尺骨近端旋转截骨术治疗先天性桡骨头前脱位11例报告
苗武胜 汪兵 吴革 吴永涛 姜海 屈继宁 李敏 王晓威 梁小菊
尺骨近端旋转截骨术治疗先天性桡骨头前脱位11例报告
苗武胜 汪兵 吴革 吴永涛 姜海 屈继宁 李敏 王晓威 梁小菊
目的 评估自行设计的尺骨近端旋转截骨技术治疗先天性桡骨头前脱位的疗效。方法 选取2 0 0 8 年 4 月至 2 0 1 5 年 1 2 月我院收治的无明确外伤史的桡骨头前脱位患儿 1 1 例,首例术前诊断为陈旧性孟氏骨折,术中发现其桡骨头前脱位,上尺桡关节位置异常,按陈旧性孟氏骨折的处理办法桡骨头不能复位,将尺骨上段截骨,远端向外后侧旋转,桡骨头可获得复位。基于这种发现,对其余 1 0 例无明确外伤史的先天性桡骨头前脱位患儿术前常规行 M R I 检查,其主要的病理改变为上尺桡关节位置异常,位于前外侧而不是外侧,由此应用自行设计的尺骨近端旋转截骨术,将上尺桡复合体向后外侧旋转,从而使肱桡关节复位。采用尺骨近端旋转截骨术共治疗 1 1 例先天性桡骨头前脱位患儿,其中男 7 例,女 4 例,年龄 2~1 2 岁,平均6.1 岁。对术前和术后的影像学和临床功能进行评估,回顾性分析术后疗效。结果 本组 1 1 例均获 1 2 ~7 0 个月随访,平均 2 6 个月。肘关节的 X 线片提示肱桡关节均复位,无桡骨头脱位的复发,无截骨处不愈合、尺骨近端发育无异常。无伤口感染、神经损伤。提携角明显减小 ( P<0.0 5 ),肘关节的稳定性和屈曲幅度得到明显改善 ( P<0.0 5 )。结论 尺骨近端旋转截骨术治疗先天性桡骨头前脱位有效,临床疗效满意。
桡骨;脱位;先天性桡骨脱位;尺骨旋转截骨;复位
先天性桡骨头脱位是一种较少见的疾病,但属于肘关节最常见的先天性畸形[1]。可以单独出现,也可以同时合并先天性上尺桡骨连接或合并其它部位的畸形[2-3]。早期多无临床症状,偶可因为肘关节前方包块、肘关节活动受限或者外伤后拍 X 线片发现,青少年时期少数可表现为轻微疼痛、弹响或肘关节屈曲活动受限。持续性的脱位可能会引起肘关节的不稳定、进行性肘外翻畸形和桡骨头的异常发育,最终将会导致肘关节的骨性关节炎[4]。因此,复位脱位的桡骨头恢复肘关节的解剖学关系是必要的。治疗先天性桡骨头脱位的手术方法有很多,包括切开复位尺骨截骨术;切开复位尺骨截骨、环状韧带重建术;桡骨头切除术等[5-7]。然而,由于对先天性桡骨头脱位的病理改变没有统一的认识,这些技术均未被广泛接受。
本组首例病例术前诊断为陈旧性孟氏骨折患儿,术中发现有完整的环状韧带,肱桡关节间无瘢痕组织,但尺骨桡切迹位于前外侧,桡骨头前脱位,按陈旧性孟氏的处理方法尺骨上段截骨成角后桡骨头不能复位,将截骨远端向外后侧旋转,桡骨头可获得复位。基于此发现,本组病例术前常规行M R I 或 C T 检查,发现这些病例中肘关节内无瘢痕组织,上尺桡关节可有完整的关节,但上尺桡关节位于尺骨的前外侧 ( 图 1 ),这些病理改变不同于陈旧性孟氏骨折。基于这一重要的发现设计了尺骨近端旋转截骨术。通过尺骨近端截骨,将上尺桡复合体向后外侧旋转,使上尺桡关节位于尺骨外侧,从而使脱位肱桡关节复位。笔者以尺骨近端旋转截骨的方法治疗先天性桡骨头脱位 1 1 例,现报告如下。
资料与方法
一、纳入与排除标准
