腰椎融合与非融合技术治疗单节段腰椎退变性疾病的疗效对比
曹华祁伟 王铮 徐正
(中国人民解放军第三五九医院脊柱关节外科,江苏镇江212001)
腰椎融合与非融合技术治疗单节段腰椎退变性疾病的疗效对比
曹华*祁伟 王铮 徐正
(中国人民解放军第三五九医院脊柱关节外科,江苏镇江212001)
背景:随着人口老年化,腰椎退变性疾病发生率也逐年增加,如何有效治疗此类疾病,学术界尚存争议。目的:比较腰椎融合与非融合技术治疗单节段腰椎退变性疾病的临床疗效。方法:回顾分析97例单节段腰椎退变性疾病患者的临床资料,根据手术方式不同将患者分为采用后路腰椎融合术治疗单节段腰椎退变性疾病组(PLIF组,n=51)和采用Dynesys动态内固定治疗单节段腰椎退变性疾病组(Dynesys组,n=46)。比较两组术后腰痛程度(VAS评分)、临床功能[Oswestry功能障碍指数(Oswestry disability index,ODI)]及术后影像学结果(手术节段椎间隙高度、活动度,上位邻近节段活动度)。结果:PLIF组随访时间28~78个月,平均(48.7±21.8)个月;Dynesys组随访时间27~76个月,平均(48.6±19.7)个月;两组随访时间比较,差异无统计学意义(P>0.05)。末次随访时,两组VAS评分及ODI评分均较术前改善(p<0.05),但组间比较,VAS评分差异无统计学意义(P>0.05),Dynesys组患者ODI评分优于PLIF组(p<0.05)。两组末次随访手术节段椎间隙高度均较术前增高,但PLIF组与术前比较差异无统计学意义(P>0.05),而Dynesys组高于术前(p<0.05)。两组末次随访手术节段活动度均低于术前(p<0.05),Dynesys组由术前6.9°±2.1°降低到4.6°±1.3°,而PLIF组由术前7.2°±2.3°降低到0°。两组末次随访时上位邻近节段活动度均较术前增加(p<0.05),Dynesys组由术前7.8°±1.2°增加到8.6°±1.7°,PLIF组由术前7.1°±2.6°增加到10.8°±2.6°,且组间比较差异有统计学意义(p<0.05)。结论:PLIF与Dynesys动态内固定治疗单节段腰椎退变性疾病均能获得满意的临床疗效,但后者能够部分保留手术节段活动度,且对邻近椎体活动度影响较小,理论上可以降低邻近节段退变。
Dynesys动态内固定;腰椎融合术;腰椎退变性疾病;活动范围,关节
