经皮加压钢板与空心钉治疗股骨颈骨折的临床疗效比较*
叶俊星,戴涟生,王松华,张斌,杨晓斐,吴红富,程飞,杨志刚,袁凤来
(江苏省无锡市第三人民医院,江苏 无锡 214000)
经皮加压钢板与空心钉治疗股骨颈骨折的临床疗效比较*
叶俊星,戴涟生,王松华,张斌,杨晓斐,吴红富,程飞,杨志刚,袁凤来
(江苏省无锡市第三人民医院,江苏 无锡 214000)
目的 比较经皮加压钢板和空心螺钉治疗股骨颈骨折的临床疗效。方法 选取2012~2015年来该院采用经皮加压钢板(PCCP)治疗股骨颈骨折病例32例,与同期采用空心螺钉固定的股骨颈骨折32例进行随访比较。PCCP组,男性14例,女性18例;平均年龄42.5岁(27~59岁);车祸伤20例,跌伤10例,高处坠落伤2例;均为闭合性骨折,无明显合并症;Garden分型,Ⅰ型3例,Ⅱ型5例,Ⅲ18例,Ⅳ型6例。空心钉组,男性20例,女性12例;平均年龄43.3岁(23~61岁);车祸伤22例,跌伤10例;均为闭合性骨折,无明显合并症;Garden分型,Ⅰ型4例,Ⅱ型9例,Ⅲ17例,Ⅳ型2例。对两组患者的手术时间、住院时间、骨折愈合时间、Harris髋关节功能评分进行比较,并进行统计学分析。结果 两组患者住院时间、骨折愈合时间、Harris髋关节功能评分比较,差异无统计学意义(P>0.05),但PCCP组并发症更少,差异有统计学意义(P<0.05)。结论 PCCP可使骨折端加压,但又控制过度压缩,钉板结合可防止颈干角丢失,两枚螺钉固定具有抗旋转能力,是治疗股骨颈骨折的一种疗效确切的方法。
股骨颈骨折;经皮加压钢板;空心螺钉
股骨颈骨折是临床上的常见骨折,约占全身骨折的3.6%、髋部骨折的53%~56%[1-2]。对于老年患者常采用人工关节置换术,而对于青壮年患者,临床则倾向于内固定治疗。但临床报道,内固定治疗股骨颈骨折后骨不愈合的发生率约为8.9%~40%[3-5],股骨头坏死发生率约为10%~43%[4,6-7]。因此,其常被称为“尚未被解决的骨折”[6]。其治疗方法多样,目前公认的是空心螺钉固定,但由于股骨颈骨折常涉及高能量损伤,骨折端局部多存在粉碎或移位,使用空心钉固定过程中,常出现骨折再移位、骨不连、内固定失效、退钉等情况,有着一定的局限性。本研究组经过多年临床实践,应用经皮加压钢板(percutaneous compression plating,PCCP)治疗股骨颈骨折,疗效确切,现报道如下。
1 资料与方法
1.1 一般资料
选取2012~2015年来江苏省无锡市第三人民医院骨科采用PCCP治疗股骨颈骨折病例32例,与同期采用空心螺钉固定的股骨颈骨折32例进行随访比较。PCCP组,男性14例,女性18例;平均年龄42.5岁(27~59岁);车祸伤20例,跌伤10例,高处坠落伤2例;均为闭合性骨折,无明显合并症;Garden分型,Ⅰ型3例,Ⅱ型5例,Ⅲ18例,Ⅳ型6例。空心螺钉组,男性20例,女性12例;平均年龄43.3岁(23~61岁);车祸伤22例,跌伤10例;均为闭合性骨折,无明显合并症;Garden分型,Ⅰ型4例,Ⅱ型9例,Ⅲ17例,Ⅳ型2例。两组病例一般资料比较差异无统计学意义(P>0.05),具有可比性。
1.2 手术过程
1.2.1 术前准备 所有患者入院后予以胫骨结节牵引,完善相关检查,排除手术禁忌,合并内科基础病者请相关科室会诊,请麻醉科评估手术风险。术中给予硬膜外或硬腰联合麻醉,有禁忌证者采用全身麻醉。