1. 纳入标准:( 1 ) 2 0 0 8 年 4 月至 2 0 1 5 年1 2 月,我院收治的先天性桡骨头前脱位的患儿;( 2 )无明确外伤史;( 3 ) X 线片示桡骨头前脱位;( 4 ) 术前 M R I 示肘关节内无瘢痕组织;( 5 ) 上尺桡关节有完整的关节,但上尺桡关节位于尺骨的前外侧。
2. 排除标准:( 1 ) 术前 M R I 示肘关节内有瘢痕组织;( 2 ) 上尺桡关节脱位,上尺桡关节位于尺骨的外侧;( 3 ) 陈旧性孟氏骨折。
二、一般资料
本组共纳入 1 1 例,其中男 7 例,女 4 例,年龄2~1 2 岁,平均 6.1 岁。单侧 1 0 例、双侧 1 例。就诊的主要原因是偶然发现肘部异常包块、轻微外伤或肘关节外翻畸形,诊断桡骨头脱位 ( 表 1 )。
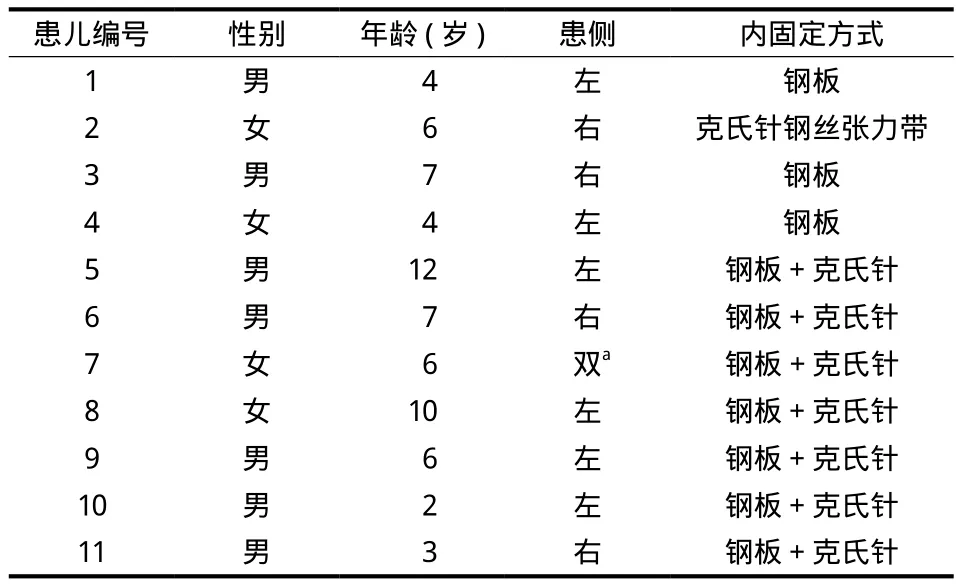
表1 患儿基本资料Tab.1 The basic information of the children
本组 1 1 例中,首例是以“陈旧性孟氏骨折”收入住院,术中发现桡骨头向前脱位,上尺桡有完整的关节,但位于前外侧,术中按陈旧性孟氏骨折的截骨方法在尺骨上段截骨钢板内固定,肱桡关节不能复位,但在将尺骨截骨远端向后外侧旋转时桡骨头可获得复位。由此对没有明确外伤史的桡骨头前脱位的患儿常规行 M R I 检查并与正常儿童肘关节M R I 比较。在正常儿童及陈旧性孟氏骨折患儿中尺骨桡切迹位于尺骨近端的外侧,陈旧性孟氏骨折中肱桡间有瘢痕组织,先天性桡骨头脱位患儿 M R I 显示尺骨桡切迹位于尺骨近端的前外侧,关节面也比较表浅,桡骨头发育差,不同于正常儿童和陈旧性孟氏骨折患儿 ( 图 1 )。其余 1 0 例为先天性桡骨头前脱位。术前通过双侧尺桡骨全段 X 线片评估尺骨的长度及桡骨是否过长,对桡骨头高于尺骨冠状突0.5 c m 或桡骨过长超过 0.5 c m 的患儿需前期行尺骨延长术,使桡骨头下降位于尺骨冠状突水平。1 1 例患儿肘关节 X 线片共同点是正位片上尺桡骨近端交叉和重叠,侧位 X 线片提示桡骨头向前脱位,尺骨弓形征不明显。
所有患儿均行尺骨近端旋转截骨手术。收集术前和术后患儿肘关节正侧位 X 线片,肘关节的活动范围,以及肘关节的 M E P S 功能评分,对手术效果进行评估。同时观察患儿是否出现截骨处不愈合、感染、神经损伤、尺骨近端发育异常、术后再脱位等术后并发症。所有数据使用 S P S S 1 9.0 软件进行统计分析,肘关节术前术后活动度使用配对样本 t 检验,对肘关节术前术后活动度进行正态性检验,符合正态分布的比较采用 t 检验,P<0.0 5 认为差异有统计学意义。
二、手术方法
手术采用 B o y d 肘关节后外侧入路,暴露肘关节后,首先观察肱桡、肱尺、尺桡关节是否在一个关节腔内,并观察它们的关系是否正常,探查环状韧带的完整性,确定尺骨的截骨平面,尺骨的截骨平面位于尺骨冠状突水平,与桡骨头关节面平行,尺骨截骨后,将上尺桡关节 ( 复合体 ) 作为一个整体向后外侧进行旋转,旋转的程度视桡骨头是否和肱骨小头恢复良好的对合关系而定。桡骨头复位后,使用克氏针和 ( 或 ) 钢板对截骨部位进行固定,屈伸肘关节及旋转前臂观察肱桡关节的稳定性。术中即行透视定位确保钢板及螺钉不会损伤骨骺,确定桡骨头是否复位。术后肘关节屈曲 9 0°、前臂旋后位上肢石膏托固定 3~4 周后开始肘关节功能锻炼。外科手术见图 2。
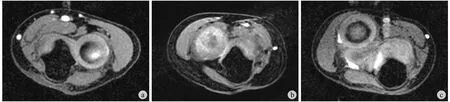
