不同剂量阿托伐他汀治疗冠心病心力衰竭有效性及安全性的对比研究
张淑平,刘宏颖,袁百祥,那雪峰,张小章
·疗效比较研究·
不同剂量阿托伐他汀治疗冠心病心力衰竭有效性及安全性的对比研究
张淑平,刘宏颖,袁百祥,那雪峰,张小章
目的 比较不同剂量阿托伐他汀治疗冠心病心力衰竭的有效性及安全性。方法 选取2014年9月—2016年12月遵化市人民医院收治的冠心病心力衰竭患者165例,采用随机数字表法分为A、B、C 3组,每组55例。在常规治疗基础上,A、B、C组患者分别给予小剂量阿托伐他汀(10 mg/次,1次/d)、中剂量阿托伐他汀(20 mg/次,1次/d)、大剂量阿托伐他汀(40 mg/次,1次/d);3组患者均连续治疗12周。比较3组患者治疗前后心室重构指标、血脂指标及血浆氨基末端脑钠肽前体(NT-proBNP)、超敏C反应蛋白(hs-CRP)水平,并观察3组患者治疗期间不良反应发生情况。结果 治疗前3组患者左心室舒张末期内径(LVEDD)、左心室收缩末期内径(LVESD)及左心室射血分数(LVEF)比较,差异均无统计学意义(P>0.05);治疗后B、C组患者LVEDD和LVESD小于A组,LVEF高于A组(P<0.05);治疗后C组患者LVEDD和LVESD小于B组,LVEF高于B组(P<0.05)。治疗前3组患者三酰甘油(TG)、总胆固醇(TC)、低密度脂蛋白胆固醇(LDL-C)比较,差异均无统计学意义(P>0.05);治疗后B、C组患者TG、TC、LDL-C水平低于A组,C组患者TG、TC、LDL-C水平低于B组(P<0.05)。治疗前3组患者血浆NT-proBNP和hs-CRP水平比较,差异均无统计学意义(P>0.05);治疗后B、C组患者血浆NT-proBNP和hs-CRP水平低于A组,C组患者血浆NT-proBNP和hs-CRP水平低于B组(P<0.05)。3组患者治疗期间不良反应发生率比较,差异无统计学意义(P>0.05)。结论 与小剂量(10 mg/d)、中剂量(20 mg/d)阿托伐他汀相比,大剂量(40 mg/d)阿托伐他汀能更有效地改善冠心病心力衰竭患者心室重构、血脂代谢及心功能,且未增加药物相关不良反应发生风险。
冠心病;心力衰竭;阿托伐他汀;治疗结果;安全性
张淑平,刘宏颖,袁百祥,等.不同剂量阿托伐他汀治疗冠心病心力衰竭有效性及安全性的对比研究[J].实用心脑肺血管病杂志,2017,25(6):46-49.[www.syxnf.net]
ZHANG S P,LIU H Y,YUAN B X,et al.Comparative study for effectiveness and safety in treating coronary heart disease patients complicated with heart failure in different doses of atorvastatin[J].Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease,2017,25(6):46-49.