1.2.2 PCCP组 在C臂机透视下牵引床复位骨折断端,位置良好后,在股骨大粗隆下切一2 cm左右的切口,分离至股骨粗隆下,将钢板从切口处插入,依靠钢板远端分离骨与软组织,使钢板与股骨近端安放服贴,矫正钢板位置良好后,1枚定位针固定钢板近端。于钢板中远端切一2 cm左右的切口,抓钳固定钢板,打入股骨颈下方1枚导针,正侧位透视良好后,打入第1枚股骨颈螺钉,依次将第2枚股骨颈螺钉和3枚股骨干螺钉固定,彻底冲洗并关闭切口。见图1。
1.2.3 空心螺钉组 在C臂机透视下牵引床复位骨折断端,位置良好后,闭合按照倒三角形打入3枚导针,然后拧入3枚空心螺钉。
1.3 术后处理
两组患者第2天开始下肢肌肉主动收缩锻炼,促进下肢血液循环及患肢功能恢复,预防深静脉血栓形成。疼痛肿胀减轻后仰卧位屈膝屈髋抬腿锻炼,逐渐取半卧位、坐位。2周后拄拐下地活动,术后8~10周患肢负重,逐渐增加。12~16周后复查X线片,骨折愈合后,逐渐全负重活动。
1.4 观察指标
每例患者分别于术后1、2、3、6和12个月各复查一次X线,以后视情况决定复查时间。观察两组患者住院时间、骨折愈合时间、Harris髋关节功能评分、内固定有无松动、股骨颈短缩、颈干角丢失等情况。两组病例随访16~32个月,平均21个月。所有患者均在最后一次随访时进行Harris髋关节功能评分。
1.5 统计学方法
应用SPSS13.0统计软件进行数据分析,数据采用均数±标准差(±s)表示,采用成组t检验,计数资料采用χ2检验,P<0.05为差异有统计学意义。
2 结果
所有患者均得到随访,两组患者住院时间、骨折愈合时间、Harris髋关节功能评分,差异无统计学意义(P>0.05),两组患者疗效相近,见表1。但空心螺钉组存在2例退钉、股骨颈短缩,1例出现颈干角变小,而PCCP组未出现螺钉松动,退钉,颈干角变小等现象,见表2。PCCP组术后复查X片见图2。
表1 两组患者术后随访情况 (n=32,±s)
组别骨折愈合/周7 ± 3 . 2 7 1 3 . 7 2 ± 2 . 8 4 7 ± 3 . 1 6 1 4 . 5 3 ± 3 . 3 2 t值末次H a r r i s评分/分P C C P组 9 2 . 2 9 ± 6 . 1 4空心螺钉组 8 9 . 5 1 ± 6 . 3 7住院时间/ d 0 . 9 2 2 0 . 7 1 3 P值 0 . 3 6 3 0 . 4 8 1 0 . 8 7 9 0 . 1 5 4
表2 两组并发症比较 (n=32,±s)
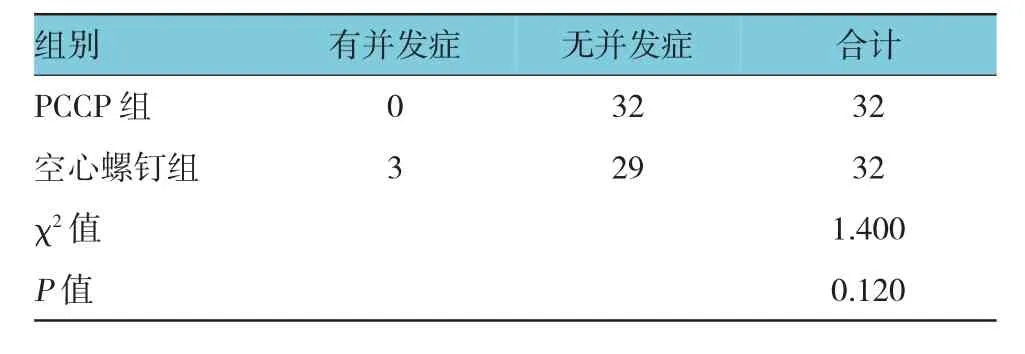
表2 两组并发症比较 (n=32,±s)
组别无并发症0 3 2 3 2 9 χ2值合计P C C P组 3 2空心螺钉组 3 2有并发症1 . 4 0 0 P值 0 . 1 2 0

图2PCCP组术后复查X线
3 讨论
对于股骨颈骨折的内固定,钉板系统出现于20世纪50年代,包括动力髋螺钉(DHS)、Richard钉和螺旋刀片型DHS[8-10],其主要原理是当骨折面发生吸收时,固定钉沿套筒滑动,使骨折端保持紧密接触,有利于骨折愈合;术后早期负重使这种接触更加紧密,以促进骨折愈合[8,11],迄今仍在临床上应用。CHEN等[12]报道了241例单侧新鲜股骨颈基底部骨折患者经闭合复位DHS内固定后,仅有5例(1.66%)出现骨折不愈合,2例(0.83%)发生断钉,其余患者均固定稳定,疗效明显,术后14~24周骨折愈合良好,无股骨头坏死发生。