Takotsubo Syndrome: Does the Octopus Trap Hide Dangers?
Maria Bergami, Peter Louis Amaduzzi and Raffaele Bugiardini
1Department of Specialistic, Diagnostic and Experimental Medicine (DIMES), Alma Mater University, Bologna, Italy
Introduction
Takotsubo syndrome (TTS) is an acute heart syndrome typically characterized by apical and circumferential mid-ventricular hypokinesia of the left ventricle in the absence of significantly obstructed epicardial coronary arteries [1]. It owes its name to the Japanesetakotsubo, an octopus trap used by Hiroshima fishermen, whose shape closely resembles that of the left ventricle at the end of systole typical of the disease. In many aspects TTS mimics the clinical presentation and ECG findings of an acute coronary syndrome (ACS) [1], thus some of the legitimacy of the distinction between these two disorders was questioned [2]. Nevertheless, TTS is also termed as a cardiomyopathy, even though patients with TTS do not appear to have a primary muscle disorder or common genetic alteration [1].
The current inability to immediately exclude ACS as a possible diagnosis has an obvious impact on the treatment and clinical management of patients with TTS, who may be given drugs with potential adverse effects and without clinical benefit. Beyond these issues, there are many other aspects that need to be studied and clarified. Differently from what was originally believed, TTS is not always benign,and the octopus trap may hide dangers that need to be fully uncovered to effectively protect and treat the patients. Thus, the goal of this review is to analyze the current findings and hypotheses regarding this enigmatic disease, offering preparatory points for the development of future research.
Epidemiology: An Increasingly Recognized Syndrome
Since its first description in 1990 [3], TTS has been observed in several case reports, and more recently many studies have attempted to analyze its frequency in larger cohorts. In 1991 Dote et al. [4] reported five cases of TTS in a study population of 415 consecutive patients with acute myocardial infarction (AMI)who were examined invasively, therefore observing a prevalence of 1.2%. In 2004 a prospective study reported that TTS cases accounted for 2.2% of patients with an initial diagnosis of ST-segment elevation myocardial infarction [5]. Recently, information has emerged whereby the TTS incidence in the United States was assessed with use of data provided by the National Inpatient Sample [6–8]. In particular, Khera et al. [8] analyzed trends in hospitalization, mortality, and characteristics of TTS patients between 2007 and 2012. A three-fold increase in the number of hospitalizations for primary TTS was observed (1642 cases in 2007–5480 in 2012), probably due to a more widespread knowledge of this disease and, consequently, to an increase in diagnoses. Nevertheless,the information gathered from this phenomenon is of the highest clinical value, because it implies that many patients with TTS are still hidden behind an incorrect diagnosis that precludes them from having the right therapies and clinical management.
Clinical Presentation and Triggers:Clues for a Better Understanding of Takotsubo Syndrome
The clinical presentation in TTS closely mimics that of AMI, with symptoms such as chest pain and dyspnea being the most frequent.
Patient Characteristics: A Women’s Disease
Numerous studies have shown that most cases of TTS concern postmenopausal women, who usually account for approximately 90% or more of the cases [7–12]. Brinjikji et al. [12] reported that among the 24,701 patients considered in their study, the mean age was 66.9±30.7 years and men tended to be younger than their female counterparts.
From these data it appears that the pathophysiology of TTS may be related to an alteration in the levels of estrogen. This hormone is known to have an important impact on cardiac health, and studies conducted on rats showed that heart rate and blood pressure during stress are controlled by estrogen [13]. As a consequence, it is possible that an estrogen deficiency, typical of the postmenopausal state, may be a predisposing factor in the development of TTS. This theory is supported by the findings of Sato et al. [14], who reported a case of TTS in a woman with Turner’s syndrome who had low estrogen levels because of her genetic disease.
Estrogen: The Double Face of an Old Ally?
Seemingly in contrast with what has been reported so far, in 2012 Brenner et al. [15] showed that the estradiol concentration at hospital admission was significantlyhigherin TTS patients than in the control groups, although this increase was transient and disappeared at follow-up. This finding may be at least partially explained by the fact that stressful events can increase the peripheral aromatization of androgens to estrogens. According to Brenner et al., long-term or short-term elevation of estradiol concentration in menopausal women could play the aforementioned protective role toward the vessels, without however managing to prevent the final cardiac insult, and inducing TTS rather than AMI.
