潮汕地区肥胖与乳腺癌患者预后相关性的研究
梁海燕 张苏伟 陈晓红

[摘要] 目的 分析潮汕地區体重指数(BMI)和乳腺癌患者预后之间的关系。 方法 回顾性收集2008年1月~2010年12月于我院就诊的236例潮汕地区乳腺癌患者。收集所有乳腺癌患者的身高、体重、年龄、乳腺癌临床分期、淋巴结转移情况及组织病理等级等基本资料,计算BMI,根据BMI水平分为低体重组、正常组、偏胖组和肥胖组。随访到2016年12月,患者乳腺癌复发死亡则随访终止,平均随访6.8年。 结果 不同组间乳腺癌患者的年龄、病理分级和临床分期比较,均无显著差异(P>0.05),但不同组间淋巴结转移情况的差异具有统计学意义(P<0.05)。截至2016年12月随访结束,共有99名患者死于乳腺癌。低体重组、正常组、偏胖组和肥胖组的死亡率分别为 29.41%,28.33%,47.76%和53.33%。随访结束时,低体重组[(54.6±2.18)个月]和正常组[(52.6±1.76)个月]乳腺癌患者生存时间无显着差异(P>0.05),高于偏胖组[(45.8±2.04)个月]和肥胖组[(41.2±1.96)个月],偏胖组乳腺癌患者的生存时间略高于肥胖组。 结论 潮汕地区乳腺癌患者的预后情况与患者自身体重有一定关联,维持正常体重可降低乳腺癌病死率,还可提高乳腺癌患者的预后情况。
[关键词] 肥胖;乳腺癌;预后情况;体重指数;死亡率
[中图分类号] R737.9 [文献标识码] A [文章编号] 1673-9701(2017)13-0004-03
[Abstract] Objective To analyze the relationship between body mass index(BMI)and prognosis of breast cancer patients of Chaoshan district. Methods A total of 236 breast cancer patients of Chaoshan district admitted in our hospital from January 2008 to December 2010 were collected respectively. The basic information including the height, weight, age, breast cancer clinical stage, lymph node metastasis and histopathological grade of all breast cancer patients were collected. And the BMI was calculated. The patients were divided into low body weight group, normal group, partial fat group and obesity group according to the level of BMI. The patients were followed up to December 2016,and the follow-up was terminated when the patient died of breast cancer recurrence, with the average follow-up of 6.8 years. Results There were no significant differences in age, pathological grade and clinical stage between different groups(P>0.05), but the difference in lymph node metastasis between different groups was statistically significant(P<0.05). The follow-up ended in December 2016 ,and a total of 99 patients died of breast cancer.The mortality rates of low weight group, normal group, partial fat group and obesity group were 29.41%, 28.33%, 47.76% and 53.33% respectively. At the end of follow-up, there was no significant difference in survival time between low body weight group[(54.6±2.18) months] and normal group[(52.6±1.76) months](P<0.05), higher than that in partial fat group[(45.8±2.04) months]and obese group[(41.2±1.96) months]. And the survival time of partial fat group was slightly higher than that of the obese group. Conclusion The prognosis of patients with breast cancer in Chaoshan district is related to the weight of patients. Maintaining body weight not only can reduce the mortality of breast cancer, but also improve the prognosis of breast cancer patients.
