长期住院失能老年患者感染性疾病的调查分析
张长尧 赵坤 祝筱姬
长期住院失能老年患者感染性疾病的调查分析
张长尧 赵坤 祝筱姬
目的 分析长期住院失能老年患者感染性疾病的发病情况,为有效防治提供参考。方法 回顾性调查2011-03—2015-12在某院住院的571例失能老年患者的感染发生率,对其进行统计学分析。结果 235例感染者中,失能老年患者男女感染率(41.89%,40.09%)和60~99岁各年龄段之间的感染率(38.89%~51.47%)均呈高水平。失能老年患者感染发生率性别之间以及各年龄段之间比较,差异无统计学意义,P>0.05。感染性疾病的构成比以上呼吸道感染最高(48.9%),之后依次为泌尿系感染(13.6%)、肺部感染(13.2%)和肠道感染(8.1%)等。结论 长期住院失能老年患者容易发生呼吸道、泌尿系和肠道感染,规范失能老年患者的呼吸道、尿道、肠道管理,可有望降低其感染的发生率。
老年人;失能;感染;发生率
老年人常患多种慢性疾病,且共存病和不利因素如失能、住院、功能衰退、死亡率之间呈线性关系[1-5]。老年人失能者约占全世界总人口的15%,其认知损害可能与失能有关[6]。荟萃分析表明,轻微认知损害到老年痴呆的年转换率为5.2%(95%CI2.9%~8.0%)。相反,健康人到老年痴呆的年转换率则为0.43%[7]。在我国,老龄化的问题已成为突出的社会问题,住院康复期间失能老年患者感染的发生对医生来说是一种挑战。本研究通过对长期住院失能老年患者感染性疾病的发病情况进行调查分析,旨在为有效的防治提供参考。
1 资料与方法
1.1 临床资料 调查对象为2011-03—2015-12在我院住院治疗的失能老年患者571例中发生感染的235例,其中男性142例,女性93例;年龄63~95岁,平均(81.9±5.2)岁。患脑血管疾病82例次,冠心病62例次,高血压病52例次,糖尿病49例次。住院32~183 d,平均103.8 d。患1种疾病者25例,占10.6%,患2种疾病者123例,占52.3%,患3种以上疾病者87例,占37.0%。所有患者生活不能完全自理,基础疾病稳定,按照《日常生活能力评定量表》评定<60分。感染标准以卫生部颁布的《医院感染诊断标准》(2001年版)为诊断依据。
1.2 方法 对235例长期住院失能老年患者感染相关资料进行列表分析,具体包括性别、年龄、感染部位。失能判断标准:按Botoseneanu[8]和Murtagh[9]打分标准计算(0~12分)。
1.3 统计处理 使用SPSS 16.0软件对数据进行统计学分析,数据资料以百分数表示,采用χ2检验,P<0.05为差异有统计学意义。
2 结果
235例感染者中,失能老年患者男女感染率(60.4%,39.6%)和60~99岁各年龄段之间的感染率(15.3%、43.0%、26.8%、14.8%)均呈高水平。失能老年患者感染发生率与性别和各年龄段之间比较,差异无统计学意义(P>0.05)。感染性疾病的构成比以上呼吸道感染最高,占48.9%,之后依次为泌尿系感染占13.6%,肺部感染占13.2%,肠道感染占8.1%,口腔感染占6.8%,其他感染占9.4%(表1)。
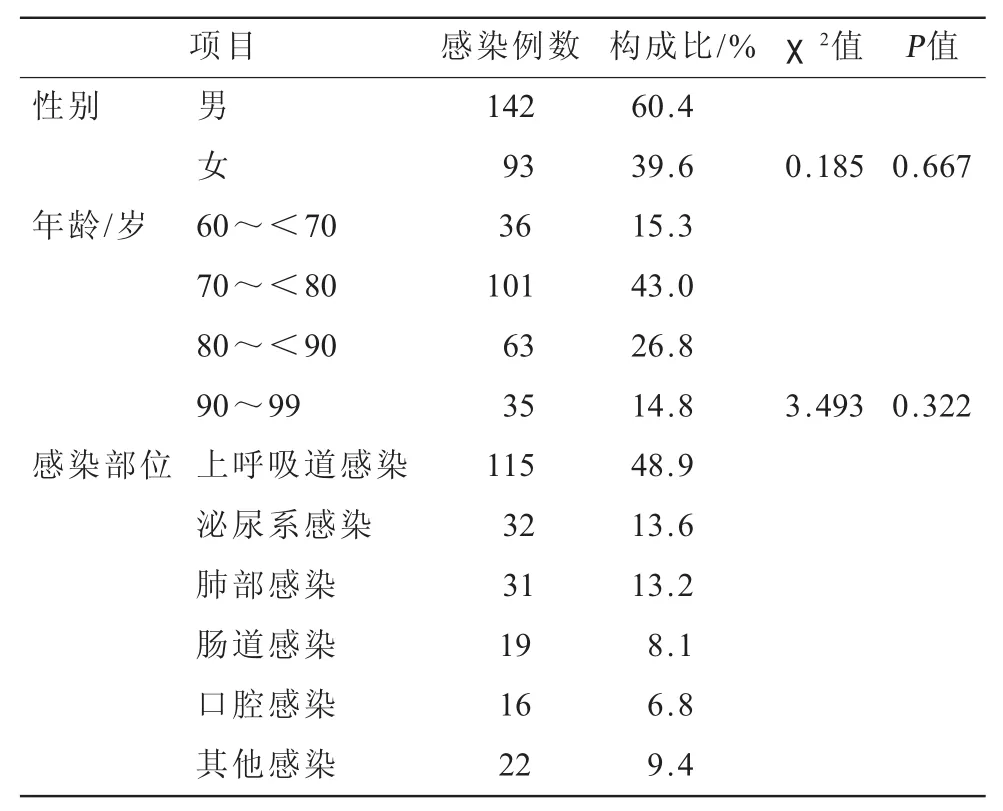
表1 235例失能老年患者感染相关资料及构成比
3 讨论
3.1 年龄和失能与感染率的关系 Shimada等[6]将老年人认知力分为:认知健康、轻微认知损伤、广泛认知损伤、痴呆。统计4 290例[年龄(71.8±5.3)岁,51%为女性]老年人,广泛认知损伤占13.9%,轻微认知损伤占17.4%。认为虽然轻微认知损害与失能之间的关系尚不清楚,但提示轻微认知损害是失能发展的一种危险因素[6]。Lopez等[10]和Rait等[11]调查2 470例和15 051例老年人中,轻微认知损害者占18.6%,广泛认知损害者占18.3%。一组法国2 350例老年人调查资料显示,70~79岁失能者为5.5%,80~89岁为14.1%,>90岁为33%[12]。研究显示,老年失能发生率与性别无关,年龄是一项重要因素,每10年增加2%的相对风险[13]。本研究发现,在235例感染者中,失能老年患者男女之间和各年龄段之间感染的发生率均呈高水平(38.89%~51.47%),但差异无统计学意义。这些结果表明,失能老年患者容易发生感染,但性别和年龄间与感染率不存在统计学的关联性。文献报道,>70岁老人失能衰退现象女性比男性出现快,但女性上、下肢体的活动能力比男性强[8],这足以解释本研究结果中失能老年患者男性感染发生率略高于女性的缘故,本研究结果与Arnau报道一致[13]。失能老年患者共存病多,机体免疫力低下,加之院内交叉感染概率增加等不利因素,均可导致失能老年患者住院期间感染率增加的可能性[14]。