Unfortunately, further data supporting this theory are currently unavailable. Moreover, the questions this finding leaves unanswered are many: If high levels of estrogen can participate in causing TTS,why is the percentage of fertile women affected by the disease so small? Could this increase in the levels of estrogen have been only a transient effect of stress, rather than a trigger of TTS? Future investigations may provide more clarity on this issue.
Symptoms and Stressors: The Importance of Patient History
As previously mentioned, the symptoms of TTS are not specific enough to differentiate it from ACS.Patients with TTS usually present at the hospital with chest pain, dyspnea, and more rarely, syncope[9, 11, 16], all symptoms that are traditionally associated with AMI.
One of the anamnestic elements that could help in orientating the diagnosis toward TTS is the patient’s history, especially the evidence of stressful physical conditions or emotional events preceding the symptom onset. These types of stressors tend to be present in the large majority of TTS patients [11, 16], and the incidence of TTS rapidly increases in populations recently hit by earthquakes or other calamities [17, 18].Physical triggers tend to have a higher frequency than emotional ones (36.0% versus 27.7%) [11],although the line that separates these two types of stressor may not always be so clear. Clinical conditions such as decompensated chronic obstructive pulmonary disease have been reported to induce TTS in several cases [19, 20]: despite being usually considered a physical trigger, this disease also brings fear and anxiety to patients, who during every attack feel they may choke to death. A similar reasoning could be made for other conditions such as stroke, and raises doubts about whether psychological factors should really have been regarded as a less frequent trigger of TTS than physical ones.
The Heart-Breaking Burden of Chronic Stress
Despite not being considered the first trigger of TTS in terms of frequency [11], and even though TTS is not the only cardiovascular disease that may be induced by psychological factors [21], emotional stressors have always been considered an important element in the characterization of the syndrome.However, the seemingly “acute” nature of the events leading to TTS raises an important question:since most of the modern population has to face acute stressful situations almost daily, why is this syndrome so rare?
It would seem that TTS patients may be “predisposed” toward an exaggerated sensitivity to emotional triggers. Some of the possible mechanisms underlying this phenomenon (such as anxiety,depression, poor stress coping skills and previous exposure to chronic stress) have been investigated, sometimes with discordant results [22–24].In particular, the “chronic stress” hypothesis was supported by Wallström et al. [23], who in their interviews revealed that TTS patients had experienced constant stress for years or even decades before the onset of symptoms. These chronic stressful situations were unanimously considered by the patients to be more burdensome than the event that had actually triggered the syndrome. Could it then be possible for a prolonged exposure to stressful circumstances to induce vulnerability and susceptibility toward acute psychological or physical stressors? How could this explain the epidemiology of the syndrome, given that chronic stress is also a constant part of our society? Most probably, an explanation will be found in the interaction between psychological/psychosocial factors and physical alterations, as suggested by Kastaun et al. [24], but to prove this theory more elaborate investigations should be undertaken, possibly exploiting the larger registries that have been established in recent years as a source of more consistent cohorts.
Stress and Pathophysiology of TTS
The important role of stressful triggers in the pathophysiology of TTS is suggested by the hyperadrenergic state observed in most patients with the disease. A study in 2005 showed that plasma catecholamine levels at presentation were two-fold to three-fold higher in patients with TTS than in those with Killip III myocardial infarction [25],and TTS has been repeatedly reported in association with diseases or clinical procedures that could induce a hyperadrenergic storm, such as pheochromocytoma, subarachnoid hemorrhage, or alcohol withdrawal [26–29]. An elevated concentration of serum catecholamines, caused by either these conditions or an excessive stress response to surgery or a strong emotion, could lead both to an increase in myocardial contractility (and/or increased vascular resistances) and to a direct injury of the myocardium caused by calcium overload. According to other theories, elevated levels of epinephrine may have a downregulating effect, possibly via β2-adrenergic receptor signaling, especially in the apex, where such receptors are more prevalent [30]. This provides a possible explanation for the characteristic distribution of contractile dysfunction.
Is Catecholamine Toxicity Really the Answer?
Despite the pathophysiological theory of catecholamine toxicity in TTS having been widely promoted,there are issues that need to be clarified. Y-Hassan et al. [31] found that only 3 of 33 consecutive TTS patients had markedly elevated catecholamine and/or metabolite levels, and all of them had underlying illnesses or acute complications. These findings contrast with the idea of a causal link between catecholamine toxicity and TTS, but do not exclude the possibility that catecholamines may trigger a cardiac sympathetic hyperactivation: most probably, these serum alterations are, as with estrogen,a single mechanism in the context of a much more complex, multifactorial disease.
