锁骨骨折患者并发症的原因分析与对策
张晓萌 陈建海 王艳华 寇玉辉 付中国 张殿英
·论著·
锁骨骨折患者并发症的原因分析与对策
张晓萌 陈建海 王艳华 寇玉辉 付中国 张殿英
目的探讨锁骨骨折患者并发症的原因及相应对策。方法选自1999年1月至2016年9月北京大学人民医院创伤骨科收治的锁骨骨折患者465例,对所有病例进行检索,并收集并发症患者的相关病历资料,分析其发生原因并据此采取相应对策。结果本组共有17例患者出现并发症,占全部锁骨骨折住院患者总数的3.87%;住院时间为3~36d,平均(12.35±10.39)d。所有患者初次致伤后按照Craig分型分类,其中Ⅰ型骨折13例、Ⅱ型骨折3例,Ⅲ型骨折1例。本组患者并发症出现时间大多在20d至1年内,仅有1例医源性骨折患者发生于术后26年。5例患者有内科合并症,其中超过3项术后合并症的患者有3例。9例患者出现骨折不愈合,其中包括4例钢板断裂、2例内固定松动和3例出现骨折不愈合;3例患者出现内固定取出后原位置再骨折;2例出现伤口愈合不良;1例出现内固定外露;1例患者内固定术后同侧锁骨因外伤出现新发骨折。再次手术的16例患者中,有7例患者行自体髂骨植骨术。除外1例保守治疗导致锁骨严重畸形愈合患者因手术禁忌而继续采取保守治疗措施,其他16例患者均再次行手术治疗并痊愈出院。结论本组锁骨骨折病例的并发症多与内固定手术有关,针对已发生并发症的锁骨骨折患者应制定个性化的治疗方案,但大多需通过再次手术实现;严密的术前评估与手术计划,规范的术中操作以及合理的功能锻炼是预防并发症发生的主要措施。
锁骨骨折;并发症;保守治疗;手术治疗
锁骨骨折是最常见的骨折之一,其发生率在成人中占全身骨折的2.6%~4.0%[1-3]。传统观点认为,大多数锁骨骨折通过保守治疗可获得良好功能,但Zlowodzki等[4]的一项Meta分析表明,非手术治疗锁骨骨折的不愈合发生率大约为5.9%。目前针对移位显著(移位、短缩大于2cm)、粉碎严重(骨块大于3块、多段骨折)的锁骨骨折患者,大多推荐手术治疗以降低并发症发生率[5],但仍存在一定的风险。Ricci等[6]报道了锁骨中段骨折切开复位内固定术后再手术原因有骨折不愈合、深部感染和畸形愈合,其发生率远低于保守治疗。目前针对锁骨骨折并发症尚缺乏规范的治疗。本研究回顾性分析了北京大学人民医院创伤骨科自1999年1月至2016年9月共收治的465例锁骨骨折患者,发现有17例出现并发症,本文总结了这些并发症的发生原因及相应对策,取得了满意的临床疗效,现报道如下。
资料与方法
一、一般资料
自1999年1月至2016年9月,本院共收治锁骨骨折患者465例,其中有17例患者发生并发症,列入本组研究对象。本研究采用回顾性分析方法,研究指标包括患者的性别、年龄、左右侧、致伤原因、并发症发生时间、主要合并症、治疗措施、住院时间以及出院时情况等(表1)。
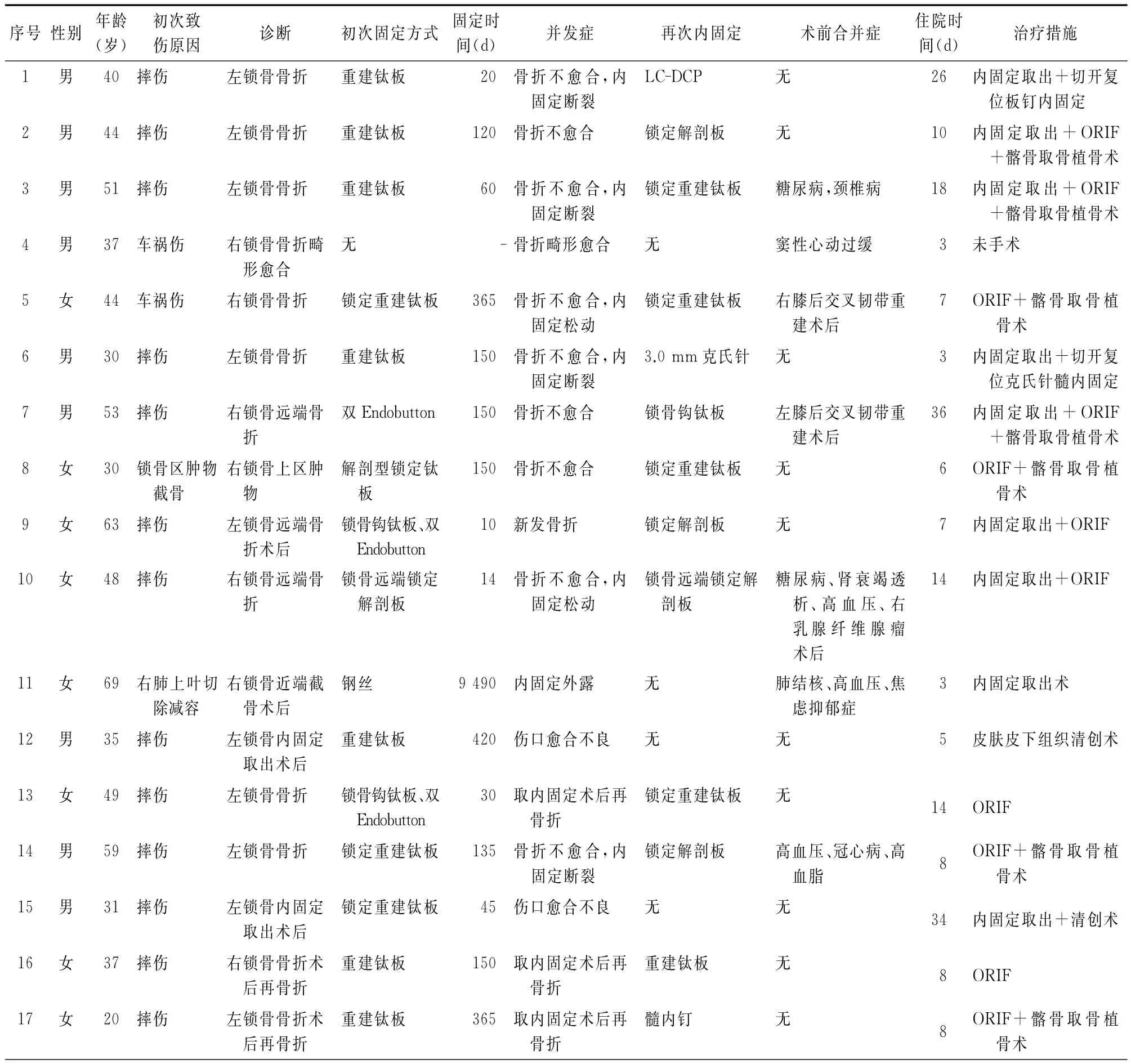
表1 17例出现并发症患者的相关资料
本组17例患者,男9例,女8例;年龄20~69岁,平均年龄为(43.53±13.01)岁;左侧10例,右侧7例。初次致伤原因均为外伤,其中摔伤13例,车祸致伤2例,医源性锁骨骨折2例。伤后16例患者接受手术治疗,1例患者因手术禁忌行保守治疗。另外,11例患者发生于日常活动中,无明显外伤诱因,1例患者发生再次摔伤,1例患者发生于患侧肢体过度负重时,2例患者因可疑感染导致伤口愈合不良,1例因内固定物长期与皮肤及皮下组织摩擦导致外露。
二、治疗措施