腰椎退变性疾病是引起中老年患者腰腿痛的常见原因,常表现为腰疼、下肢放射性疼痛以及跛行,严重影响患者生活质量[1-3]。目前对其治疗主要采用后路腰椎间融合术(PLIF),但是此方法可导致邻近节段退变,影响长期临床疗效[4-6]。为此,有学者[7-9]建议,采用非融合技术(Dynesys动态内固定)治疗腰椎退变性疾病,以期获得脊柱的稳定,而不改变相邻节段的应力,降低邻近节段的退变。
本研究回顾性分析我院采用PLIF与Dynesys动态内固定治疗单节段腰椎退变性疾病患者的相关临床资料,旨在探讨Dynesys动态内固定治疗单节段腰椎退变性疾病的临床疗效。
1 资料与方法
1.1 临床资料
纳入标准:①年龄>55岁;②患有单节段腰椎退变性疾病;③经正规保守治疗>6个月,临床症状没有明显改善;④由同一医师进行手术。排除标准:①峡部裂导致腰椎滑脱者;②多节段病变者;③手术节段有手术史者;④腰椎退变性滑脱>3度者;⑤资料不完整者。
选择2006年7月至2012年7月于我院行手术治疗的97例单节段腰椎退变性疾病患者,根据手术方式不同分为两组:采用后路腰椎体间融合术治疗组(PLIF组),共51例,其中,男23例、女28例;年龄57~78岁,平均(62.8±8.7)岁;BMI 19.8~30.1 kg/m2,平均(23.7±4.6)kg/m2;术前ASA分级,1级23例、2级26例、3级2例;术前诊断腰椎退变性管狭窄患者29例、腰椎退变性滑脱患者12例、腰椎退变性不稳患者10例;术前腰疼VAS评分7~10分,平均(8.2±3.1)分;采用Dynesys内固定治疗组(Dynesys组),共46例,其中,男21例、女25例;年55~76岁,平均(61.9±11.3)岁;BMI 20.7~29.8 kg/m2,平均(23.8±5.1)kg/m2;术前ASA分级,1级26例、2级19例、3级1例;术前诊断腰椎退变性管狭窄患者25例、腰椎退变性滑脱患者11例、腰椎退变性不稳患者10例;术前腰疼VAS评分7~10分,平均(8.1±2.3)分。两组术前临床资料比较,差异无统计学意义(P>0.05,表1)。
1.2 手术方法及术后处理
Dynesys组:采用全身麻醉,俯卧位下手术,作后纵中切口,长约10 cm,逐层切开,分离椎旁肌,显露病变节段两侧上下椎体关节突,透视下确定椎弓根螺钉进针点,拧入椎弓根螺钉。部分咬除椎板,切除黄韧带,显露神经根及硬脊膜,行侧隐窝减压,探查神经根及椎间孔见减压彻底,切开纤维环,取出髓核及病变的椎间盘组织。测量椎弓根螺钉间距,取适宜长度的椎间管状袖套,将聚对苯二甲酸乙二酯带套入管状袖套与上下椎弓根螺钉之间,收紧多聚酯纤维带,使小螺钉紧固。冲洗切口,放置引流管,缝合切口。