Microvascular Dysfunction
Coronary microvascular dysfunction (CMD),an identified pathogenetic factor in ACS, is also among the long list of mechanisms associated with TTS and which may explain its greater incidence in women [32–43]. The diagnostic efficacy of the quantification of coronary flow reserve, by adenosine as a stressor, has been observed in patients with patent coronary arteries, in patients with significant stenosis, and even in those with occluded arteries but effective collateral coronary circulation[44–46]. More recently, quantification of coronary flow reserve to detect either normal coronary flow or impaired coronary circulation due to CMD and dobutamine stress as a means of disclosing myocardial viability (by differentiating it from stunning due to actual ischemia) was proposed as a diagnostic means in TTS [47, 48]. Furthermore, Elesber et al. [49] observed a diffuse CMD that correlated with the extent of myocardial injury during the acute phase of the syndrome, suggesting that CMD,possibly mediated by catecholamine overload, may be an underlying mechanism of myocardial insult and consequent stunning in TTS. Given the high prevalence of neuropsychiatric disorders observed in TTS patients and the direct connection between brain and coronary microcirculation, it remains plausible that this phenomenon represents a key for unlocking the mysteries of this syndrome [11].
An Ageless and Genetic Disorder?
Another interesting phenomenon associated with TTS is its observation in younger age groups such as newborns, children, and adolescents, which does not speak in favor of the hypothesis of atherosclerotic endothelial injury as a causal factor in this syndrome [50–54]. Further observations from case reports of TTS in siblings and relatives are hypothetically indicative of a potential genetic determinant underlying the syndrome, possibly a channelopathy similar to that of Brugada syndrome [55–58]. Although this hypothesis could explain the rarity and possibly the morphology of the disease, further research is still needed for confirmation.
Diagnostic Criteria – the Path Toward a Diagnosis of Certainty
The progression of our understanding of TTS has seen a contemporary evolution of diagnostic criteria,with some characteristics maintaining their importance and others being reinterpreted or becoming obsolete (Table 1).
