(2)富脂坏死核心及其体积可以指导强化调脂治疗,亦可以评价调脂治疗效果[19]。Demarco等[14]的研究显示,尽管颈动脉狭窄程度未达重度狭窄(≤70%),但HRMRI仍显示易损斑块,表现为较大的富脂坏死核心合并斑块内出血、菲薄或破裂的纤维帽,考虑为脑卒中高危患者,与近期脑卒中风险具有相关性;尽管颈动脉狭窄程度达重度狭窄(>70%),但HRMRI仍显示稳定斑块,表现为富脂坏死核心体积较小、无斑块内出血、纤维帽厚重,考虑为无症状性颈动脉狭窄。一项纳入33例颈动脉狭窄患者的前瞻性临床试验显示,经过3年强化调脂治疗(阿托伐他汀10~80 mg/d+烟酸缓释片2 g/d+考来维仑3.80 g/d),复查HRMRI显示富脂坏死核心体积缩小,生物学时间效应表现为先出现斑块脂质排空,再出现斑块消融[19]。(3)HRMRI不单纯依靠 DSA测量的颈动脉狭窄程度即可定性和定量检测颈动脉斑块富脂坏死核心,从而进行脑卒中危险程度分层,筛选出适宜进行强化调脂治疗或外科手术的患者,以及评价治疗效果。
2.斑块内出血可以显著增加脑卒中复发风险
(1)斑块内出血发生机制是颈动脉斑块内富脂坏死核心的红细胞渗出和铁离子沉积。上述两个过程促进炎症反应,导致斑块去稳定化[10,20]。一项前瞻性临床试验显示,颈动脉斑块内出血与斑块进展相关[21]。既往由于临床检查方法有限,不能动态观察斑块内出血的发生与发展过程;现有的无创性颈动脉斑块成像技术可以同时观察斑块进展和颈动脉粥样硬化自然病程。(2)斑块内出血与斑块体积扩大和同侧动脉⁃动脉栓塞性缺血性卒中事件相关。Takaya等[17]纳入98例无症状性中至重度颈动脉狭窄患者,HRMRI显示43例(43.88%)存在斑块内出血,经过38.20个月随访,6例(6.12%)发生同侧缺血性卒中且均存在斑块内出血。Altaf等[22]纳入64例症状性颈动脉狭窄患者(狭窄程度30%~69%),39例(60.94%)基线HRMRI显示存在斑块内出血,经28个月随访,14例(21.88%)发生同侧缺血性卒中,其中13例(20.31%)存在斑块内出血。Meta分析显示,基线HRMRI显示存在斑块内出血的颈动脉狭窄患者发生同侧脑卒中风险是无斑块内出血患者的 5.60 倍[23]。
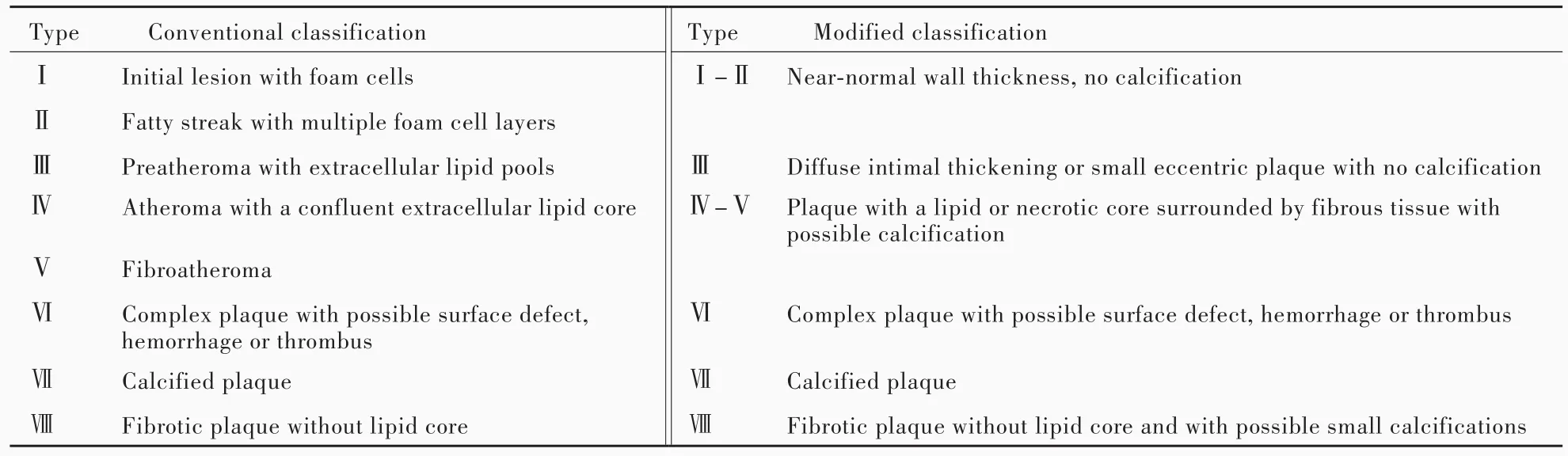
表1 基于HRMRI的颈动脉易损斑块影像学分型[13]Table 1. Conventional and modified classification of carotid vulnerable plaque based on HRMRI[13]
3.颈动脉斑块性状的性别差异及其与同侧脑卒中风险的关系 Ota等[24]纳入131例颈动脉狭窄患者(狭窄程度≥50%),男性不稳定型斑块特征高于女性,表现为男性颈动脉斑块富脂坏死核心、纤维帽菲薄或破裂、斑块内出血发生率均高于女性,男性易损斑块发生率亦高于女性,可以部分解释颈动脉内膜切除术在预防男性无症状性颈动脉狭窄相关脑卒中方面优于女性。另一项研究显示,颈动脉斑块性状的性别差异不仅限于中至重度颈动脉狭窄患者,亦存在于轻度颈动脉狭窄患者(狭窄程度<50%)[25]。因此,颈动脉狭窄的治疗策略应同时考虑易损斑块特征和性别因素。
四、展望