[Key words] Obesity; Breast cancer; Prognosis; Body mass index; Mortality
近年来乳腺癌发病率呈逐年上升趋势,其发病率和死亡率在妇科肿瘤中居首位。随着生活水平的提高和饮食习惯的改变,肥胖与乳腺癌的相互关系越来越受到关注[1]。 一些研究表明,体重指数(BMI)与乳腺癌的发病关系密切[2]。国外相关报道较多,由于我国的饮食习惯和妇女的肥胖水平与西方国家相比存在很大差异,本研究旨在探讨潮汕地区乳腺癌患者的体重和乳腺癌预后之间的关系,为本地区乳腺癌患者改善预后提供参考资料,现报道如下。
1 资料与方法
1.1 一般资料
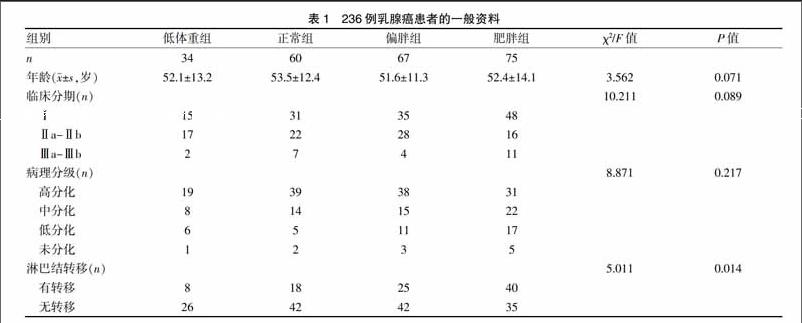
收集2008年1月~2010年12月于我院接受乳腺癌手术治疗的潮汕地区女性患者共236例,年龄34~72岁,平均年龄52.6岁。低体重组34例、正常组60例、偏胖组67例、肥胖组75例。纳入标准:经组织病理活检明确诊断为乳腺癌患者;且排除以下情况的病例:怀孕或哺乳期妇女;过敏性体质患者;糖尿病患者等。收集患者的身高、体重、年龄、乳腺癌临床分期、全身淋巴结转移情况、组织病理学分级等基本资料。随访时间为乳腺癌手术后至2016年12月,记录患者预后情况。四组间的年龄,病理分级,临床分期相比较无显著性差异(P>0.05)。而组间淋巴结转移情况比较有显著性差异(P<0.05),见表1。
1.2 评价标准
依据WHO关于肥胖的定义标准:BMI<18.5 kg/m2定义为低体重组,BMI处于(18.5~24.9)kg/m2之间定义为正常组,BMI处于(25.0~30.0)kg/m2间定义为偏胖组,BMI>30.0 kg/m2组定义为肥胖组,共四组。[注:BMI=体重(kg)/身高2(m2)]。
1.3 统计学方法
所有资料均采用SPSS 16.0进行统计学分析。计量资料以(x±s)表示,采用F检验或t检验,计数资料采用χ2检验,P<0.05为差异有统计学意义。患者的生存率分析则用Kaplan-Meier分析。
2 结果
2.2 各组患者体重指数与生存情况的相关关系分析
236例乳腺癌患者平均随访6.8年,共有99例乳腺癌患者死于复发或者转移癌,死亡率为41.95%,肥胖组死亡率最高,正常组最低,肥胖组死亡率为正常组的1.88倍。各组间比较,差异有统计学意义(χ2=11.638,P=0.009)。见表2。
2.3 BMI与乳腺癌预后的关系
通过Kaplan-Meier分析得出,低体重组的平均生存时间为(54.6±2.18)个月,正常组的平均生存时间为(52.6±1.76)个月,偏胖组的平均生存时间为(45.8±2.04)个月,肥胖组的平均生存时间为(41.2±1.96)个月。可见,不同的BMI乳腺癌患者的预后不同(F=2.08,P<0.05),低体重和正常体重乳腺癌患者的生存时间无显著差异(t=1.38,P>0.05),但与偏胖组和肥胖组相比较,生存时间明显较高,差异具有统计学意义(F=2.45,P<0.05);且偏胖组乳腺癌患者的生存时间也较肥胖组略高,差异有统计学意义(t=3.01,P<0.05)。
3 讨论
近年来,超重和肥胖对乳腺癌生存时间的影响越来越引起医学界的关注[3]。Li HT等[4]通过218例辅助化疗患者的回顾性分析结果显示,BMI≥30 kg/m2是乳腺癌早期预后(包括复发,转移和死亡)的独立危险因素。这一结果也得到了Bao PP等[5]的大样本研究的支持。Shin A等[6]通过分析1169例新辅助化疗晚期乳腺癌(中位随访时间为4.1年),发现肥胖乳腺癌患者(BMI≥30 kg/m2)比正常体重患者的生存时间短。Key TJ等[7]的8项前瞻性研究的Meta分析结果显示,BMI≥30 kg/m2的乳腺癌患者的存活时间比体重正常者低。Santa-Maria CA等[8]针对中国妇女的研究也显示,超重(BMI≥25 kg/m2)的乳腺癌患者新辅助化疗后存活率低。这些研究表明,超重和肥胖是乳腺癌预后的重要因素,但肥胖影响乳腺癌的预后的机制尚不清楚。