图1 a:正常肘关节,上尺桡关节面位于尺骨外侧;b:先天性桡骨头前脱位,上尺桡骨关节面位于尺骨前外侧;c:陈旧性孟氏骨折中尺骨桡切迹位于外侧,而且上尺桡是脱位Fig.1 a: Proximal radioulnar joint was located in the lateral side of the ulna in the normal elbow joint; b: Proximal radioulnar joint was located in the anterior lateral side of the ulna in the patient with congenital anterior dislocation of the radial head; c: Radial notch was located in the lateral side of the ulna, and the proximal radioulnar joint dislocation was noticed in the patient with old Monteggia fracture

图2 a:先天性桡骨头前脱位术中所见:肱桡关节脱位,关节内无瘢痕组织,上尺桡有完整的关节,但位于尺骨近端前外侧;b:在平行桡骨头水平行尺骨截骨;c:上尺桡复合体向外后侧旋转恢复肱桡关系,用截骨板固定截骨远近端Fig.2 a: During the operation for congenital anterior dislocation of the radial head, the radiocapitellar joint dislocation was noticed. There were no scar tissues in the joint. There was a complete joint in the proximal radioulnar joint, but it was located in the anterior lateral side of the ulna; b: Ulna osteotomy was performed at the level of parallel radial head; c: Upper radioulnar complex was rotated posterolaterally to restore the radiocapitellar line and the osteotomy site was fi xed with the plate
结 果
所有患儿均获 1 2~7 0 个月随访,平均 2 6 个月。肘关节的 X 线片提示肱桡关节均复位,无桡骨头脱位的复发,无截骨处不愈合、尺骨近端发育无异常。无伤口感染,神经损伤。提携角明显减小,肘关节的稳定性和屈曲幅度得到改善。
一、放射学评估
术前正位 X 线片主要表现为肘外翻,尺桡骨近端重叠,侧位 X 线片上桡骨头向前脱位。术后肘关节正侧位片提示:术后所有患儿提携角较术前减小,尺桡骨近端交叉和重叠的影像消失,桡骨头完全复位,尺骨无过度后成角 ( 图 3 )。患儿术后均未出现桡骨头脱位复发、骨化性肌炎、上尺桡骨性融合、截骨部位不愈合等并发症。
二、临床评估