冠心病是心血管系统常见病、多发病,治疗不及时或病情进展可导致心力衰竭,且病死率较高。目前,临床治疗心力衰竭仍以维持心脏泵血功能、延缓心力衰竭进程、延长患者生存期为主要目的[1],常规抗心力衰竭治疗包括抗血小板聚集、强心、调脂等[2]。临床研究表明,阿托伐他汀作为调脂的代表药物对改善冠心病心力衰竭患者预后具有重要意义[3],但阿托伐他汀治疗心力衰竭的最佳负荷剂量尚存在争议。白墨青等[4]研究表明,大剂量阿托伐他汀能有效改善心力衰竭患者预后;但肖衍龙等[5]研究表明,小剂量阿托伐他汀治疗收缩性心力衰竭的疗效确切且安全性较高。本研究旨在比较不同剂量阿托伐他汀治疗冠心病心力衰竭的有效性及安全性,现报道如下。
1 资料与方法
1.1 纳入与排除标准 纳入标准:(1)近期无严重感染史;(2)未合并糖尿病、慢性阻塞性肺疾病、肺结核等;(3)无需服用其他药物。排除标准:(1)合并精神障碍者;(2)妊娠期和哺乳期妇女;(3)近期发生过休克、心肌梗死者;(4)合并肿瘤、病毒性感染及严重肝、肾、肺等重要脏器疾病者。
1.2 一般资料 选取2014年9月—2016年12月遵化市人民医院收治的冠心病心力衰竭患者165例,均符合第8版《内科学》[6]中的冠心病诊断标准及《中国心力衰竭诊断和治疗指南2014》[7]中的心力衰竭诊断标准。采用随机数字表法将所有患者分为A、B、C 3组,每组55例。3组患者性别、年龄、体质指数(BMI)、冠心病病程及纽约心脏病协会(NYHA)分级比较,差异均无统计学意义(P>0.05,见表1),具有可比性。本研究经医院医学伦理委员会审核批准,所有患者知情同意并签署知情同意书。
1.3 治疗方法 3组患者均给予常规治疗,包括休息、清淡饮食、适量运动、利尿、扩张血管及给予β-受体阻滞剂、血管紧张素转换酶抑制剂(ACEI)等药物治疗。在常规治疗基础上,A、B、C组患者分别给予小剂量阿托伐他汀(10 mg/次,1次/d)、中剂量阿托伐他汀(20 mg/次,1次/d)、大剂量阿托伐他汀(40 mg/次,1次/d),所用阿托伐他汀由Pfizer Ireland Pharmaceuticals生产;3组患者均连续治疗12周。

表1 3组患者一般资料比较
注:BMI=体质指数,NYHA=纽约心脏病协会;a为χ2值
1.4 观察指标 (1)比较3组患者治疗前后心室重构指标:采用飞利浦彩色超声多普勒诊断仪检测左心室舒张末期内径(LVEDD)、左心室收缩末期内径(LVESD),采用Simpson法检测左心室射血分数(LVEF)。(2)比较3组患者治疗前后血脂指标:采用氧化酶法检测三酰甘油(TG)、低密度脂蛋白胆固醇(LDL-C)、总胆固醇(TC),试剂盒购自上海申索佑福医学诊断用品有限公司。(3)比较3组患者治疗前后血浆氨基末端脑钠肽前体(NT-proBNP)和超敏C反应蛋白(hs-CRP)水平:抽取患者清晨空腹静脉血6 ml并置于真空采血管中,离心半径r=15 cm,3 000 r/min离心15 min,留取血浆,置于-20 ℃环境下保存待测,采用酶联免疫吸附试验(ELISA)检测血浆NT-proBNP和hs-CRP水平,试剂盒购自杭州普望生物技术有限公司,仪器为北京普朗新技术有限公司生产的DNM-9606酶标分析仪。(4)观察3组患者治疗期间不良反应发生情况。

2 结果
2.1 3组患者治疗前后心室重构指标比较 治疗前3组患者LVEDD、LVESD及LVEF比较,差异均无统计学意义(P>0.05);治疗后3组患者LVEDD、LVESD及LVEF比较,差异均有统计学意义(P<0.05)。治疗后B、C组患者LVEDD和LVESD小于A组,LVEF高于A组,差异有统计学意义(P<0.05);治疗后C组患者LVEDD和LVESD小于B组,LVEF高于B组,差异有统计学意义(P<0.05,见表2)。
2.2 3组患者治疗前后血脂指标比较 治疗前3组患者TG、TC、LDL-C比较,差异均无统计学意义(P>0.05);治疗后3组患者TG、TC、LDL-C比较,差异均有统计学意义(P<0.05)。治疗后B、C组患者TG、TC、LDL-C低于A组,C组患者TG、TC、LDL-C低于B组,差异均有统计学意义(P<0.05,见表3)。