由身体脂肪堆积引起的肥胖患者可促进雄烯二醇转化为雌激素,使血液中的游离雌激素水平升高,而乳腺癌恰恰是雌激素依赖性肿瘤[9]。可见肥胖与乳腺癌具有千丝万缕的关系。其可能的相关机制是[10]:甘油三酯可导致性激素结合球蛋白降低,使得游离雌激素水平升高,雌激素可刺激乳腺细胞增殖,促进乳腺癌复发和转移;高浓度的不饱和脂肪酸血液容易被氧化,导致脂质过氧化产物生成,氧自由基过多,从而引起细胞突变。有研究表明,高密度脂蛋白可以减少酶或非酶途径产生过氧化氢、超氧化物阴离子和羟基自由基,发挥抗癌和抗氧化作用[11]。表明高密度脂蛋白降低将导致乳腺癌患者丧失保护作用[12]。本研究从宏观角度收集潮汕地區乳腺癌患者的初始体重和相关预后因素,用以探讨本地区乳腺癌患者预后与体重之间的关系。据数据分析,发现各组年龄、病理分级、临床分期无显着性差异,但淋巴结转移情况差异有统计学意义。
本研究结果显示,低体重组、正常组、偏胖组和肥胖组的死亡率分别为29.41%、28.33%、47.76%和53.33%,随着体重指数的增加,乳腺癌患者的生存率呈下降趋势,这与国内外大部分研究成果类似[13-16]。Kaplan-Meier分析结果得出,低体重组的平均生存时间为(54.6±2.18)个月,正常组的平均生存时间为(52.6±1.76)个月,偏胖组的平均生存时间为(45.8±2.04)个月,肥胖组的平均生存时间为(41.2±1.96)个月。从各组患者的生存时间可以看出,低体重组和正常组生存预后无差异,但高于偏胖组和肥胖组。雌激素是影响乳腺癌发生和发展的重要因素[17,18]。在绝经后妇女中,脂肪组织是雌激素产生的主要部位,血液雌激素水平与肥胖呈正相关[19]。脂肪组织还可以分泌多种脂肪细胞因子,包括血管内皮生长因子,肝细胞生长因子,白细胞介素-6,肿瘤坏死因子-α,肝素结合表皮生长因子样因子,瘦素和脂联素与乳腺癌发病密切相关[20,21]。脂肪细胞因子水平与生殖力有关,脂肪水平呈正相关。脂肪细胞因子可通过影响血管生成、芳香酶活性、癌转移、细胞增殖等方面影响乳腺癌的发展[22]。一系列流行病学研究表明,肥胖是乳腺癌发病的危险因素[23]。
因此,肥胖在某種程度上是影响乳腺癌患者的预后风险因素。通过这项研究结果的提示可对潮汕地区的乳腺癌患者,特别是肥胖妇女进行体重控制干预,从而降低乳腺癌的复发风险,提高乳腺癌患者的生存时间。
[参考文献]
[1] Sophia H,Salma B,Ivarsson Malin IL,et al. Interactive effect of genetic susceptibility with height,body mass index,and hormone replacement therapy on the risk of breast cancer[J]. BMC Women's Health,2012,12(1):1-10.
[2] Fontanella C,Lederer B,Gade S,et al. Impact of body mass index on neoadjuvant treatment outcome:A pooled analysis of eight prospective neoadjuvant breast cancer trials[J].Breast Cancer Research and Treatment,2015, 150(1):127-139.
[3] Mccarthy AM,Keller B,Kontos D,et al. The use of the Gail model,body mass index and SNPs to predict breast cancer among women with abnormal(BI-RADS 4) mammograms[J]. Breast Cancer Research,2015,17(1):1-6.
[4] Li HT,Han XH,Liu YX,et al.Relationship between body mass index and incidence of breast cancer[J]. International Journal of Clinical & Experimental Medicine,2015,8(7):11549-11553.