术前 9 例屈曲活动受限,术后 7 例肘关节的屈伸活动度得到改善,1 例无明显变化,1 例伸直活动受限。所有 1 1 例术前前臂旋转正常,第 1 例截骨平面在上尺桡关节面下方,术后旋后活动严重受限,其余 1 0 例旋后正常,但 1 例旋前受限 1 0°,2 例旋前受限 5° ( 表 2 )。使用配对样本 t 检验经统计分析,发现 1 1 例术后屈伸活动均较前有所增加,其活动度增加差异有统计学意义 ( t=-5.9 7,P=0.0 0 ) ( 表 3 );术后旋前旋后活动较术前无明显变化,其活动度变化差异无统计学意义 ( t=2.0 2 5,P=0.0 7 ) ( 表 3 );术后提携角较术前均有改善,其改善度差异有统计学意义 ( t=1 0.2 5,P=0.0 0 ) ( 表 3 )。肘关节的疼痛和日常活动术前术后未见明显变化。
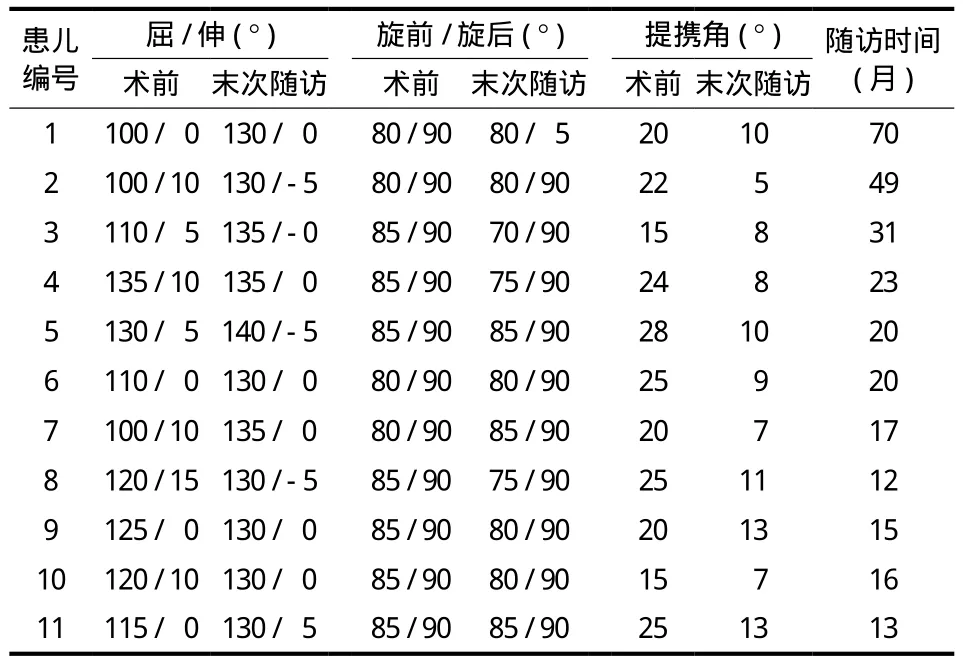
表2 先天性桡骨头前脱位术前、术后肘关节功能及提携角对比Tab.2 Comparison of preoperative and postoperative elbow functions and carrying angles in the patients with congenital anterior dislocation of the radial head
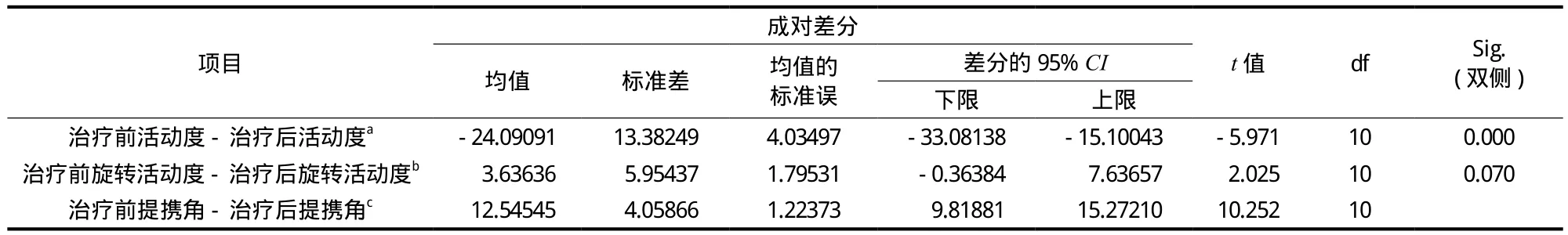
表3 对手术前后屈伸活动度、提携角配对样本 t 检验Tab.3 Paired sample t-test of preoperative and postoperative rotation ranges of fl exion and extension

图3 a:患儿,男,7 岁,右肘关节正位 X 线片示尺桡骨近端交叉和重叠;b:肘关节侧位 X 线片示桡骨头前脱位;c~d:术后 2 个月X 线片示桡骨头复位、提携角减小;e~f:术后 2 年 X 线片示尺骨近端发育正常Fig.3 a: Anteroposterior radiograph of the right elbow of a 7-year-old boy showed overlap between the proximal radius and ulna; b: Lateral radiograph of the elbow showed anterior dislocation of the radial head; c - d: X-ray 2 months after operation showed the reduction of the radial head and decrease of the carrying angle; e - f: X-ray 2 years after operation showed the development of the proximal ulna was normal
讨 论