3.2 感染部位与失能的关系 目前,对高龄老人的研究主要聚焦在人口学特征、住院前、并存病、老人状况、功能评价[14]。急性心肌梗死、心衰、肺炎是导致老年人死亡的主要因素[15]。住院老人多患获得性肺炎,肺炎球菌是其主要致病菌之一[15]。其次为吸入性肺炎,其中老年胃反流性疾病是一种隐患[16-17]。在老年失能和共存病的情况下,肺炎的死亡率明显增加[18]。过去认为,获得性肺炎的高死亡率与低营养状态呈相关性,改善营养状态可降低肺炎的死亡率[19-21],但现在通过回归方程分析发现,营养状态和住院时间与肺炎的严重性无相关性[22]。研究发现,血清乙酰胆碱水平与肺炎的严重性呈负相关。乙酰胆碱可抑制巨噬细胞和其他免疫细胞中的细胞因子产生,并通过神经递质和巨噬细胞的通路发挥其调节作用[23]。文献报道,80岁女性老年人尿路感染发生率为20%,男性则为5%~10%[24]。长期留置导尿管老年人尿路感染发生率为5%~10%,且女性居多[25-27]。经饮食摄入肠内的微生物含有遗传和免疫信号,可影响宿主的代谢、免疫及炎症。若先天性免疫系统和肠微生物畸变,则可导致复杂疾病的发生。因此,肠内的微生物被称为信号中枢[28]。肠道炎症与微生物的失调有关,可谓生态失调[29]。本研究显示,失能老年患者感染部位构成比以上呼吸道感染最高,占49%,之后依次为泌尿系感染占13.6%,肺部感染占13.2%,肠道感染占8.1%等。上呼吸道是呼吸系统的门户,来自外界的病毒或细菌等病原微生物对呼吸系统的损害以鼻、咽、喉器官首当其冲,自然上呼吸道也就成为炎症反应的重要场所。因此,对失能老年患者来讲,自身抵抗力下降和缺乏有效的防护成为肺部感染发生的必要条件。此外,气管切开、反复吸痰、留置胃管等侵入性损伤也增加了获得性肺炎的易感因素。失能老年患者长期留置导尿管,即使2周更换一次和经常膀胱冲洗,尿路感染发生率仍居高不下。肠道感染可能与营养摄入不足或长期应用抗生素及糖皮质激素导致菌群失调有关。
综上所述,长期住院康复失能老年患者的感染相关资料表明,失能老年患者感染发生率呈高水平,但与性别和年龄无直接相关性,而是取决于失能老年患者的自身免疫力、共存病、营养状况以及医院的护理和抗生素应用的管控。有效地控制失能老年患者感染的发生率,可延长其生存率。把规范呼吸道、尿道、肠道的管理作为重点,有望降低失能老年患者感染的发生率。
[1]Di Bari M,Virgillo A,Matteuzzi D,et al.Predictive validity of measures of comorbidity in older community dwellers:the insufficienza cardiaca negli anziani residenti a dicomano study[J].J Am Geriatr Soc,2006,54(2):210-216.
[2]Brilleman SL, Salisbury C.Comparing measures of multimorbidity to predict outcomes in primary care:a cross sectional study[J].Fam Pract,2013,30(2):172-178.
[3]Boeckxstaens P,Vaes B,Van Pottelbergh G,et al.Multimorbidity measures were poor predictors of adverse events in patients aged ≤80 years:a prospective cohort study[J].J Clin Epidemiol,2015,68(2):220-227.