[5] Bao PP,Cai H,Peng P,et al. Body mass index and weight change in relation to triple-negative breast cancer survival[J]. Cancer Causes & Control,2016,27(2):229-234.
[6] Shin A,Sandin S,Lof M,et al. Alcohol consumption, body mass index and breast cancer risk by hormone receptor status:Women lifestyle and health study[J]. BMC Cancer,2015,15(1):881-889.
[7] Key TJ, Appleby PN, Reeves GK,et al. Steroid hormone measurements from different types of assays in relation to body mass index and breast cancer risk in postmenopausal women:Reanalysis of eighteen prospective studies[J]. Steroids,2015,99(Pt A):49-55.
[8] Santa-Maria CA,Yan J,Xie XJ,et al. Aggressive estrogen-receptor-positive breast cancer arising in patients with elevated body mass index[J]. International Journal of Clinical Oncology, 2015,20(2):317-323.
[9] Chen MJ,Wu WY, Yen AM,et al. Body mass index and breast cancer:Analysis of a nation-wide population-based prospective cohort study on 1 393 985 Taiwanese women[J].International Journal of Obesity,2015,40(3):524-530.
[10] Smith SA,Claridy MD,Whitehead MS,et al. Factors associated with body mass index among African American breast cancer survivors[J]. Journal of the Georgia Public Health Association,2016,5(3):259-265.
[11] Chlebowski RT,Anderson GL,Aragaki AK,et al. Breast cancer and menopausal hormone therapy by race/ethnicity and body mass index[J].J Journal of the National Cancer Institute,2015,108(2):327-334.
[12] Benn M,Tybj?覸rg-Hansen A,Smith GD,et al. High body mass index and cancer risk-A mendelian randomisation study[J]. European Journal of Epidemiology,2016,31(9):1-14.
[13] Cecchini RS,Swain SM,Costantino JP,et al. Body mass index at diagnosis and breast cancer survival prognosis in clinical trial populations from NRG Oncology/NSABP B-30,B-31,B-34,and B-38[J]. Cancer Epidemiology Biomarkers & Prevention,2015,25(1):51-62.
[14] Pradhan KR,Stump TE,Monahan P,et al. Relationships among attention function,exercise,and body mass index:A comparison between young breast cancer survivors and acquaintance controls[J]. Psycho-Oncology,2015,24(3):325-332.
[15] Keinan-Boker L,Levine H,Derazne E,et al. Measured adolescent body mass index and adult breast cancer in a cohort of 951,480 women[J]. Breast Cancer Research and Treatment,2016,158(1):1-11.
[16] Cakar B,Muslu U,Erdogan AP,et al. The role of body mass index in triple negative breast cancer[J]. Oncology Research & Treatment,2015,38(10):518-522.
[17] Barba M,Pizzuti L,Sperduti I,et al. Body mass index and treatment outcomes in metastatic breast cancer patients treated with eribulin[J]. Journal of Cellular Physiology,2015,231(5):986-991.
[18] Hortobagyi GN. Trastuzumab in the treatment of breast cancer.[J]. BioDrugs,2016,353(2):1734-1740.
[19] Med AI. Screening for breast cancer:U.S. Preventive Services Task Force recommendation statement[J]. Annals of Internal Medicine,2016,154(5):356-364.
[20] Swain SM,Baselga J,Kim SB,et al.Pertuzumab,trastu-zumab,and docetaxel in HER2-positive metastatic breast cancer[J]. New England Journal of Medicine,2015,372(8):724-729.
[21] Butta A,Maclennan K,Flanders KC,et al. Induction of transforming growth factor β1 in human breast cancer in vivo following tamoxifen treatment[J].Cancer Research,2017,52(15):4261-4264.
[22] Cancer AAF. Clinical cancer research:An official journal of the American Association for cancer research[M]. American:The Association, 2013.
[23] Moss SM,Cuckle H,Evans A,et al. Effect of mammographic screening from age 40 years on breast cancer mortality at 10 years' follow-up:A randomised controlled trial[J]. Lancet,2015,368(9552):2053-2058.
(收稿日期:2017-01-15)