先天桡骨头脱位发病原因目前尚不清楚,有学者认为与胚胎发育的五个阶段有关[8]。其影像学表现主要为相对短的尺桡或者长的桡骨;肱骨小头发育不全或者缺如;部分滑车缺如;长而细的桡骨颈、桡骨头圆顶状;突出的肱骨内髁;尺骨弓形症[9],患儿年龄越大畸形越明显。先天性桡骨头脱位患儿早期多无症状,青春期前有轻微疼痛以及肘关节屈伸活动受限[10-11]。随着年龄的增长,疼痛和肘关节功能障碍将会逐步加重[3,10-15]。桡骨头切除术虽为经典技术,但切除桡骨头后可引起其它并发症[16]。采用尺骨截骨、切开复位并环状韧带重建来达到桡骨头复位。有较高的并发症和术后再次脱位的现象[5]。为使桡骨头复位,这些技术中尺骨截骨往往需要向后过度成角,容易出现伸直肘关节受限。而本研究中尺骨不需要向后成角,对肘关节伸直活动影响小。
近几年,有研究通过三维 C T 扫描与重建发现陈旧性桡骨头脱位的患儿,尺骨存在三维畸形,有学者根据所测三维畸形制订手术方案,通过尺骨旋转截骨治疗桡骨头脱位获得成功[17-18]。本组病例尺骨同样存在旋转畸形;尺骨桡切迹向前外移位,桡骨头位于肱骨小头前方,为行尺骨旋转截骨术提供了理论基础。因此,本研究试图通过改变上尺桡关节的位置,而使桡骨头复位。
确定尺骨截骨平面对于该手术的成功至关重要。第 1 例患儿术后出现旋转严重受限。可能与该患儿尺骨截骨平面没有位于桡骨头平面,而是在上尺桡关节面下方有关。在尺骨截骨后的旋转过程中,实际是近端尺桡关节整体向外侧旋转,使得桡骨头达到复位,因此,该手术不适合桡骨过长的患儿。对桡骨头过长的患儿,需在前期行尺骨延长术。截骨过程中,应特别注意保护桡骨头圆韧带受到损伤。环状韧带在维持肘关节的稳定性中发挥重要作用。
截骨平面在尺骨冠状突水平,毗邻近端尺桡关节和肱桡关节,因此,该类手术是否会引起尺骨近端发育异常和肘关节骨性关节炎是关注的一个焦点。在短期随访中,尚未发现尺骨近端发育异常及骨性关节炎的发生。
本研究未对先天性桡骨头后脱位及侧方脱位的病理改变进行研究,尺骨近端旋转截骨只是针对先天性桡骨头前脱位的病理改变而设计,是否适用于后脱位及侧方脱位需要进一步研究。同时,对于桡骨脱位高的病例,需前期尺骨延长,否则容易发生再脱位。
综上所述,短期的随访结果提示尺骨近端旋转截骨是一种治疗先天性桡骨头脱位的有效方法。但本研究样本量小、随访期很短,存在术前及术后病理变化待证实的不足;尺骨近端旋转截骨是否适用其它类型的脱位,也有待临床验证。
[1]Caravias DE. Some observations on congenital dislocation of the head of the radius[J]. J Bone Joint Surg Br, 1957, 39-B(1):86-90.
[2]Agnew DK, Davis RJ. Congenital unilateral dislocation of the radial head[J]. J Pediatr Orthop, 1993, 13(4):526-528.
[3]Miura T. Congenital dislocation of the radial head[J]. J Hand Surg Br, 1990, 15(4):477-481.
[4]Lloyd-Roberts GC, Bucknill TM. Anterior dislocation of the radial head in children: aetiology, natural history and management[J]. J Bone Joint Surg Br, 1977, 59-B(4):402-407.