有报道显示[13]DHS内固定有角稳定作用,对于有移位的不稳定型股骨颈骨折(GardenⅢ或Ⅳ型),特别是Pauwels角度较大的股骨颈骨折的效果比单纯空心螺钉固定相对较好,两者骨不连发生率分别为8%和19%。单用钉板系统的效果较差,在DSH上方加拧1枚松质骨螺钉可增加其抗扭转能力,降低骨折断端移位风险,所以2枚主钉较1枚主钉固定更加可靠,而PCCP有2枚主钉,固定较1枚主钉更加可靠。
即使采用空心加压螺钉固定,从生物力学强度看,2枚空心加压螺钉固定与3枚空心加压螺钉固定在抗垂直载荷方面无明显区别。一些学者[14-15]认为,第3枚空心加压螺钉固定并非必要。然而在2枚空心加压螺钉固定时,Pauwels角较大的股骨颈骨折前后方向的弯曲载荷所致应变,明显高于Pauwels角较小时的情况。从螺钉固定布局看,2枚螺钉以水平方位固定股骨颈骨折比以垂直方位固定者可提供更好的固定效果[16]。而3枚空心螺钉正三角内固定,还有造成医源性粗隆下骨折的风险。PCCP正是由2枚主钉以平行方向固定股骨颈骨折,具有良好的骨折端加压,抗旋转作用。ZHE等[17]运用PCCP治疗股骨颈骨折,并进行平均18.8个月的随访,认为PCCP是一种稳定的具有抗轴向和旋转应力的内固定装置。运用PCCP治疗股骨颈骨折,具有较低的骨折不愈合和股骨头缺血性坏死的发生率。
PCCP属于髋部钉板系统[18],它是在DHS的基础上研制出的一种新型经皮微创加压钢板系统,该系统由1块钢板、2枚股骨颈螺钉、3枚股骨干螺钉组成,手术过程中采用闭合复位,钢板经皮插入,不暴露骨折端,减少软组织的剥离及术中出血[19-24]。可滑动的颈钉既能提供微动环境,可控制骨折端的过度压缩,又可使骨折处得到加压,促进骨折生长,避免了螺钉的退钉、松动等情况[25],固定可靠,具有空心螺钉没有的优越性。股骨颈内打入的2枚螺钉,增加了抗旋转力量,提供了额外的骨折端稳定性。颈钉套筒与钢板之间锁定,整体稳定性强。朱峰等[26]通过对74例股骨颈骨折患者采用闭合复位PCCP内固定治疗,末次随访Harris评分(92.9±5.0)分,优良率99%,其中65例能独立行走,1例需扶拐行走,部分负重时间(3.6±1.7)d,完全负重时间(2.1±1.4)个月,骨折临床愈合时间(3.9±1.6)个月,无不愈合。他们认为PCCP治疗股骨颈骨折具有创伤小、固定牢固、患者术后可早期负重、功能恢复佳、并发症少等优点。
本研究通过对PCCP内固定和空心螺钉内固定治疗股骨颈骨折的临床疗效比较,两组患者住院时间、骨折愈合时间、Harris髋关节功能评分,差异无统计学意义,两组患者疗效相近,但PCCP组并发症更少。笔者认为PCCP内固定具有与空心螺钉相同的疗效,且固定可靠,抗剪切力强,更好地避免了退钉、松动等情况,是临床治疗股骨颈骨折,尤其是不稳定型骨折的一种良好的选择。当然本研究因为病例相对较少,缺乏大样本病例随访,具有一定的局限性,但这并不能影响其在治疗股骨颈骨折中的巨大潜力。
[1]WILK R,SKRZYPEK M,KOWALSKA M,et al.Standardized incidence and trend of osteoporotic hip fracture in polish women and men:a nine year observation[J].Maturitas,2013,77(1):59-63.