The Mayo Clinic diagnostic criteria for TTS,introduced in 2004 and revised in 2008, would seem to have become somewhat outdated for various reasons [59, 60]. Firstly, the requirement of extension of regional wall motion abnormality (RWMA)beyond the territory of distribution of a single coronary artery is in contrast with the identification of the focal TTS subtype [61, 62]. Furthermore, the observation that up to 15% of TTS patients have significant coronary artery disease suggests that a more encompassing criterion, such as theabsence of culprit atherosclerotic coronary artery disease,as stated by the European Society of Cardiology
(ESC) Heart Failure Association position statement,may be more effective [1, 11, 63]. Lastly, differentiating TTS from pheochromocytoma-induced cardiomyopathy is too restrictive, for many cases of TTS in these patients have been observed [25–27].
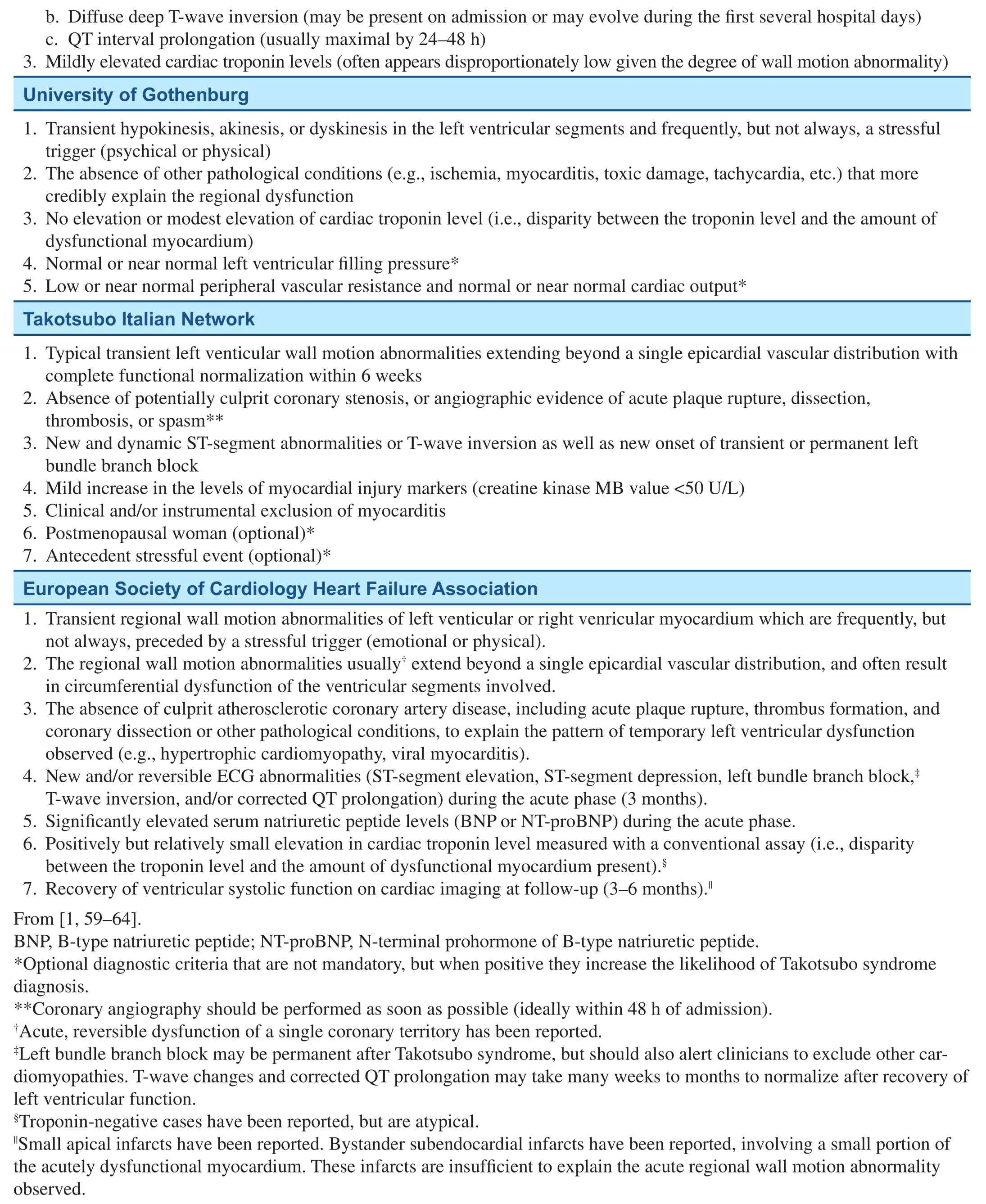
Table 1 (continued)
The 2007 Japanese Takotsubo Cardiomyopathy Group criteria defined TTS as idiopathic, distinguishing it from TTS-like cases associated with known causes [64]. In our opinion the conceptual separation between TTS and TTS-like cases does not respect the syndromic nature of the disease,considering the clinical differences are minimal.Lastly, these criteria were formulated with the assistance of a questionnaire that could possibly predispose to a criteria selection bias.
In 2012, Wittstein [65] of the Johns Hopkins University School of Medicine published criteria somewhat similar to those proposed by the Mayo Clinic, with slight differences such as the separation of helpful and mandatory factors. The inclusion of cardiac imaging evidence of restored ventricular systolic function within a predetermined time frame may be helpful in certain cases; however, signs of short-term recovery, such as ECG characteristics,serum marker levels, or radionuclide imaging findings, may be more clinically useful during the acute phase, when complications have been found to be most frequent. The Gothenburg criteria, introduced in 2011 and recently revised, have brought some interesting measurable factors into consideration,such as left ventricular filling pressure and peripheral vascular resistance and cardiac output [66].This novel attempt to introduce quantitative units of measurement is an important insight and represents the desirable direction of progression in terms of identifying more specific clinical criteria.