1.颈动脉斑块HRMRI技术 未来颈动脉斑块HRMRI技术有待改进和提高成像质量、缩短成像时间。2013年出现的非对比血管造影和出血成像(SNAP),将检查时间缩短至4~5分钟,可以检测到斑块内出血[26]。2012年出现的多对比三维梯度回波序列,可以提高成像质量,提供良好的信噪比(SNR)[27]。共识普遍认为,综合 3 项 HRMRI序列(如SNAP、3D⁃T1WI和增强3D⁃T1WI)扫描4分钟,即可获得颈动脉易损斑块的所有特征,包括富脂坏死核心、纤维帽和斑块内出血。若这一技术实现,快速多对比颈动脉斑块成像可以列入常规影像学检查。此外,提高成像质量还有赖于专用的颈动脉斑块线圈。第1代4通道线圈通常置于颈部中间,可以提供高信噪比图像,扫描范围覆盖10~12 cm区域;第2代颈部线圈采用高密度设计(6~8通道线圈),全面提高信噪比,亦可以增加扫描范围(覆盖16~18 cm区域),第1和2代线圈均已通过美国食品与药品管理局(FDA)审批,并已广泛应用于临床;第3代线圈为颈部高度集成线圈,系神经血管专用,扫描范围下至主动脉弓,上至Willis环和脑组织。如果将第3代线圈与新研发的HRMRI序列相结合,可以在45分钟内完成主动脉弓、颈动脉、脑组织和Willis环成像,极大地扩展颈动脉斑块成像的临床应用。目前,HRMRI技术自动识别颈动脉斑块成分的可行性已经完成[28],有助于临床医师对颈动脉斑块的认识和理解。
2.颈动脉斑块HRMRI的前瞻性多中心研究未来研究最核心的问题在于,颈动脉斑块HRMRI能否替代传统DSA测量的颈动脉狭窄程度以指导临床决策、改进治疗效果。可以设想,颈动脉易损斑块HRMRI可以同时指导药物治疗和外科手术。(1)HRMRI可以检出颈动脉易损斑块的富脂坏死核心,从而指导临床医师进行积极药物治疗;此外,还可以根据颈动脉斑块HRMRI设计前瞻性多中心随机对照临床试验,将存在富脂坏死核心的颈动脉狭窄患者随机分为标准药物治疗组和积极药物治疗组,除将短暂性脑缺血发作和(或)脑卒中作为终点事件外,也将富脂坏死核心体积变化作为终点事件或颈动脉粥样硬化疗效判定指标。(2)对于近期发生症状性颈动脉狭窄的患者,HRMRI可以进行脑卒中危险程度分层,筛选出适宜早期外科手术(颈动脉支架成形术或颈动脉内膜切除术)的患者。由此可见,即使轻至中度颈动脉狭窄患者,如果HRMRI检出斑块内出血,同侧短暂性脑缺血发作和(或)脑卒中风险明显增加;早期外科手术(颈动脉支架成形术或颈动脉内膜切除术)可以有效预防脑卒中复发,尚待前瞻性多中心随机对照临床试验的验证。
综上所述,脑卒中预防的关键在于早期识别危险因素。过去几十年,全世界在危险因素控制方面取得长足进步,如高血压、冠心病、糖尿病、高脂血症等均得到有效控制。未来脑卒中预防的重点在于识别个体化危险因素。国际上多个单中心临床试验业已证实基于HRMRI的颈动脉易损斑块成像技术较传统的颈动脉超声或DSA能够更准确预测脑卒中复发风险[17,29⁃30]。我们也寄希望于国际上的前瞻性临床试验以验证颈动脉易损斑块与同侧动脉⁃动脉栓塞性缺血性卒中事件的相关性。未来有望根据颈动脉易损斑块的HRMRI,提供个体化药物治疗和外科手术方案。
[1]Kernan WN,Ovbiagele B,Black HR,Bravata DM,Chimowitz MI,Ezekowitz MD,Fang MC,Fisher M,Furie KL,Heck DV,Johnston SC,Kasner SE,Kittner SJ,Mitchell PH,Rich MW,RichardsonD,Schwamm LH,WilsonJA;AmericanHeart Association Stroke Council,Councilon Cardiovascularand Stroke Nursing,Council on Clinical Cardiology,Council on Peripheral Vascular Disease.Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack:a guideline for healthcare professionals from the American Heart Association/American Stroke Association.Stroke,2014,45:2160⁃2236.
[2]Barnett HM,Taylor DW,Haynes RB,Sackett DL,Peerless SJ,Ferguson GG,Fox AJ,Rankin RN,Hachinski VC,Wiebers DO,Eliasziw M; North American Symptomatic Carotid Endarterectomy Trial Collaborators.Beneficial effect of carotid endarterectomy in symptomatic patients with high⁃grade carotid stenosis.N Engl J Med,1991,325:445⁃453.
[3]Halliday A,Mansfield A,Marro J,Peto C,Peto R,Potter J,Thomas D;MRC Asymptomatic Carotid Surgery Trial(ACST)Collaborative Group.Prevention of disabling and fatal strokes by successful carotid endarterectomy in patients without recent neurologicalsymptoms:randomised controlled trial.Lancet,2004,363:1491⁃1502.
[4]Halliday A,Harrison M,Hayter E,Kong X,Mansfield A,Marro J,Pan H,Peto R,Potter J,Rahimi K,Rau A,Robertson S,StreiflerJ,ThomasD;Asymptomatic Carotid Surgery Trial(ACST)Collaborative Group.10⁃year stroke prevention after successfulcarotid endarterectomy forasymptomatic stenosis(ACST⁃1):a multicentre randomised trial.Lancet,2010,376:1074⁃1084.
[5]Abbott AL,Chambers BR,Stork JL,Levi CR,Bladin CF,Donnan GA.Embolic signals and prediction of ipsilateral stroke or transient ischemic attack in asymptomatic carotid stenosis:a multicenter prospective cohort study.Stroke,2005,36:1128⁃1133.