表1 两组术前临床资料比较
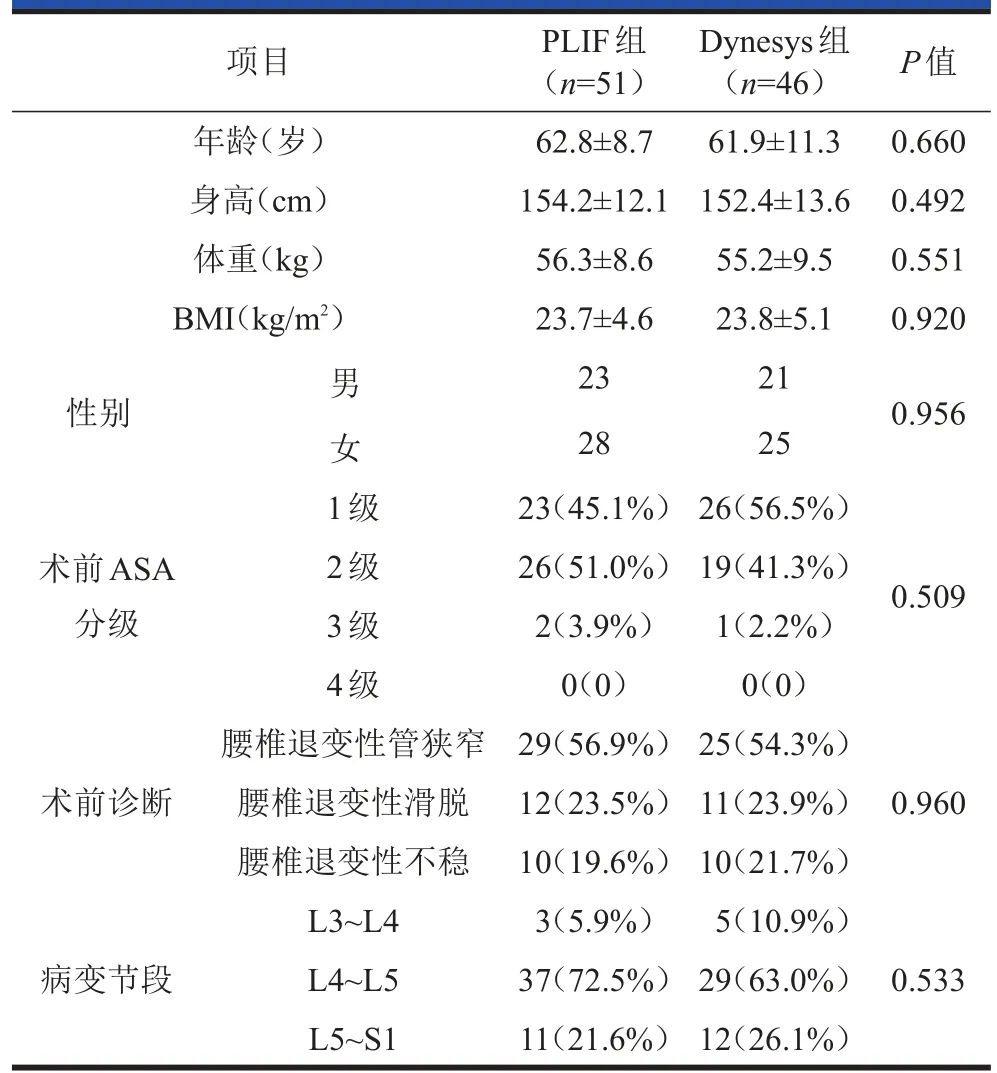
表1 两组术前临床资料比较
项目年龄(岁)身高(cm)体重(kg)BMI(kg/m2)P值0.660 0.492 0.551 0.920性别男女1级0.956术前ASA分级0.509术前诊断0.960病变节段2级3级4级腰椎退变性管狭窄腰椎退变性滑脱腰椎退变性不稳L3~L4 L4~L5 L5~S1 PLIF组(n=51)62.8±8.7 154.2±12.1 56.3±8.6 23.7±4.6 23 28 23(45.1%)26(51.0%)2(3.9%)0(0)29(56.9%)12(23.5%)10(19.6%)3(5.9%)37(72.5%)11(21.6%)Dynesys组(n=46)61.9±11.3 152.4±13.6 55.2±9.5 23.8±5.1 21 25 26(56.5%)19(41.3%)1(2.2%)0(0)25(54.3%)11(23.9%)10(21.7%)5(10.9%)29(63.0%)12(26.1%)0.533
PLIF组:采用与Dynesys组相同的手术方法行椎弓根螺钉固定、椎管减压及切除病变的椎间盘,然后行椎间植骨及置入Cage椎间融合器,冲洗切口,放置引流管,缝合切口。
术后处理:两组患者均预防性使用抗生素2天,引流管术后48 h拔除,术后2天鼓励患者在脊柱支具固定下下地活动。
1.3 随访计划及评价指标
采用VAS评分评估术后腰痛程度、采用Oswestry功能障碍指数(Oswestry disability index,ODI)评估临床功能,记录术后影像学结果所示的手术节段椎间隙高度、活动度、上位邻近节段活动度,并对两组的上述指标进行比较。出院后要求患者于术后第3个月、6个月、1年进行门诊随访,以后每年随访1次。
1.4 统计学方法
采用SPSS 18.0软件进行统计学分析。计量资料以均数±标准差表示,连续变量组间比较采用t检验。分类变量组间比较采用χ2检验。融合率及并发症发生率采用Fisher精确检验。以p<0.05为有统计学差异。
2 结果