[4]BoeckxstaensP,VaesB,Legrand D,etal.Therelationship of multimorbidity with disability and frailty in the oldest patients:a cross-sectional analysis of three measures of multimorbidity in theBELFRAIL cohort[J].EurJGen Pract,2015,21(1):39-44.
[5]Boeckxstaens P,Vaes B,De Sutter A,et al.A high sense of coherence as protection against adverse health outcomes in patients aged 80 years and older[J].Ann Fam Med,2016,14(4):337-343.
[6]Shimada H,Makizako H,Doi T,et al.Cognitive impairment and disability in older japanese adults[J].PLoS One,2016,11(7):e0158720.
[7]MitchellAJ,Shiri-Feshki M.Rate ofprogression ofmild cognitive impairment to dementia-meta-analysis of 41 robust inception cohort studies[J].Acta Psychiatr Scand,2009,119(4):252-265.
[8]Botoseneanu A,Allore HG,Mendes de Leon CF,et al.Sex differences in concomitant trajectories of self-reported disability and measured physical capacity in older adults[J].J Gerontol A Biol Sci Med Sci,2016,71(8):1056-1062.
[9]Murtagh KN,Hubert HB.Gender differences in physical disability among an elderly cohort[J].Am JPublic Health,2004,94(8):1406-1411.
[10]LopezOL,JagustWJ,DeKoskyST,etal.Prevalenceand classification of mild cognitive impairment in the Cardiovascular Health Study Cognition Study:part 1[J].Arch Neurol,2003,60(10):1385-1389.
[11]Rait G,Fletcher A,Smeeth L,et al.Prevalence of cognitive impairment:results from the MRC trial of assessmentand management of older people in the community[J].Age Ageing,2005,34(3):242-248.
[12]HerrM,Arvieu JJ,Robine JM,etal.Health,frailty and disability after ninety:Results of an observational study in France[J].Arch Gerontol Geriatr,2016(66):166-175.
[13]Arnau A,Espaulella J,Serrarols M,et al.Risk factors for functional decline in a population aged 75 years and older withouttotaldependence:a one-yearfollow-up[J].Arch Gerontol Geriatr,2016(65):239-247.