2.3 3组患者治疗前后血浆NT-proBNP和hs-CRP水平比较 治疗前3组患者血浆NT-proBNP和hs-CRP水平比较,差异无统计学意义(P>0.05);治疗后3组患者血浆NT-proBNP和hs-CRP水平比较,差异有统计学意义(P<0.05)。治疗后B、C组患者血浆NT-proBNP和hs-CRP水平低于A组,C组患者血浆NT-proBNP和hs-CRP水平低于B组,差异均有统计学意义(P<0.05,见表4)。

Table 4 Comparison of plasma levels of NT-proBNP and hs-CRP among the three groups before and after treatment
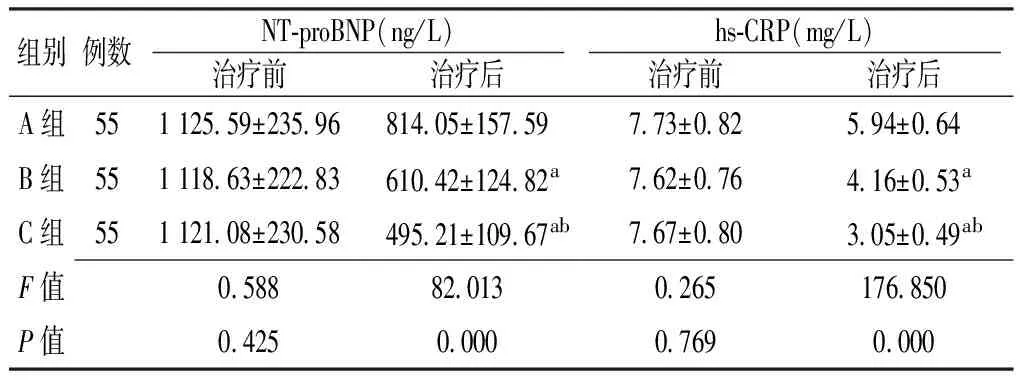
组别例数NT⁃proBNP(ng/L)hs⁃CRP(mg/L)治疗前治疗后治疗前治疗后A组551125 59±235 96814 05±157 597 73±0 825 94±0 64B组551118 63±222 83610 42±124 82a7 62±0 764 16±0 53aC组551121 08±230 58495 21±109 67ab7 67±0 803 05±0 49abF值0 58882 0130 265176 850P值0 4250 0000 7690 000
注:NT-proBNP=氨基末端脑钠肽前体,hs-CRP=超敏C反应蛋白;与A组比较,aP<0.05;与B组比较,bP<0.05
2.4 3组患者治疗期间不良反应发生率比较 治疗期间,A组患者不良反应发生率为3.6%,B组患者为5.4%,C组患者为10.9%。3组患者治疗期间不良反应发生率比较,差异无统计学意义(χ2=1.156,P=0.294,见表5)。

表5 3组患者治疗期间不良反应发生情况(例)

表2 3组患者治疗前后心室重构指标比较
注:LVEDD=左心室舒张末期内径,LVESD=左心室收缩末期内径,LVEF=左心室射血分数;与A组比较,aP<0.05;与B组比较,bP<0.05

表3 3组患者治疗前后血脂指标比较
注:TG=三酰甘油,TC=总胆固醇,LDL-C=低密度脂蛋白胆固醇;与A组比较,aP<0.05;与B组比较,bP<0.05
3 讨论
冠心病是指因冠状动脉狭窄、供血不足所致的心肌功能障碍和/或器质性病变[8]。临床研究表明,冠心病心力衰竭患者不仅表现为心脏射血功能下降,同时还伴有心室重构,故单纯强心治疗并不能有效改善患者预后[9-10]。近年来,随着对冠心病心力衰竭发生机制的研究深入发现,冠心病心力衰竭与神经内分泌紊乱关系密切,尤其是心脏交感神经系统紊乱[11]。VEVERKA等[12]研究结果显示,与单纯强心、利尿药物相比,抗心室重构药物能使大多数心力衰竭患者获益。
阿托伐他汀是临床常用的调脂药物,可通过调节血脂而降低心血管疾病风险[13]。近年有研究指出,阿托伐他汀除调脂作用外,还能抑制心室重构[14-15]。动物实验结果显示,阿托伐他汀可有效下调心肌血管紧张素Ⅱ受体水平,阻断氧自由基对心肌细胞的杀伤作用,从而抑制心肌肥厚[16],但阿托伐他汀治疗心力衰竭的最佳负荷剂量尚有争议。
本研究采用不同剂量阿托伐他汀治疗冠心病心力衰竭,结果显示,治疗后B、C组患者LVEDD和LVESD小于A组,LVEF高于A组;治疗后C组患者LVEDD和LVESD小于B组,LVEF高于B组;提示大剂量(40 mg/d)阿托伐他汀能有效改善患者心室重构。NT-proBNP是临床上评价心功能的常用客观指标,其水平升高提示心功能损伤[17];hs-CRP是一种由肝脏合成的与全身性炎症反应密切相关的非特异性标志物,是心血管事件预测因子之一。本研究结果显示,治疗后B、C组患者血浆NT-proBNP和hs-CRP水平低于A组,C组患者血浆NT-proBNP和hs-CRP水平低于B组,提示大剂量(40 mg/d)阿托伐他汀对冠心病心力衰竭患者心功能的改善效果更佳。增加阿托伐他汀剂量可能增加药物不良反应,故本研究进一步评价了不同剂量阿托伐他汀治疗冠心病心力衰竭的安全性,结果显示,3组患者治疗期间不良反应发生率间无差异,提示大剂量(40 mg/d)阿托伐他汀治疗冠心病心力衰竭的安全性较高。