PLIF组随访时间28~78个月,平均(48.7±21.8)个月;Dynesys组随访时间27~76个月,平均(48.6±19.7)个月;两组随访时间比较,差异无统计学意义(P>0.05)。末次随访时,两组VAS评分及ODI均较术前改善(p<0.05),但组间比较,VAS评分差异无统计学意义(P>0.05),而Dynesys组ODI评分优于PLIF组(p<0.05,表2)。两组末次随访时手术节段椎间隙高度均较术前升高,但PLIF组与术前比较,差异无统计学意义(P>0.05),而Dynesys组较术前升高(p<0.05,表3)。两组末次随访时手术节段活动度均低于术前(p<0.05,表4)。两组末次随访时上位邻近节段活动度均较术前增加(p<0.05),且组间比较差异有统计学意义(p<0.05,表5)。典型病例见图1、2。
3 讨论
腰椎退变性疾病主要发生机制是随着患者年龄的增加,腰椎间盘退变,导致腰椎节段性不稳,相应的小关节突应力增加,导致关节突关节退变,影像学检查可见椎间隙高度下降、椎体周围边缘骨赘增生、小关节突增生肥大等[10,11]。本研究中,所有患者术前平均椎间隙高度均<5 mm。这些增生的骨赘发生在椎体后缘、关节突内侧面,可导致椎管狭窄、神经根管狭窄等,引起一系列的腰腿疼痛症状。临床常需要手术行狭窄段椎板及神经根管减压,但是单纯减压将进一步导致腰椎不稳,因此传统上对于腰椎退变性疾病,在减压的同时行椎体间融合,以增加脊椎的稳定性[12,13]。
尽管腰椎融合术治疗方法较多,但PLIF技术在临床中较常用,相比其他的融合技术,该技术的融合率更佳[14]。但是PLIF也存在一些局限性,如加速邻近节段的退变,关节突增生、椎间融合器移位等,从而引起一系列腰部不适症状[15]。随着研究的不断深入,学者发现,非融合技术似乎具有更佳的临床疗效。本研究表明,相比PLIF治疗腰椎退变性疾病,Dynesys组ODI评分明显优于PLIF组,同时Dynesys组术后手术节段椎间活动度得以大部分保留,邻近节段活动度增幅较小,这些均有利于降低术后相邻脊椎节段的应力,从而降低退变发生。本研究在一定程度上证明了使用非融合技术治疗腰椎退变性疾病具有较好的临床疗效。相比PLIF,非融合技术术后护理较容易,有利于患者术后康复。
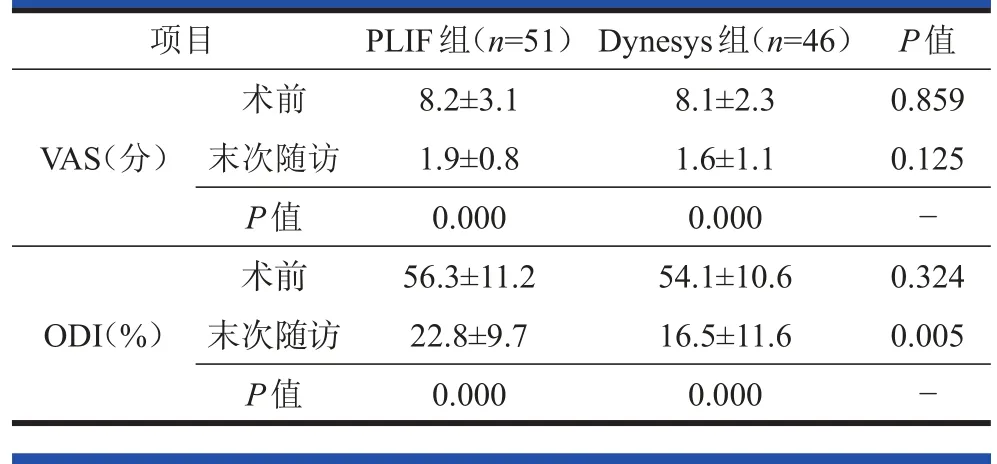
表2 两组术前及末次随访时VAS、ODI比较(x±s)