17例患者中有16例再次行手术治疗。治疗措施:3例患者行内固定取出、再次切开复位内固定、植骨手术;4例患者行内固定取出、再次切开复位内固定未植骨;4例患者行切开复位内固定、髂骨取骨植骨术;2例患者仅行切开复位内固定术;1例患者取出内固定后行皮肤软组织清创术;1例患者仅行内固定取出术;1例患者仅行皮肤软组织清创术;1例患者因禁忌证采取非手术治疗。
三、术后处理
所有手术患者术后均采用前臂吊带固定患肩2周左右,2周后逐渐恢复肩关节的主、被动活动,6~8周后行持重功能训练。1例保守治疗的患者因锁骨已畸形愈合,不再对患侧肩关节主、被动活动进行限制,仅要求避免患侧上肢过度持重。
四、统计学分析
所有数据采用Excel 2016软件整理,并采用SPSS 20.0软件对部分数据进行分析处理,计量资料用±s表示。
结 果
本组研究共有17例患者,占全部锁骨骨折住院患者总数的3.66%;住院时间为3~36d,平均(12.35±10.39)d。所有患者初次致伤后按照Craig分型分类,其中Ⅰ型骨折13例、Ⅱ型骨折3例,Ⅲ型骨折1例。本组患者并发症出现时间大多在20d至1年内,仅有1例医源性骨折患者发生于术后26年。5例患者有内科合并症,其中超过3项合并症的患者有3例。9例患者出现骨折不愈合,其中包括4例(1、3、6和14号)钢板断裂(图1)、2例(5和10号)内固定松动(图2)、3例(2、7和8号)仅出现骨折不愈合;3例(13、16和17号)患者出现内固定取出后原位置再骨折;2例(12和15号)出现伤口愈合不良;1例(11号)出现内固定外露;1例(9号)患者内固定术后同侧锁骨因外伤出现新发骨折;另有1例患者(4号)伤后因手术禁忌采取保守治疗导致畸形愈合(图3)。再次手术的16例患者中,有7例患者行自体髂骨取骨植骨术。
讨 论

图1 14号患者,59岁,男性,左侧锁骨中段骨折切开复位内固定术后正位X线片(A),提示内固定位置良好,达到解剖复位。术后3个月左右正位X线片(B)提示左侧锁骨内固定断裂,骨折不愈合,轻度成角移位。术中(C)取出断裂的内固定后清除断端死骨,再次复位后放置锁骨解剖型锁定钛板,断端植入自体髂骨。术后正位X线片(D)显示内固定位置良好,骨折断端愈合。术后2年正位X线片(E、F)显示骨折已愈合以及内固定取出术后表现

图2 5号患者,44岁,女性,X线片(A)示右锁骨中段骨折,断端移位。手术采用切开复位非锁定解剖钛板内固定。术后正位X线片(B)提示骨折不愈合,螺钉松动,内固定失效。术中(C、D)取出内固定后放置锁定型解剖钛板并取自体髂骨植入骨折断端。术中(E)及术后X线片(F)显示内固定位置良好,骨折解剖复位

图3 4号患者,37岁,男性,右锁骨骨折后保守治疗10个月,因手术禁忌继续采取保守治疗。X线片分别显示伤后10个月(A)、伤后15个月(B)和伤后18个月(C)的锁骨愈合情况
锁骨骨折可发生于各年龄段,通常好发于小于3 0岁的青年男性和大于80岁的老年人这两个高峰段[1]。早期观点认为,锁骨中段骨折即使有移位(断端有2/3接触)也可通过保守治疗(“8”字绷带或前臂吊带)获得收益。Lenza等[7]研究发现有移位骨折的通过保守治疗其不愈合发生率可高达15%。同时,Andermahr等[8]和 Edelson[9]认为保守治疗的锁骨骨折均有不同程度的畸形愈合,而锁骨畸形愈合不仅影响患者美观,也可引起肩关节功能障碍。Ledger等[10]通过CT三维重建、调查问卷及生物力学检测研究发现锁骨骨折短缩移位15mm时对肩关节活动的影响较大。McKee等[11]研究发现锁骨畸形可严重影响相应上肢的肌力。因此对于存在临床症状的骨折不愈合或畸形愈合患者应积极采取手术矫正,以改善肩胛带及相应肢体的功能。在本院465例锁骨骨折住院患者中,有1例37岁中年男性患者(4号)因车祸导致右锁骨中段骨折,采取保守治疗约2个月后出现右侧锁骨严重畸形愈合的并发症。但由于合并有窦性心动过缓,最终只能放弃手术矫形并接受后续功能康复锻炼。