[2]BRODERICK J M,BRUCE-BRAND R,STANLEY E,et al.Osteoporotic hip fractures:the burden of fixation failure[J].Sci World J,2013,51(5):1-7.
[3]VAN MUST A B.Femoral neck non-unions:how do I do it?[J]. Injury,2007,38(Suppl 2):S51-S54.
[4]DAMANY D S,PARKER M J,CHOJNOWSKI A.Complications after intracapsular hip fractures in young adults.A meta-analysis of 18 published studies involving 564 fractures[J].Injury,2005, 36(1):131-141.
[5]FRIHAGEN F,FIGVED W,MADSEN J E,et al.The treatment of femoral neck fractures[J].Tidsskr Nor Laegeforen,2010,130 (16):1614-1617.
[6]SU Y,CHEN W,ZHANG Q,et al.An irreducible variant of femoral neck fracture:a minimally traumatic reduction technique[J].Injury,2011,42(2):140-145.
[7]MITTAL R,GLASGOW M,BANERJEE S.Proximal femoral fracture:principles of management and review of literarure[J].J Clin Orthop Trauma,2012,3(1):15-23.
[8]GOLDSTEIN C,PETRESOR B A,FERGUSON T,et al.Evidence-based medicine:implantsforfixation offemoralneck fractures[J].Tech Orthop,2008,23(4):301-308.
[9]WINDOLF M,BRAUNSTEIN V,DUTOIT C,et al.Is a helical shaped implant a superior alternative to the dynamic hip screw for unstable femoral neck fractures?Abiomechanical investing ation[J].Clin Biomech,2009,24(1):59-64.
[10]LAGERBY M,ASPLUND S,RINGQVIST I.Cannulated screws for fixation of femoral neck fractures.No difference between Uppsala screws and Richards screws in a randomized prospective study of 268 cases[J].Acta Orthop Scand,1998,69(4): 387-391.
[11]BRANDT E,VERDONSCHOT N,VAN VUGT A,et al.Biomechanical analysis of the percutaneous compression plate and sliding hip screw in intracapsular hip fractures:experimental assessment using synthetic and cadaver bones[J].Injury,2006,37 (10):979-983.
[12]CHEN C Y,CHIU F Y,CHEN C M,et al.Surgical treatment of basicervical fractures of femur:a prospective evaluation of 269 patients[J].J Trauma,2008,64(2):427-429.
[13]LIPORACE F,GAINES R,COLLINGE C,et al.Results of internal fixation of pauwells type-3 vertical femoral neck fractures[J].J Bone Joint Surg Am,2008,90(80):1654-1659.
[14]WALKER E,MUKHER JEE D P,OGDEN A L,et al.A biomechanical studay of simulated femoral neck fracture fixation by cannulated screws:effects of placement angle and number of screws[J].Am J Orthop,2007,36(12):680-684.
[15]MAURER S G,WRIGHT K E,KUMMER F J,et al.Two or three screws for fixation of femoral neck fractures[J].Am J Orthop,2003,32(9):438-442.
[16]TAN V,WONG K L,BORN C T,et al.Two-screw femoral neck fracture fixation:a biomechanical analysis of 2 different configurations[J].Am J Orthop,2007,36(9):481-485.
[17]ZHE F,LIU G,SHAO H G,et al.Treatment of femoral neck fracture with percutaneous compression plate:preliminary results in 74 patients[J].Orthopaedic Surgery,2015,7(2):132-137.
[18]GOTFRIED Y.Percutaneous compression plating of intertrochanteric hip fractures[J].J Orthop Trauma,2000,14(7):490-495.