[5]Hasler CC, Von Laer L, Hell AK. Open reduction, ulnar osteotomy and external fi xation for chronic anterior dislocation of the head of the radius[J]. J Bone Joint Surg Br, 2005, 87(1):88-94.
[6]Campbell CC, Waters PM, Emans JB. Excision of the radial head for congenital dislocation[J]. J Bone Joint Surg Am, 1992, 74(5):726-733.
[7]Yamazaki H, Kato H. Open reduction of the radial head with ulnar osteotomy and annular ligament reconstruction for bilateral congenital radial head dislocation: a case with longterm follow-up[J]. J Hand Surg Eur Vol, 2007, 32(1):93-97.
[8]Al-Qattan MM, Abou Al-Shaar H, Alkattan WM. The pathogenesis of congenital radial head dislocation/subluxation[J]. Gene, 2016, 586(1):69-76.
[9]Bryan McFarland. Congenital dislocation of the head of the radius[J]. Br J Surg, 1936, 24:41-49.
[10]Bengard MJ, Calfee RP, Steffen JA, et al. Intermediate-term to long-term outcome of surgically and nonsurgically treated congenital, isolated radial head dislocation[J]. J Hand Surg Am, 2012, 37(12):2495-2501.
[11]Kaas L, Struijs PA. Congenital radial head dislocation with a progressive cubitus valgus: a case report[J]. Strategies Trauma Limb Reconstr, 2012, 7(1):39-44.
[12]Bell SN, Morrey BF, Bianco AJ Jr. Chronic posterior subluxation and dislocation of the radial head[J]. J Bone Joint Surg Am, 1991, 73(3):392-396.
[13]Kelly DW. Congenital dislocation of the radial head: spectrum and natural history[J]. J Pediatr Orthop, 1981, 1(3):295-298.