随着内固定材料的发展和技术的成熟,现代观点认为锁骨骨折只要存在手术指征都应积极采取手术治疗,其优势在于能够达到解剖复位、减少疼痛[1215],避免了骨折断端的扭转,而且手术简单可靠还可重复[16],降低了畸形愈合的发生率[17],有助于患者早期功能锻炼,恢复正常工作和生活,并获得更好的美观和整体满意度。然而手术治疗也有一定几率导致并发症的发生,原因较为复杂,应该获得足够重视。这些并发症通常包括内固定松动(4.8%)[1820]、钢 板 断 裂 (1.9%)[18]、感 染 (0% ~18%)[1921]、内 固 定 引 起 的 疼 痛、术 后 再 发 骨 折(0.04%)[22]等,通常与骨折粉碎严重、术中操作不当、内固定取出时间过早、术后患者依从性差、不能遵循制动及限制负重等危险因素有关[22-25]。章浩等[26]研究认为,医源性因素是锁骨骨折内固定失败的最主要原因。术中复位手法粗暴、过度强调解剖复位以及过多剥离骨膜,均可干扰骨折断端血运;同时,为达到满意的复位而采用缝线或钢丝捆扎过紧也可减少骨折断端的血供,影响骨折愈合。因此,在骨折端的显露与复位时应尽量避免对周围组织及骨膜的过度干扰,减少术后骨折不愈合的发生。术中采用重建板并可因金属疲劳而降低钢板强度,易导致内固定物断裂;而内固定物工作距离过短则使钢板受力增大,无法抗拒锁骨在肩胛带活动时产生的扭转力量,同时钢板未放置于锁骨张力侧以及固定螺钉数量不足均可导致日后发生内固定松动。针对此类并发症大多主张取出原有内固定后清除死骨,对骨折断端进行新鲜化处理,复位后尽量选用锁定钛板内固定治疗以减少反复塑形对钛板强度的影响,同时进行断端植骨可促进骨折断端生长。与人工骨材料相比,自体髂骨具有其他人工骨材料所不具备的良好的骨形成、骨传导和骨诱导作用,降低了感染风险,是最理想的材料[27]。此外,术后应延长患侧肩关节的制动时间以及避免患肢过早负重活动。
本组17例患者的并发症主要与内固定物及手术伤口相关。1、3、6、14号患者出现内固定断裂,主要与内固定物选择不当有关。这4例患者均选用重建钛板,术中未贴附锁骨解剖形态进行塑形,反复塑形可导致金属疲劳,降低了钛板的强度;同时,患侧肩关节术后过早活动增加了钛板的受力以致发生断裂。因此,再次固定时依据个体情况,内固定物分别选择了锁定加压钛板、锁定解剖钛板、3.0mm克氏针及锁定重建钛板,同时术中取自体髂骨植骨,并延长了术后制动时间、避免患肢过早负重活动。5号患者初次固定采用的钛板工作距离过短,螺钉距离骨折断端太近,因此无法抗拒锁骨在肩胛带活动时产生的扭转力量而发生松动失效,再次手术时更换为相对加长的锁定重建钛板并尽量避免螺钉距离骨折线过近。8号患者为切出右锁骨上区肿物而行锁骨截骨术,术后采用解剖型锁定钛板固定,3个月后发生不愈合,更换内固定后取自体髂骨植骨,其发生原因可能与切除肿物时对周围软组织的剥离与破坏导致血供受损有关。