综上所述,与小剂量(10 mg/d)、中剂量(20 mg/d)阿托伐他汀相比,大剂量(40 mg/d)阿托伐他汀能更有效地改善冠心病心力衰竭患者心室重构、血脂代谢及心功能,且未增加药物相关不良反应发生风险,值得临床推广应用。
[1]CARDINALE D,COLOMBO A,BACCHIANI G,et al.Response to letters regarding article,"Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy"[J].Circulation,2016,133(4):e363.DOI:10.1161/CIRCULATIONAHA.115.018780.
[2]FELKER G M,AHMAD T,ANSTROM K J,et al.Rationale and design of the GUIDE-IT study:Guiding evidence based therapy using biomarker intensified treatment in heart failure[J].JACC Heart Fail,2014,2(5):457-465.DOI:10.1016/j.jchf.2014.05.007.
[3]林晓明,陈生晓,钟春,等.不同剂量阿托伐他汀治疗冠心病慢性心力衰竭疗效分析[J].山东医药,2014,25(17):60-61.DOI:10.3969/j.issn.1002-266X.2014.17.024.
[4]白墨青,李宇琛.不同剂量阿托伐他汀治疗300例心力衰竭的临床效果分析[J].海峡药学,2016,28(4):203-204.DOI:10.3969/j.issn.1006-3765.2016.04.105.
[5]肖衍龙,颜程光.长期小剂量阿托伐他汀治疗血脂水平正常收缩性心力衰竭的分析[J].江西医药,2015,16(10):1047-1051.DOI:10.3969/j.issn.1006-2238.2015.10.033.
[6]葛均波,徐永健.内科学[M].8版.北京:人民卫生出版社,2013:473-474.
[7]中华医学会心血管病学分会,中华心血管杂志编辑委员会.中国心力衰竭诊断和治疗指南2014[J].中华心血管病杂志,2014,42(2):98-122.DOI:10.3760/cma.j.issn.0253-3758.2014.02.004.
[8]MYERBURG R J,JUNTTILA M J.Sudden cardiac death caused by coronary heart disease[J].Circulation,2012, 125(8):1043-1052.DOI:10.1161/CIRCULATIONAHA.111.023846.
[9]朱丽,巢敏,龙昱凤.阿托伐他汀对冠心病心力衰竭患者心功能的改善效果研究[J].当代医学,2015,21(16):143-144.DOI:10.3969/j.issn.1009-4393.2015.16.096.
[10]WELLES C C,KU I A,KWAN D M,et al.Left atrial function predicts heart failure hospitalization in subjects with preserved ejection fraction and coronary heart disease:Longitudinal data from the heart and soul study[J].J Am Coll Cardiol,2012,59(7):673-680.
[11]黄峻.心力衰竭合并冠心病处理的现代概念[J].中国介入心脏病学杂志,2014,9(3):201-204.