[6]Nicolaides AN,Kakkos SK,Griffin M,Sabetai M,Dhanjil S,Tegos T,Thomas DJ,Giannoukas A,Geroulakos G,Georgiou N,Francis S,Ioannidou E,DoréCJ;Asymptomatic Carotid Stenosis and Risk of Stroke(ACSRS)Study Group.Severity of asymptomatic carotid stenosis and risk of ipsilateral hemispheric ischaemic events:results from the ACSRS study.Eur J Vasc Endovasc Surg,2005,30:275⁃284.
[7]NaghaviM,Libby P,Falk E,CasscellsSW,Litovsky S,Rumberger J,Badimon JJ,Stefanadis C,Moreno P,Pasterkamp G,Fayad Z,Stone PH,Waxman S,Raggi P,Madjid M,Zarrabi A,Burke A,Yuan C,Fitzgerald PJ,Siscovick DS,de Korte CL,Aikawa M,Airaksinen KE,Assmann G,Becker CR,Chesebro JH,Farb A,Galis ZS,Jackson C,Jang IK,Koenig W,Lodder RA,March K,Demirovic J,Navab M,Priori SG,Rekhter MD,Bahr R,Grundy SM,Mehran R,Colombo A,Boerwinkle E,Ballantyne C,Insull W Jr,Schwartz RS,Vogel R,Serruys PW,Hansson GK,Faxon DP,Kaul S,Drexler H,Greenland P,MullerJE,VirmaniR,RidkerPM,ZipesDP,Shah PK,Willerson JT.From vulnerable plaque to vulnerable patient:a call for new definitions and risk assessment strategies.PartⅡ.Circulation,2003,108:1772⁃1778.
[8]Abbott AL.Medical(nonsurgical)intervention alone is now best for prevention of stroke associated with asymptomatic severe carotid stenosis:results of a systematic review and analysis.Stroke,2009,40:E573⁃583.
[9]VirmaniR,BurkeAP,KolodgieFD,Farb A.Vulnerable plaque:the pathology of unstable coronary lesions.J Interv Cardiol,2002,15:439⁃446.
[10]NaghaviM,Libby P,Falk E,CasscellsSW,Litovsky S,Rumberger J,Badimon JJ,Stefanadis C,Moreno P,Pasterkamp G,Fayad Z,Stone PH,Waxman S,Raggi P,Madjid M,Zarrabi A,Burke A,Yuan C,Fitzgerald PJ,Siscovick DS,de Korte CL,Aikawa M,Juhani Airaksinen KE,Assmann G,Becker CR,Chesebro JH,Farb A,Galis ZS,Jackson C,Jang IK,Koenig W,LodderRA,MarchK,DemirovicJ,NavabM,PrioriSG,Rekhter MD,Bahr R,Grundy SM,Mehran R,Colombo A,Boerwinkle E,Ballantyne C,Insull W Jr,Schwartz RS,Vogel R,Serruys PW,Hansson GK,Faxon DP,Kaul S,Drexler H,Greenland P,Muller JE,Virmani R,Ridker PM,Zipes DP,Shah PK,Willerson JT.From vulnerable plaque to vulnerable patient:a call for new definitions and risk assessment strategies.PartⅠ.Circulation,2003,108:1664⁃1672.
[11]Saam T,Hatsukami TS,Takaya N,Chu B,Underhill H,Kerwin WS,Cai J,Ferguson MS,Yuan C.The vulnerable,or high⁃risk,atherosclerotic plaque: noninvasive MR imaging for characterization and assessment.Radiology,2007,244:64⁃77.
[12]Stary HC,Chandler AB,Dinsmore RE,Fuster V,Glagov S,Insull W Jr,Rosenfeld ME,Schwartz CJ,Wagner WD,Wissler RW.A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis:a report from the Committee on Vascular Lesions of the Council on Arteriosclerosis,American Heart Association.Circulation,1995,92:1355⁃1374.
[13]Cai JM,Hatsukami TS,Ferguson MS,Small R,Polissar NL,Yuan C.Classification of human carotid atherosclerotic lesions with in vivo multicontrast magnetic resonance imaging.Circulation,2002,106:1368⁃1373.