7号及10号均为右锁骨远端骨折术后并发症患者。7号患者发生骨折不愈合的主要原因是术中骨折复位不良,双纽扣钢板的缝线磨断导致内固定失效,同时纽扣钢板仅重建了喙锁垂直方向的稳定性,但对于水平方向的单纯喙锁固定并不能将不稳定骨折完全转变为稳定骨折,也是导致这一并发症的原因之一。10号是采用锁骨远端解剖锁定板治疗右锁骨远端骨折的48岁女性患者,在术后14d出现锁骨远端螺钉松动退出,由于该患者患有肾功能衰竭、糖尿病,且自身处于更年期状态,结合其自身疾病以及生理上的特殊时期,考虑该患者骨质疏松导致螺钉的把持力度下降,同时锁骨远端螺钉数量偏少,引起内固定失效,故再次手术时在锁骨远端增加了螺钉数量,以实现坚强固定。有4例女性患者(9,13,16和17号)在锁骨骨折术后患侧锁骨在原骨折部位或内固定周围再次发生骨折,这主要与内固定的类型、拆除内固定的时间、术后未采取制动保护、患侧肩关节过度活动或再次受外伤有关。王晓波等认为男女锁骨解剖形态特点有很大不同:女性锁骨的总长度及各部分长度均较短,因此应选择较短的接骨板;近段最大宽度、中段最小宽度和远段最大宽度也偏小。这也可能是女性锁骨术后强度下降且易发生再骨折的一个原因。针对此类并发症大多主张取出原有内固定后清除死骨,对骨折断端进行新鲜化处理,复位后再次行内固定治疗的同时进行断端自体植骨。2号患者为锁骨中段骨折重建钛板内固定患者,术后4个月出现骨折不愈合,经上述内固定取出、断端新鲜化处理后更换内固定为锁定解剖钛板,同时置入自体髂骨,效果良好。
此外,2例患者(12和15号)在行锁骨内固定取出后出现伤口愈合不良,局部分泌物细菌培养有1例表皮葡萄球菌感染,2例患者均为35岁以下青年男性,自身健康状况良好,术前无任何合并症,各项检查化验指标未见明显异常,其中1例行皮肤皮下组织清创术,另1例行内固定取出、清创术,均经过抗感染治疗后痊愈,因而此类并发症发生可能与锁骨区放置内固定后皮肤更加薄弱、手术操作不规范有关,严格规范的无菌操作并注意保护骨折区域周围软组织是预防此类并发症的主要措施。11号患者在26年前因肺减容手术行锁骨近端截骨术,现内固定钢丝外露,未见明显感染迹象,予取出后清创关闭伤口,愈合良好。这主要由于内固定长期与皮肤、软组织发生摩擦有关,在条件允许的情况下及时取出可能影响皮肤和软组织的内固定可避免此类并发症的发生。
综上所述,锁骨骨折并发症的发生原因较多,手术并发症通常与内固定的选择不当及术中操作不当有关。因此,应依据骨折类型选择合适种类及长度的内固定材料并避免过度塑形、减少对骨折断端血运的破坏,术中遵循严格规范的无菌操作,术后患侧肩关节予以制动保护,科学地指导功能康复锻炼,有助于降低术后并发症的发生率。
[1]Robinson CM.Fractures of the clavicle in the adult.Epidemiology and classiflcation [J].J Bone Joint Surg Br,1998,80(3):476-484.
[2]Nordqvist A,Petersson C.The incidence of fractures of the clavicle[J].Clin Orthop Relat Res,1994,300:127-132.
[3]Postacchini F,Gumina S,De Santis P,et al.Epidemiology of clavicle fractures[J].J Shoulder Elbow Surg,2002,11(5):452-456.
[4]Zlowodzki M,Zelle BA,Cole PA,et al.Treatment of acute midshaft clavicle fractures:systematic review of 2144 fractures:on behalf of the Evidence-Based Orthopaedic Trauma Working Group[J].J Orthop Trauma,2005,19(7):504-507.