[14]Sachar K, Mih AD. Congenital radial head dislocations[J]. Hand Clin, 1998, 14(1):39-47.
[15]Song KS, Ramnani K, Cho CH. Long term follow-up of open realignment procedure for congenital dislocation of the radial head[J]. J Hand Surg Eur Vol, 2011, 36(2):161-162.
[16]Bengard MJ, Calfee RP, Steffen JA, et al. Intermediate-term to long-term outcome of surgically and nonsurgically treated congenital, isolated radial head dislocation[J]. J Hand Surg Am, 2012, 37(12):2495-2501.
[17]Miyake J, Oka K, Moritomo H, et al. Open reduction and 3-dimensional ulnar osteotomy for chronic radial head dislocation using a computer-generated template: case report[J]. J Hand Surg Am, 2012, 37(3):517-522.
[18]Miyake T, Iida G, Fukuhara T, et al. Treatment of plastic bowing of the ulna with radial head dislocation using minimally invasive bending and rotational osteotomy: a case report[J]. J Shoulder Elbow Surg, 2013, 22(6):e20-24.
A retrospective analysis of the curative results of proximal ulnar rotation osteotomy for congenital anterior dislocation of the radial head in children
MIAO Wu-sheng, WANG Bing, WU Ge, WU Yong-tao, JIANG Hai, QU
Ji-ning, LI Min, WANG Xiao-wei, LIANG Xiao-ju. Department of Pediatric Orthopedics, Honghui Hospital, Xi’an Jiaotong University, Xi’an, Shaanxi, 710054, China
WANG Bing, Email: wangbingheli@126.com
Objective To evaluate the curative results of self-designed proximal ulnar rotation osteotomy for the treatment of congenital anterior dislocation of the radial head. Methods From April 2008 to December 2015, 19 children with anterior dislocation of the radial head without a history of trauma were treated in our hospital. Firstly, one child was radiographically diagnosed with old Monteggia fracture before surgery with abnormal position of proximal radioulnar joint, which could not be treated by using old Monteggia procedures. We repositioned the radial head by cutting the proximal ulna and rotated the distal ulna back-outside. The MRI examination was performed in 18 cases of anterior dislocation of the radial head without a history of trauma before surgery. It showed that there were 8 cases of old Monteggia fractures and 10 cases of congenital anterior dislocation of the radial head. The main pathological changes included abnormal position of the proximal radioulnar joint, which was located in the anterior lateral side of the ulna rather than the outside. Based on the pathological changes, we designed proximal ulnar rotation osteotomy with ulnar radial complex on the backward of the lateral rotation to reset the radiocapitellar joint. Among the 11 patients treated with proximal ulnar rotation osteotomy, there were 7 boys and 4 girls whose average age was 6.1 years ( range: 2 - 12 years ). The curative results were retrospectively analyzed for 11 children with congenital anterior dislocation of the radial head by preoperative and postoperative radiographical and clinical evaluation of the elbow functions. Results All the patients were followed up for an average period of 26 months ( range: 12 - 70 months ). The radiography of the elbow showed that the radiocapitellar joint was reduced in all the patients, and radial head dislocation did not recur. No ulnar nonunion, elbow osteoarthritis, wound infection or nerve injury was observed in these patients. The carrying angle was obviously decreased ( P < 0.05 ). The elbow stability and range of elbow fl exionmotion were obviously improved ( P < 0.05 ). Conclusions The follow-up results have shown that proximal ulnar rotation osteotomy is an effective method for the treatment of congenital anterior dislocation of the radial head.
Radius; Dislocations; Congenital dislocation of the radial head; Ulnar rotation osteotomy; Reset
10.3969/j.issn.2095-252X.2017.07.007
R726.8, R682.1
2017-03-27 )
( 本文编辑:李慧文 )
7 1 0 0 5 4 西安交通大学附属红会医院小儿骨科
汪兵,E m a i l: w a n g b i n g h e l i@1 2 6.c o m