[14]Demarco JK,OtaH,Underhill HR,ZhuDC,ReevesMJ,Potchen MJ,Majid A,Collar A,Talsma JA,Potru S,Oikawa M,Dong L,Zhao X,Yarnykh VL,Yuan C.MR carotid plaque imaging and contrast⁃enhanced MR angiographyidentifies lesions associated with recent ipsilateral thromboembolic symptoms:an in vivo study at 3T.AJNR Am J Neuroradiol,2010,31:1395⁃1402.
[15]Hatsukami TS,Ross R,Polissar NL,Yuan C.Visualization of fibrous cap thickness and rupture in human atherosclerotic carotid plaque in vivo with high⁃resolution magnetic resonance imaging.Circulation,2000,102:959⁃964.
[16]Cai J,Hatsukami TS,Ferguson MS,Kerwin WS,Saam T,Chu B,Takaya N,PolissarNL,Yuan C.In vivo quantitative measurement of intact fibrous cap and lipid⁃rich necrotic core size in atherosclerotic carotid plaque:comparison of high⁃resolution,contrast⁃enhanced magnetic resonance imaging and histology.Circulation,2005,112:3437⁃3444.
[17]Takaya N,Yuan C,Chu B,Saam T,Underhill H,Cai J,Tran N,Polissar NL,Isaac C,Ferguson MS,Garden GA,Cramer SC,Maravilla KR, Hashimoto B, Hatsukami TS.Association between carotid plaque characteristics and subsequent ischemic cerebrovascular events:a prospective assessment with MRI⁃initial results.Stroke,2006,37:818⁃823.
[18]Underhill HR,Hatsukami TS,Cai J,Yu W,DeMarco JK,Polissar NL,Ota H,Zhao X,Dong L,Oikawa M,Yuan C.A noninvasive imaging approach to assess plaque severity:the carotid atherosclerosis score.AJNR Am J Neuroradiol,2010,31:1068⁃1075.
[19]Zhao XQ,Dong L,Hatsukami T,Phan BA,Chu B,Moore A,Lane T,Neradilek MB,Polissar N,Monick D,Lee C,Underhill H,Yuan C.MR imaging of carotid plaque composition during lipid⁃lowering therapy a prospective assessment of effect and time course.JACC Cardiovasc Imaging,2011,4:977⁃986.
[20]Kolodgie FD,Gold HK,Burke AP,Fowler DR,Kruth HS,Weber DK,Farb A,Guerrero LJ,Hayase M,Kutys R,Narula J, Finn AV, Virmani R. Intraplaque hemorrhage and progression of coronary atheroma.N Engl J Med,2003,349:2316⁃2325.
[21]Takaya N,Yuan C,Chu B,Saam T,Polissar NL,Jarvik GP,Isaac C,McDonough J,Natiello C,Small R,Ferguson MS,Hatsukami TS.Presence of intraplaque hemorrhage stimulates progression of carotid atherosclerotic plaques:a high⁃resolution magnetic resonance imaging study.Circulation,2005,111:2768⁃2775.
[22]Altaf N,Daniels L,Morgan PS,Auer D,MacSweeney ST,Moody AR,Gladman JR.Detection of intraplaque hemorrhage by magnetic resonance imaging in symptomatic patients with mild to moderate carotid stenosis predicts recurrent neurological events.J Vasc Surg,2008,47:337⁃342.
[23]Saam T,Hetterich H,Hoffmann V,Yuan C,Dichgans M,Poppert H,Koeppel T,Hoffmann U,Reiser MF,Bamberg F.Meta⁃analysis and systematic review of the predictive value of carotid plaque hemorrhage on cerebrovascular events by magnetic resonance imaging.J Am Coll Cardiol,2013,62:1081⁃1091.
[24]Ota H,Reeves MJ,Zhu DC,Majid A,Collar A,Yuan C,DeMarco JK.Sex differences in patients with asymptomatic carotid atherosclerotic plaque:in vivo 3.0⁃T magnetic resonance study.Stroke,2010,41:1630⁃1635.