[5]Evaniew N,Simunovic N,Mckee M D,et al.Cochrane in CORR?:Surgical versus conservative interventions for treating fractures of the middle third of the clavicle[J].Clin Orthop Relat Res,2014,472(9):2579-2585.
[6]Ricci WM,Black JC,McAndrew CM.et al.What′s new in orthopaedic trauma?[J].J Bone Joint Surg Am,2015,97(14):1200-1207.
[7]Lenza M,Buchbinder R,Johnston RV,et al.Surgical versus conservative interventions for treating fractures of the middle third of the clavicle(Review)[J].Cochrane Database Sys Rev,2013,6(6):3108-3113.
[8]Andermahr J,Jubel A,Elsner A,et al.Malunion of the clavicle causes significant glenoid malposition:aquantitative anatomic investigation[J].Surg Radiol Anat,2006,28(5):447-456.
[9]Edelson JG.The bony anatomy of clavicular malunions[J].J Shoulder Elbow Surg,2003,12:173-178.
[10]Ledger M,Leeks N,Ackland T,et al.Short malunions of the clavicle:an anatomic and functional study [J].J Shoulder Elbow Surg,2005,14(4):349-354.
[11]McKee MD,Wild LM,Schemitsch EH.Midshaft malunions of the clavicle[J].J Bone Joint Surg Am,2003,85(5):790-797.
[12]Wang K,Dowrick A,Choi J,et al.Post-operative numbness and patient satisfaction following plate fixation of clavicular fractures[J].Injury,2010,41(10):1002.
[13]Vanbeek C,Boselli KJ,Cadet ER,et al.Precontoured plating of clavicle fractures: decreased hardware-related complications?[J].Clin Orthop Relat Res,2011,469(12):3337-3343.