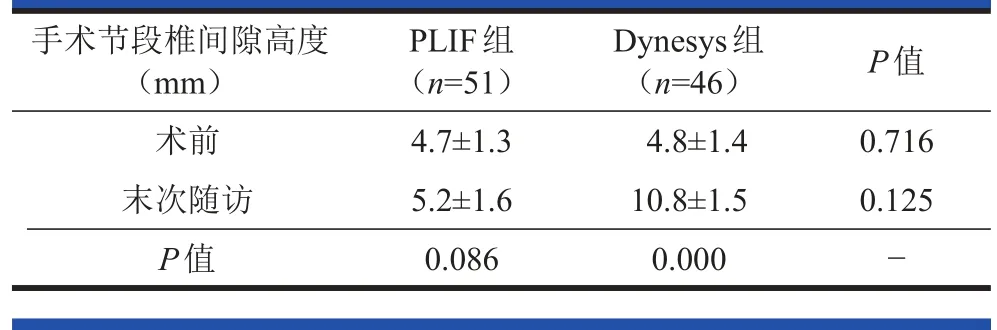
表3 两组术前及末次随访时手术节段椎间隙高度比较(x±s)
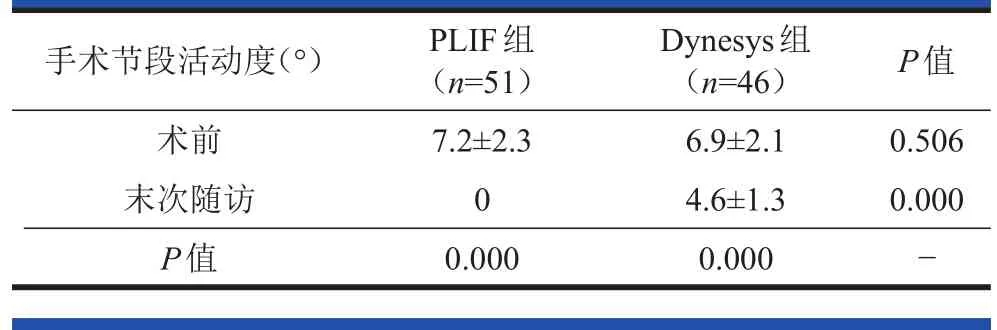
表4 两组术前及末次随访时手术节段活动度比较(x±s)
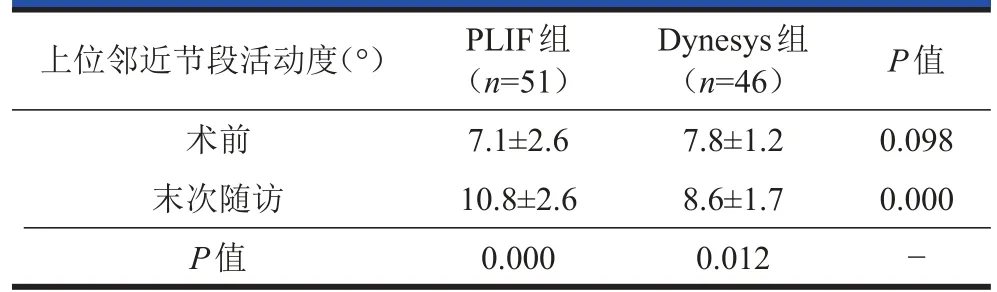
表5 两组术前及末次随访时上位邻近节段活动度比较(x±s)
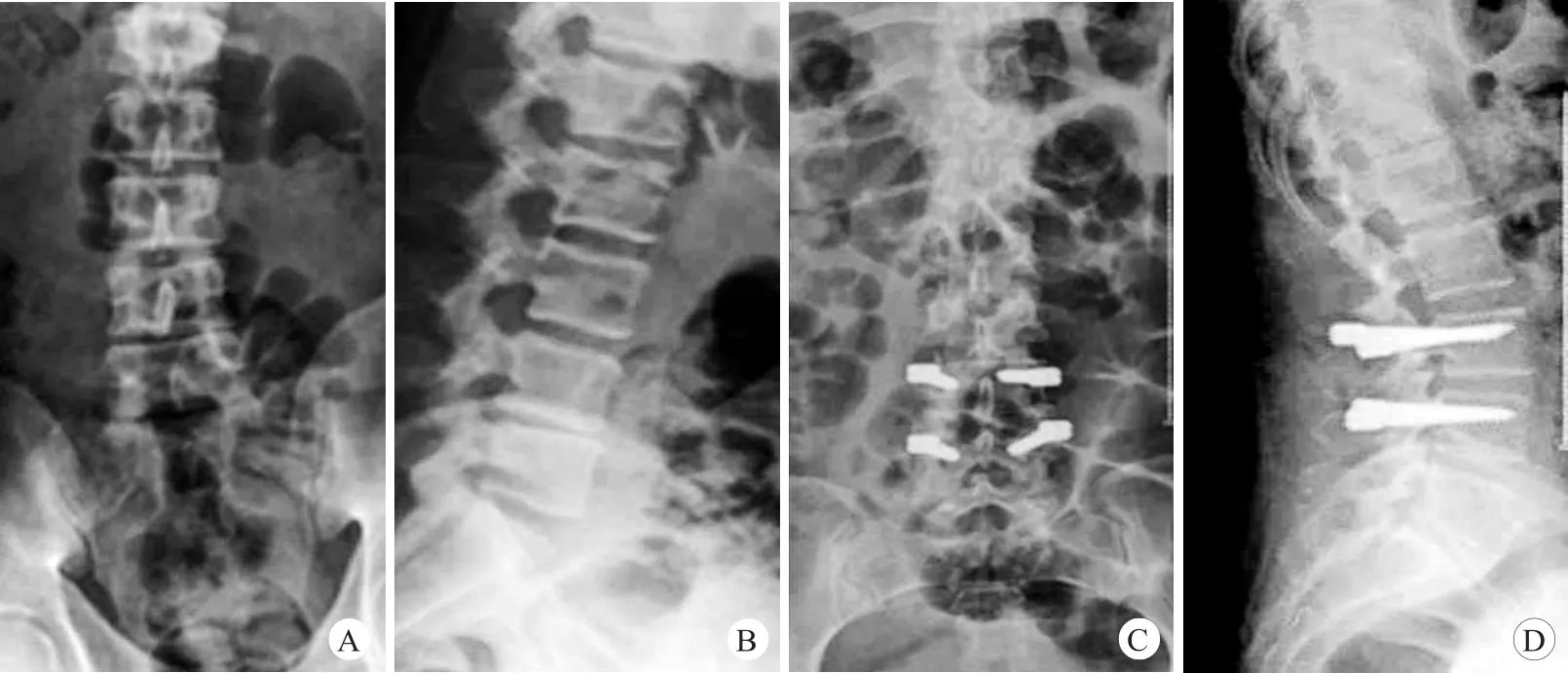
图1 患者,女,54岁,因L4-5椎间隙退变性疾病,采用Dynesys动态内固定治疗A、B.术前正侧位X线片;C、D.末次随访时正侧位X线片
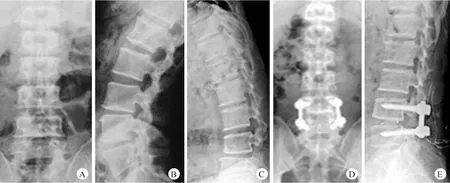
图2 患者,女,63岁,因L4椎体退变性不稳,采用后路腰椎融合术A-C.术前正位、后伸位及前曲位X线片;D、E.末次随访时正侧位X线片示椎间融合
综上所述,PLIF与Dynesys动态内固定治疗单节段腰椎退变性疾病均能获得满意的临床疗效,但后者能够部分保留手术节段活动度,且对邻近椎体活动度影响较小,理论上可以降低邻近节段退变。然而,本研究也存在例数较少、随访时间较短等不足之处。
[1]Guentchev M,Peter L,Preuss C,et al.Dynamic intraspinous stabilization reduces spinal mobility after bilateral laminotomy.J Spine,2017,6(366):2.
[2]Yang S,Liu Y,Bao Z,et al.Comparison of adjacent segment degeneration after nonrigid fixation system and posterior lumbar interbody fusion for single-level lumbar disc herniation:A new method of MRI analysis of lumbar nucleus pulposus volume.J Invest Surg,2017,19:1-6.