In 2014, the Takotsubo Italian Network proposal for diagnostic criteria was published, containing a series of intriguing novelties, alongside a number of shortcomings inherited from previous criteria [67]. Worthy of note is the attempt to quantify biomarker level elevation and the recovery period,even though, as stated before, the latter is less useful in the acute phase. Subsequent to great demand,in 2015, the ESC Heart Failure Association adapted and revised previous models to formulate the TTS diagnostic criteria, which comprise several previously defined factors but have also included a series of footnotes capable of making these criteria more encompassing [1]. For example, the ubiquitous and characteristic circumferential RWMA is required,but the existence of focal abnormalities was also recognized. On the other hand, semiquantitative criteria, such as significant elevation of serum natriuretic peptide levels and moderate increase in cardiac troponin levels, represent an important step toward the use of measurable markers for TTS diagnosis. The standard diagnostic approach to TTS is transitioning away from a diagnosis of exclusion with the identification of more TTS-“specific”characteristics, such as the circumferential nature of ventricular dysfunction and other clinical patterns.Despite these advancements, measurable diagnostic parameters and evidence of their validity are still lacking; therefore prospective comparative analyses are needed to formulate novel and verify proposed clinical scores [68].
Diagnostic Procedures
The ESC Heart Failure Association has also proposed a novel diagnostic algorithm, for the identification and differentiation of TTS patients that may help clinicians navigate through this difficult diagnosis [1]. Most TTS patients have typical ECG abnormalities, such as ST-segment elevation,T-wave inversions, and pathological Q waves [9,69]. Hypoglycemia, a known cause of TTS, is also associated with catecholamine surge and corrected QT interval prolongation, both of which are frequently present in patients with TTS [53, 70–72].Some authors have proposed a series of ECG characteristics as having a high sensitivity and specificity for TTS; however, prospective data are needed to verify their predictive capacity [68, 69].
Coronary Angiography and Left Ventriculography – Identification of Typical Morphology
Considering the profound clinical similarities between TTS and AMI, coronary angiography remains the standard invasive procedure for the exclusion of culprit coronary artery stenosis in the acute setting [63].In addition, the identification of wall motion abnormalities by left ventriculography may be of help for diagnosis. However, it should be noted that, given the limits of ventriculography in delineating the true extent of RWMAs in both the left ventricle and the right ventricle, diagnoses should be coadjuvated by echocardiography and possibly cardiac magnetic resonance imaging, given the higher diagnostic power of these two noninvasive procedures.
Echocardiography
Transthoracic echocardiography has been shown to contribute to a more frequent diagnosis of TTS given its capacity to identify left ventricular morphology and function, anatomical variants, and coronary flow reserve, as well as to detect correlated complications in the acute phase, such as left ventricular out flow tract obstruction, right ventricular involvement, apical thrombosis, mitral regurgitation, and cardiac rupture [30, 47, 48, 73].Furthermore, typical RWMAs, which correlate with the extent of myocardial insult and suggest a circumferential morphology, and wall motion score index, which has been observed to positively correlate with the extent of ST-segment elevation, have been found to differentiate AMI from TTS with a significant specificity and sensitivity [73–75].
Two-dimensional speckle tracking echocardiography has played an important role in the study of ventricular morphology and in the identification of the circumferential nature of RWMAs [75].
An interesting diagnostic alternative might be the use of stress testing with low doses of dobutamine in combination with enoximone, which has been found to be at least as efficient as full-dose dobutamine, yet safer, in ACS patients [76].
Adjunctive Imaging
Cardiac magnetic resonance imaging can be of assistance in the initial diagnosis of TTS, given its capacity to accurately assess left and right ventricular RWMAs, distinguish irreversible and reversible myocardial damage, and identify the distinct transmural, midventricular to apical pattern [77–79].These characteristics can be of assistance in differentiating TTS from AMI and myocarditis, and therefore cardiac magnetic resonance imaging should be used in synergy with coronary angiography and echocardiography.
Nuclear imaging techniques have been found not only to have a valid application in differential diagnosis between TTS and AMI but have had a substantial role in studying the pathogenetic mechanisms associated with TTS as well. Various studies have shown a typical pattern in TTS patients,referred to as “inverse flow metabolism mismatch,”characterized by a severely reduced apical myocardial uptake of glucose and by a moderately reduced myocardial perfusion [80, 81]. Additionally, TTS patients were found to have a severe denervation,measured with123I- metaiodobenzylguanidine single photon emission computed tomography [81]. Ito el al. [82] compared TTS and AMI metabolic characteristics and concluded that the transitory nature of TTS suggests similarities with myocardial stunning. However, given the high rate of false positives of single photon emission computed tomography perfusion imaging in the detection of myocardial infarction with concurrent wall motion abnormalities and reduced ventricular wall thickness, which are frequently dominant characteristics in TTS,nuclear imaging should be preceded or the nuclear imaging findings should be con firmed by cardiac magnetic resonance imaging in these patients [83,84].