[14]Alshameeri ZA,Katam K,Alsamaq M,et al.The outcome of surgical fixation of mid shaft clavicle fractures;looking at patient satisfaction and comparing surgical approaches[J].Int J Shoulder Surg,2012,6(3):76-81.
[15]Campochiaro G,Tsatsis C,Gazzotti G,et al.Displaced midshaft clavicular fractures:surgical treatment with a precontoured angular stability plate [J].Musculoskelet Surg,2012,96(1):21-26.
[16]Mckee MD,Kreder HJ,Mandel S,et al.Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures.A multicenter,randomized clinical trial[J].J Bone Joint Surg Am,2007,89(1):1-10.
[17]Shin SJ,Do NH,Jang KY.Risk factors for postoperative complications of displaced clavicular midshaft fractures[J].J Trauma Acute Care Surg,2012,72(4):1046-1050.
[18]Fridberg M, Ban I,Issa Z, et al.Locking plate osteosynthesis of clavicle fractures:complication and reoperation rates in one hundred and five consecutive cases[J].Int Orthop,2013,37(4):689.
[19]Altamimi SA,Mckee MD.Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures.Surgical technique[J].Orthop J China,2007,89(8):1866-1867.
[20]Bstman O,Manninen M,Pihlajamki H.Complications of plate fixation in fresh displaced midclavicular fractures[J].J Trauma,1997,43(5):778-783.
[21]Poigenfürst J,Rappold G,Fischer W.Plating of fresh clavicular fractures:results of 122operations[J].Injury Int J Care Injure,1992,23(4):237-241.
[22]Schiffer G,Faymonville C,Skouras E,et al.Midclavicular fracture:not just a trivial injury:current treatment options[J].Dtsch Arztebl Int,2010,107(41):711-717.
[23]Shin SJ,Do NH,Jang KY.Risk factors for postoperative complications of displaced clavicular midshaft fractures[J].J Trauma Acute Care Surg,2012,72(4):1046-1050.
[24]Assobhi JE.Reconstruction plate versus minimal invasive retrograde titanium elastic nail fixation for displaced midclavicular fractures[J].J Orthop Traumatol,2011,12(4):185-192.
[25]Fu TH,Tan BL,Liu HC,et al.Anatomical reduction for treatment of displaced midshaft clavicular fractures:knowles pinning vs.reconstruction plating[J].Orthopedics,2012,35(1):23-30.
[26]章浩,贺倩芸,王光超,等.锁骨骨折内固定失败的原因分析及其补救措施 [J/CD].中华肩肘外科电子杂志,2016,4(2):82-86.
[27]Szpalski M,Gunzburg R.Recombinant human bone morphogeneticprotein 2:an ovelosteo inductive alternative to autogenous bone graft?[J].Acta Orthop Belg,2005,71(2):133-148.
Analyses and countermeasures of complications in patients with clavicle fractures
Zhang Xiaomeng,Chen Jianhai,Wang Yanhua,Kou Yuhui,Fu Zhongguo,Zhang Dianying.Department of Orthopedics and Traumatology,Peking University People′s Hospital,Beijing 100044,China
Zhang Dianying,Email:zdy8016@163.com
BackgroundClavicle fracture is one of the most common fractures,and its incidence rate weights about 2.6%-4.0%of total body fractures.The traditional view believes that most of the clavicle fractures can be managed well via conservative treatment.However,a Meta-analysis by Zlowodzki et al.showed that the incidence of nonunion for clavicle fractures with non-surgical treatment was approximately 5.9%.Most of the patients with clavicle fractures of significant shift(shift or shortening of more than 2cm)and comminuted bone fractures(multiple fractures with more than 3fragments)are currently recommend with surgery to lower the incidence of complications,but there are still some risks.Ricci et al.reported that the reoperation of mid-shaft clavicle fractures with previous open reduction and internal fixation was caused by nonunion,deep infection and malunion,the complications that had an incidence rate much lower than that of the complications caused by conservative treatments.Nowadays,there is still a lack of clinical guidelines for the standardized treatment of clavicle fractures.In this study,we conducted a retrospective analysis on 17cases of clavicle fractures with postsurgical complications to summarize causes of complications and to take relevant measures.Methods(1)General data.From January 1999to September 2016,17out of 465cases of treated clavicle fractures were found with complications.A retrospective study was conducted based on indicators including gender,age,affected side,causes of injury,occurring time of complications and related retreating measures ,major combined diseases,therapeutic measures,duration of hospitalization and discharge conditions.17patients(9males and 8females)were included in the group of this study,and the average age was(43.53±13.01)years(20-69years).10cases had the left side affected,and 7cases had the right side affected.Trauma was the cause of primary cause for all patients,including fall injury(13cases),injury by traffic accidents(2cases)and iatrogenic clavicle fractures(2cases).16patients