[12]VEVERKA A,JOLLY J L.Recent advances in the secondary prevention of coronary heart disease[J].Expert Rev Cardiovasc Ther,2014,2(6):877-889.
[13]蔡德印.阿托伐他汀对冠心病心力衰竭患者血浆脑钠肽水平的影响分析[J].中国实用医药,2014,32(26):161-162.
[14]林颖惠.阿托伐他汀治疗冠心病心力衰竭的效果观察[J].中国当代医药,2016,23(16):122-124.
[15]EL-SISI A,HEGAZY S,AHMED M,et al.Evaluation of short term effect of atorvastatin on myocardial performance and its pleiotropic effects on ischemic heart failure[J].Br J Pharm Res,2015,6(5):343-357.
[16]杜萍,常栋,陈畅.阿托伐他汀对大鼠心肌缺血再灌注保护作用的实验研究[J].中国医科大学学报,2014,43(5):407-410.
[17]崔飞飞,徐惠.阿托伐他汀对冠心病性心力衰竭患者血浆hs-CRP、NT-proBNP水平及心功能的影响[J].山东医药,2014,54(8):42-44.
(本文编辑:谢武英)
Comparative Study for Effectiveness and Safety in Treating Coronary Heart Disease Patients Complicated with Heart Failure in Different Doses of Atorvastatin
ZHANGShu-ping,LIUHong-ying,YUANBai-xiang,NAXue-feng,ZHANGXiao-zhang
ThePeople′sHospitalofZunhua,Zunhua064200,China
Objective To compare the effectiveness and safety in treating coronary heart disease patients complicated with heart failure in different doses of atorvastatin.Methods A total of 165 coronary heart disease patients complicated with heart failure were selected in the People′s Hospital of Zunhua from September 2014 to December 2016,and they were divided into A group,B group and C group according to random number table,each of 55 cases.Based on conventional treatment,patients of A group
low-dose atorvastatin(10 mg per time,1 time per day),patients of B group received medium-dose atorvastatin(20 mg per time,1 time per day),while patients of C group received high-dose atorvastatin(40 mg per time,1 time per day);all of the three groups continuously treated for 12 weeks.Index of ventricular remodeling,blood lipids index,plasma levels of NT-proBNP and hs-CRP before and after treatment were compared among the three groups,and incidence of adverse reactions was observed during the treatment.Results No statistically significant differences of LVEDD,LVESD or LVEF was found among the three groups before treatment(P>0.05);after treatment,LVEDD and LVESD of B group and C group were statistically significantly smaller than those of A group,while LVEF of B group and C group was statistically significantly higher than that of A group,respectively(P<0.05);after treatment,LVEDD and LVESD of C group was statistically significantly smaller than that of B group,respectively,while LVEF of C group was statistically significantly higher than that of B group(P<0.05).No statistically significant differences of TG,TC or LDL-C was found among the three groups before treatment(P>0.05);after treatment,TG,TC and LDL-C of B group and C group were statistically significantly lower than those of A group,meanwhile TG,TC and LDL-C of C group were statistically significantly lower than those of B group(P<0.05).No statistically significant differences of plasma level of NT-proBNP or hs-CRP was found among the three groups before treatment(P>0.05);after treatment,plasma levels of NT-proBNP and hs-CRP of B group and C group were statistically significantly lower than those of A group,meanwhile plasma levels of NT-proBNP and hs-CRP of C group were statistically significantly lower than those of B group(P<0.05).No statistically significant differences of incidence of adverse reactions was found among the three groups during the treatment(P>0.05).Conclusion Compared with low-dose atorvastatin(10 mg per day)and medium-dose atorvastatin(20 mg per day),high-dose atorvastatin(40 mg per day)can more effectively inhibit the ventricular remodeling,adjust the blood lipid metabolism and improve the cardiac function,without increasing the risk of adverse reactions.
Coronary disease;Heart failure;Atorvastatin;Treatment outcome;Safe
河北省科技成果推广课题(20171401)
R 541.4 R 541.6
B
10.3969/j.issn.1008-5971.2017.06.011
2017-02-15;
2017-06-12)
064200河北省遵化市人民医院