[19]VARELA-EGOCHEAGA J R,IGLESIAS-COLAO R,SUAREZSUAREZ M A,et al.Minimally invasive osteosynthesis in stable trochanteric fractures:a comparative study between Gotfried percutaneous compression plate and Gamma 3 intramedullary nail[J].Arch Orthop Trauma Surg,2009,129(10):1401-1407.
[20]PEYSER A,WEIL Y A,BROCKE L,et al.A prospective,randomised study comparing the percutaneous compression plate and the compression hip screw forthe treatmentofintertrochanteric fractures of the hip[J].J Bone Joint Surg Br, 2007,89(9):1210-1217.
[21]YANG E,QURESHI S,TROKHAN S,et al.Gotfried percutaneous compression plating compared with sliding hip screw fixation of intertrochanteric hip fractures:a prospective randomized study[J].J Bone Joint Surg Am,2011,93(10):942-947.
[22]CRESPO E,GALVEZ J,TEN A J,et al.A comparative study between gamma nail and percutaneous compression plating for the treatment of intertrochanteric hip fractures[J].Eur J Trauma Emerg Surg,2012,38(4):443-449.
[23]CHENG T,ZHANG G Y,LIU T,et al.A meta-analysis of percutaneous compression plate versus sliding hip screw for the management of intertrochanteric fractures of the hip[J].J Trauma Acute Care Surg,2012,72(5):1435-1443.
[24]MA J,XING D,MA X,et al.The percutaneous compression plate versus the dynamic hip screw fortreatmentofintertrochanteric hip fractures:a systematic review and meta-analysis of comparative studies[J].Orthop Traumatol Surg Res,2012, 98(7):773-783.
[25]王飞,庞军,郭开今,等.PCCP与PFNA内固定股骨粗隆间骨折的疗效对比[J].中国骨与关节损伤杂志,2012,27(6):532-533.
[26]朱峰,徐耀增,耿德春,等.经皮加压钢板治疗股骨颈骨折的早期疗效[J].中华创伤杂志,2014,30(9):909-912.
(张蕾 编辑)
Clinical curative effect of percutaneous compression plating and cannulated screw for treatment of femoral neck fractures*
Jun-xing Ye,Lian-sheng Dai,Song-hua Wang,Bin Zhang,Xiao-fei Yang, Hong-fu Wu,Fei Cheng,Zhi-gang Yang,Feng-lai Yuan
(The Third People's Hospital of Wuxi,Wuxi,Jiangsu 214000,China)
Objective To compare the clinical effect of percutaneous compression plate(PCCP)and cannulated screw for treatment of femoral neck fractures.Methods From 2012 to 2015,32 cases of femoral neck fracture were treated with PCCP (PCCP group)and 32 cases were treated with cannulated screw(cannulated screw group)in our hospital.In the PCCP group,there were 14 males and 18 females with the average age of 42.5 y;the patients had closed fractures due to traffic accidents(20 cases),tumble(10 cases),or falling from height(2 cases)without obvious complications;for Garden typing,there were 3 cases of typeⅠ,5 cases of typeⅡ,18 cases of typeⅢand 6 cases of typeⅣ.In the cannulated screw group,there were 20 males and 12 females with the average age of 43.3 y;the patients had closed fractures due to traffic accident(22 cases)or tumble (10 cases),there were no obvious complications;for Garden typing,there were 4 cases of type I,9 cases of typeⅡ,17 cases of typeⅢand 2 cases of typeⅣ.The operation time,duration of hospital stay,fracture healing time and Harris hip function score were compared between the two groups,and statistical analyses were performed.Results The hospital time,fracture healing time and Harris hip function score had no statistical differences between the two groups(P>0.05);but the PCCP group had fewer complications than the cannulated screw group(P<0.05).Conclusions PCCP can pressurize the fracture ends,but avoid excessive compression.Nail and plate combination can prevent the loss of neck stem angle.Two-screw
fixation can resist rotation.Therefore,PCCP is an effective curative method for the treatment of femoral neck fracture.
femoral neck fracture;PCCP;cannulated screw
R683
A
2017-02-28
国家自然科学基金(No:82170011);江苏省自然科学基金(No:BK20151114)
袁凤来,E-mail:bjjq88@163.com;Tel:0510-8260332
10.3969/j.issn.1005-8982.2017.19.009
1005-8982(2017)19-0045-04