[3]Triebel J,Snellman G,Sandén B,et al.Women do not fare worse than men after lumbar fusion surgery:Two-year follow-up results from 4,780 prospectively collected patients in the Swedish National Spine Register with lumbar degenerative disc disease and chronic low back pain.Spine J,2017,17(5):656-662.
[4]Tsai TT,Tai CL,Ho NY,et al.Effects of strontium ranelate on spinal interbody fusion surgery in an osteoporotic rat model.PLoS One,2017,12(1):e0167296.
[5]Yavin D,Casha S,Wiebe S,et al.Lumbar fusion for degenerative disease:A systematic review and meta-analysis.Neurosurgery,2017,80(5):701-715.
[6]VonderHoeh NH,Voelker A,Heyde CE.Results of lumbar spondylodeses using different bone grafting materials after transforaminal lumbar interbody fusion(TLIF).Eur Spine J,2017,May 25.[Epub ahead of print].
[7]Huang YJ,Zhao SJ,Zhang Q,et al.Comparison of lumbar pedicular dynamic stabilisation systems versus fusion for the treatment of lumbar degenerative disc disease:A metaanalysis.Acta Orthopædica Belgica,2017,83(1):180-193.
[8]尚凯,陈铭吉,王德国.椎旁肌间隙入路经椎弓根动态稳定固定结合经关节突减压治疗腰椎退行性病变的疗效观察.中华医学杂志,2017,97(19):1496-1501.