the surgical treatment,and 1patient was treated conservatively due to surgical contraindications.In addition,11cases occurred in daily activities without any obvious trauma cause;1case occurred with repeated fall injury;1case occurred during overloading of the affected limb;2cases had poor wound healing due to suspected infection;1case had exposure of internal fixator because of the long-term friction between internal fixator and subcutaneous tissue/skin.(2)16cases received further surgical treatments.The therapeutic measures included:3 cases of removal of internal fixator and reopening for reduction of internal fixation with autologous bone graft;4cases of removal of internal fixator and reopening for reduction of internal fixation without bone graft;4cases of opening for reduction of internal fixation with iliac crest bone graft;1 case of skin and soft tissue debridement after removal of internal fixator;1case of internal fixator removal;1case of skin and soft tissue debridement.Another patient did not receive the surgical treatment due to contraindications.(3)Postoperative management.The affected shoulder of all patients was immobilized with forearm sling postoperatively for 2weeks.The active and passive movements of shoulder were gradually restored 2weeks after the operation,and the pragmatic functional training was allowed 6to 8weeks later.One patient with conservative treatment had clavicle malunion.Thus,the active and passive activities of affected shoulder were no longer limited.The only request was to avoid weight-bearing of the affected upper limb.(4)Statistical analysis.All data were collected using Microsoft Excel 2016,and the software SPSS 20.0was used for data analysis and process.The measurement data were expressed as mean±standard deviation.Results The 17patients in this study accounted for 3.66%of the total patients with clavicle fractures,and the length of stay ranged from 3 to 36days.According to Craig classification:13cases were typeⅠfractures;3cases were typeⅡfractures;1case was typeⅢfractures.Most of the complications occurred 20days to 1year after the surgery,and only 1case of iatrogenic fractures occurred 26years postoperatively.5cases had medical complications,including 3cases with more than 3complications.9cases had fracture nonunion,including 4cases(No.1,3,6and 14)of plate fractures,2cases(No.5and 10)of internal fixator loosening and 3cases(No.2,7and 8)of simple fracture nonunion;3cases(NO.13,16and 17)had clavicle fractures at the original position after plate removal;2cases(No.12and 15)had poor wound healing;1case(No.11)had exposure of internal fixator;1cases(NO.19)had fresh clavicle fractures due to trauma of the operated side;another one(No.4)with conservative treatments had fracture malunion due to surgical contraindication.Out of the 16patients who underwent reoperation,7 patients were performed with autologous iliac bone grafting.Conclusions The causes of complications of clavicular fractures varies,which usually relate to impropriate selection of internal fixators or intraoperative operation.Therefore,proper type and length of internal fixators should be chosen according to the fracture classification.Also,excessive remodeling of plates should be avoided as well.Blood supply of the fracture ends should be protected,and strict aseptic operative regulations should be followed during the surgery.The affected shoulder should be protected for immobilization,and functional rehabilitations should be guided scientifically after operation.With these beneficial measures,the postoperative complication rate can be lowered.
Clavicle fractures;Complications;Conservative treatment;Surgical treatment
2016-12-14)
(本文编辑:胡桂英;英文编辑:陈建海、张晓萌、张立佳)
10.3877/cma.j.issn.2095-5790.2017.01.005
卫生公益性行业科研专项(201002014);教育部创新团队项目(IRT1201);国家自然科学基金主任基金(31640045);国家自然科学基金面上项目(31671246);国家重点研发计划专项(2016YFC1101604)
100044 北京大学人民医院创伤骨科
张殿英,Email:zdy8016@163.com
张晓萌,陈建海,王艳华,等.锁骨骨折患者并发症的原因分析与对策 [J/CD].中华肩肘外科电子杂志,2017,5(1):22-28.