[14]Wang HH,Shyu YL,Chang HY,et al.Prevalence,characteristics,and acute care utilization of disabled older adults with an absence of help for activities of daily living:Findings from a nationally representative survey[J].Arch Gerontol Geriatr,2016(67):28-33.
[15]Shashank RJ,SamikaSJ,Siddharth NS.Pneumococcalvaccine in diabetes:relevance in India[J].J Assoc Physicians India,2015,63(4):34-35.
[16]Heppner HJ.Aspiration pneumonia in elderly patients:treacherous and often fatal[J].MMW Fortschr Med,2016,158(8):20.
[17]Tsukanov VV,Kasparov EV,Onuchina EV,et al.The frequency and clinical aspects of extraesophageal syndromes in elderly patients with gastroesophageal reflux disease[J].Ter Arkh,2016,88(2):28-32.
[18]Holter JC,Ueland T,Jenum PA,etal.Risk factors for long-term mortality after hospitalization for community-acquired pneumonia:A 5-year prospective follow-up study[J].PLoS One,2016,11(2):e0148741.
[19]HedlundJ,HanssonLO,OrtqvistA.Short- andlong-term prognosisformiddle-aged and elderly patientshospitalized with community-acquired pneumonia:impact ofnutritional and inflammatory factors[J].Scand J Infect Dis,1995,27(1):32-37.
[20]Tejera A,Santolaria F,Diez ML,etal.Prognosisof community acquired pneumonia(CAP):value of triggering receptor expressed on myeloid cells-1(TREM-1)and other mediators ofthe inflammatory response[J].Cytokine,2007,38(3):117-123.
[21]Corrales-Medina VF,Valayam J,Serpa JA,et al.The obesity paradox in community-acquired bacterial pneumonia[J].Int J Infect Dis,2011,15(1):e54-57.
[22]Akuzawa N,Naito H.Nutritional parameters affecting severity of pneumonia and length of hospital stay in patients with pneumococcal pneumonia:a retrospective cross-sectional study[J].BMC Pulm Med,2015(15):149.
[23]Pohanka M.Inhibitors of acetylcholinesterase and butyrylcholinesterase meet immunity[J].IntJMolSci,2014,15(6):9809-9825.
[24]Nicolle LE.Urinary tractinfectionsin the olderadult[J].Clin Geriatr Med,2016,32(3):523-538.
[25]Nicolle LE.Urinary tractinfectionsin the elderly[J].Clin Geriatr Med,2009,25(3):423-436.
[26]Nicolle LE.Catheterassociated urinary tractinfections[J].Antimicrob Resist Infect Control,2014(3):23.
[27]NicolleLE.Catheter-related urinary tractinfection:practical management in the elderly[J].Drugs Aging,2014,31(1):1-10.
[28]Thaiss CA,Zmora N,Levy M,etal.The microbiome and innate immunity[J].Nature,2016,535(7610):65-74.
[29]B umler AJ,Sperandio V.Interactions between the microbiota and pathogenic bacteria in the gut[J].Nature,2016,535(7610):85-93.
Objective To analyze the morbidity of infectious diseases among long-stay senile patients with disability,so as to provide reference for effective prevention and treatment.Methods The incidence rates of infectious diseases among 571 long-stay senile patients with disability at a certain hospital from March 2011 to December 2015 were investigated retrospectively and analyzed statistically.Results In the 235 infected patients,the infection rates in the senile patients with disability between men and women(41.89%,40.09%)and between 60~99 years old(38.89%~51.47%)took on very high level.The infection rates in the senile patients with disability had no difference of statistical significance in different sexes and ages(P>0.05).The constituent ratio of infectious diseases showed that the upper respiratory tract infection was the highest(48.9%),then followed by urinary infection(13.6%),pulmonary infection(13.2%),and intestinal infection(8.1%),and so on.Conclusion Long-stay senile patients with disability are likely to have the upper respiratory tract infection,urinary infection,and intestinal infection.Regulation on the respiratory,urinary and intestinal tract management can help decrease the incidence rate of infection.
The senile;Disability;Infection;Incidence rate
2016-12-21)
1005-619X(2017)06-0656-03
10.13517/j.cnki.ccm.2017.06.045
266071 济南军区青岛第二疗养院慢性病康复科
祝筱姬