[9]Goldstein IM,Singh R,Agarwal N.Resolution of screw radiolucency following instrumentation with a hybrid rigid to dynamic stabilization system.Interdisciplinary Neurosurgery,2017,9:71-75.
[10]唐金平,刘晓岚,陈群.退变性腰椎侧凸的影像学和临床特点的相关性研究.实用骨科杂志,2016,22(2):134-138.
[11]Albert HB.Antibiotic treatment of patients with chronic low back pain and Modic changes.Schmerzmedizin,2017,33(2):49-52.
[12]杨勇,王清,徐双,等.单侧椎板间扩大开窗所获自体骨行腰椎椎间融合的可行性.中国脊柱脊髓杂志,2017,27(2):142-148.
[13]汤旭日,马安军,傅弛,等.单侧椎弓根螺钉固定联合TLIF行腰椎融合术的中期疗效.中国矫形外科杂志,2017,25(5):410-415.
[14]Audat Z,Moutasem O,Yousef K,et al.Comparison of clinical and radiological results of posterolateral fusion,posterior lumbar interbody fusion and transforaminal lumbar interbody fusion techniques in the treatment of degenerative lumbar spine.Singapore Med J,2012,53(3):183-187.
[15]Sehulte TL,Leistra F,Bullmann V,et a1.Disc height reduction in adjacent segments and clinical outcome 10 years after lumbar 360 degrees fusion.Eur Spine J,2007,16(12):2152-2158.
Comparison of clinical effect of lumbar fusion and non-fusion in treatment of single segmental lumbar degenerative disease
CAO Hua*,QI Wei,WANG Zheng,XU Zheng
(Department of Spinal&Joint Surgery,No.359th Hospital of PLA,Zhenjiang 212001,Jiangsu,China)
Background:With the aging of population,the incidence of lumbar degeneration is increasing year by year.How to effectively treat such diseases is controversial.Objective:To compare the clinical efficacy of lumbar fusion and nonfusion in treatment of single segmental lumbar degenerative disease.Methods:A total of 97 patients with single segmental lumbar degenerative disease were selected and divided into two groups according to surgical procedures.Of them,51 patients were treated with posterior lumbar interbody fusion(PLIF group)and 46 were treated with Dynesys dynamic internal fixation(Dynesys group).Postoperative back pain(VAS score),clinical function(ODI score)and radiographic results(height and range of motion of intervertebral space of surgical segment,range of motion of upper adjacent segment)were compared between the two groups.Results:The mean duration of follow-up was(48.7±21.8)months in PLIF group(range,28-78 months)and(48.6±19.7)months in Dynesys group(range,27-76 months,P>0.05).At the final follow-up,both VAS and ODI were improved significantly when compared with preoperative ones(p<0.05),but there was no significant difference in VAS score between the two groups(P>0.05),and patients in Dynesys group had a lower ODI than those in PLIF group(p<0.05).The height of surgical segment intervertebral space increased at the final follow up in both groups.Compared with preoperative one,the height of surgical segment intervertebral space was significantly increased in Dynesys group(p<0.05)at the final follow up,but no significant difference was found in PLIF group(P>0.05).Range of motion of surgical segment was significantly lower at final follow up than that before surgery in both Dynesys group(6.9°±2.1°vs 4.6°±1.3°)and PLIF group(7.2°±2.3°vs 0°,p<0.05).Range of motion of upper adjacent segment was significantly higher at final follow up than that before surgery in both Dynesys group(7.8°±1.2°vs 8.6°±1.7°)and PLIF group(7.1°±2.6°vs 10.8°±2.6°,p<0.05).Conclusions:Both of PLIF and Dynesys dynamic internal fixation have a satisfactory effect on single segmental lumbar degenerative disease,however,Dynesys dynamic internal fixation can partially maintain range of motion of surgical segment,has less impact on range of motion of the adjacent vertebra,and can theoretically reduce adjacent segment degeneration.
Dynesys Dynamic Internal Fixation;Lumbar Fusion;Lumbar Degenerative Diseases;Range of Motion,Joint
2095-9958(2017)08-0 308-04
10.3969/j.issn.2095-9958.2017.04-08
*通信作者:曹华,E-mail:caohuaauu@163.com