[25]Ota H,Reeves MJ,Zhu DC,Majid A,Collar A,Yuan C,Demarco JK.Sex differences of high⁃risk carotid atherosclerotic plaque with less than 50%stenosis in asymptomatic patients:an in vivo 3T MRI study.AJNR Am J Neuroradiol,2013,34:1049⁃1055.
[26]Wang J,Börnert P,Zhao H,Hippe DS,Zhao X,Balu N,FergusonMS,Hatsukami TS,Xu J,Yuan C,KerwinWS.Simultaneous noncontrast angiography and intraplaque hemorrhage(SNAP)imaging for carotid atherosclerotic disease evaluation.Magn Reson Med,2013,69:337⁃345.
[27]Liu W,Balu N,Sun J,Zhao X,Chen H,Yuan C,Zhao H,Xu J,Wang G,Kerwin WS.Segmentation of carotid plaque using multicontrast 3D gradient echo MRI.J Magn Reson Imaging,2012,35:812⁃819.
[28]LiuF,XuD,FergusonMS,ChuB,Saam T,TakayaN,HatsukamiTS,Yuan C,Kerwin WS.Automated in vivo segmentation of carotid plaque MRI with Morphology⁃Enhanced probability maps.Magn Reson Med,2006,55:659⁃668.
[29]Kwee RM,van Oostenbrugge RJ,Mess WH,Prins MH,van der Geest RJ,ter Berg JW,Franke CL,Korten AG,Meems BJ,van Engelshoven JM,Wildberger JE,Kooi ME.MRI of carotid atherosclerosis to identify TIA and stroke patients who are at risk of a recurrence.J Magn Reson Imaging,2013,37:1189⁃1194.
[30]Turc G,Oppenheim C,Naggara O,Eker OF,Calvet D,Lacour JC,Crozier S,Guegan ⁃Massardier E,Hénon H,Neau JP,Toussaint JF,Mas JL,Méder JF,Touzé E;HIRISC Study Investigators. Relationships between recent intraplaque hemorrhage and stroke risk factors in patients with carotid stenosis:the HIRISC study.Arterioscler Thromb Vasc Biol,2012,32:492⁃499.
Research progress of noninvasive high⁃resolution magnetic resonance imaging in carotid atherosclerotic plaque
GAO Peng,YANG Bin,JIAO Li⁃qun,ZHANG Hong⁃qi,ZHU Feng⁃shui
Department of Neurosurgery,Xuanwu Hospital,Capital Medical University,Beijing 100053,China
Carotid atherosclerotic stenosis is closely related to recurrent ischemic stroke.Currently,therapies for carotid artery stenosis are mainly intensive medication or surgery,including carotid artery stenting(CAS)and carotid endarterectomy(CEA).The prevention of stroke lies in identifying risk factors for carotid artery stenosis,screening patients with high risk of recurrent stroke,so as to benefit from medication or surgery.However,therapeutic schedule is formulated only according to the degrees of carotid artery stenosis,and there lacks of individualized treatment. Recently,new imaging modalities,such as noninvasive high⁃resolution MRI(HRMRI)could detect the vulnerability of carotid atherosclerotic plaque.Compared with the degree of carotid artery stenosis measured by conventional DSA,noninvasive HRMRI can precisely predict the risk of ipsilateral stroke according to plaque morphology,so as to guide individualized treatment.
Carotid stenosis; Atherosclerosis; Magnetic resonance imaging; Review
ZHU Feng⁃shui(Email:zhufengshui@sina.com)
This study was supported by the NationalKey Research and DevelopmentProgram (No.2016YFC1301700)and Beijing Municipal Scientific and Technological New Star Plan Program (No.2010B052).
10.3969/j.issn.1672⁃6731.2017.05.012
国家重点研发计划项目(项目编号:2016YFC1301700);北京市科技新星计划项目(项目编号:2010B052)
100053 北京,首都医科大学宣武医院神经外科
朱凤水(Email:zhufengshui@sina.com)
2017⁃05⁃02)