Laboratory Testing – Searching for Measurable Markers
The level of serum cardiac biomarkers may assist the clinician in differentiating TTS and AMI. Said biomarkers can be present in both TTS and AMI but, given the extent of ventricular dysfunction, the elevation of their levels is considered disproportionately low in TTS [11, 59].
As previously stated, an elevation in catecholamine serum levels is thought to be one of the main driving forces in TTS [25–27]; therefore dosing catecholamine levels may facilitate the identification of dubious cases. B-type natriuretic peptide serum levels, which have the advantage of correlating with myocyte distension rather than necrosis [85], have been shown to increase in TTS to a greater extent than in AMI [86]. However, when a similar extent of wall motion abnormality is present, B-type natriuretic peptide values in AMI can resemble those seen in TTS.
Specific microRNA patterns have been widely observed in both cardiovascular and noncardiovascular diseases [87]. A comparison between the elevation and/or depression of the levels of cardiac specific microRNAs has shown TTS-specific patterns that may potentially be useful in differential diagnosis with AMI [88]. This novel diagnostic approach will, nonetheless, require further prospective data for its validation.
Prognosis: Not as Harmless as It Seemed
Left ventricular dysfunction in TTS is typically a transient phenomenon, so TTS has historically been considered harmless. However, most of the studies currently at hand show that the octopus trap is more dangerous than previously thought [89, 90]. Firstly,the rate of acute complications such as heart failure, arrhythmias, mitral regurgitation, cardiogenic shock, and cardiac rupture is rather high, although data on their incidence differ widely [8, 11, 12].Brinjikji et al. [12] reported that the prevalence of acute complications was 34.5%, and that the most frequent complication was acute coronary heart failure (31.1%), more frequent in women than in men and occasionally accompanied by respiratory insufficiency (6.7%). Others have observed independent predictors of low and high incidence of acute complications [11]. The ESC Heart Failure Association position statement introduced a promising risk stratification tool aimed at the prediction of complications in TTS patients, although additional prospective and comparative studies are needed for its validation [1].
Mortality among TTS patients is yet another element that should warn clinicians about the potential harmfulness of the syndrome. In-hospital mortality differs widely from study to study, ranging from 1%to 8%, which are rates actually similar to those of AMI patients [12, 91–97]. According to Brinjikji et al. [12], mortality tended to rise in patients with acute complications and in those with underlying critical illnesses. Moreover, although no correlation was found between death and age or ethnicity,it was observed that men had higher mortality and were likelier to have underlying critical illnesses and acute complications (except for coronary heart failure).
Elesber et al. [97] found that chest pain recurred in 31% of TTS patients at follow-up, and that the average annual recurrence rate of TTS was 2.9% in the first 4 years and 1.3% at the end of the followup. Singh et al. [91] reported similar recurrence rates (1.5%), although the percentage of patients with recurrent chest pain was lower (14%).
Therapy: From Empirical to Evidence Based
Initial therapy is usually directed toward AMI,and patients often begin treatment with aspirin,anticoagulants, beta-blockers, and possibly angiotensin-converting enzyme (ACE) inhibitors. If the presence of plaque rupture is compatible with TTS,then long-term antiplatelet therapy may be reasonably justified. Similarly, in consideration of the absence of beneficial effects and excessive bleeding risks, thrombolytic therapies should be avoided in patients with TTS [63]. Therapy with beta-blockers and ACE inhibitors or angiotensin receptor blockers may be continued or introduced in the aim of preventing or treating acute complications such as arrhythmias, severe heart failure, or left ventricular out flow tract obstruction [1, 63]. However, Templin et al. [11] observed beneficial effects on long-term survival associated with ACE inhibitor or angiotensin receptor blocker administration, but did not find the same association with beta-blocker therapy.This suggests that prospective randomized data are needed not only to verify the ideal management of the acute phase but also to identify efficient longterm prevention in TTS patients. Furthermore, the relatively high incidence of complications in TTS justifies thorough evaluation of risk and attentive monitoring to enable timely and efficient prevention and treatment. The European Heart Failure Takotsubo Task Force has recently elaborated diagnostic and therapeutic algorithms, based on expert consensus, the latter of which considers different strategies for low-risk and high-risk patients [1].
Use of sympathomimetic agents and inotropes should be avoided or discontinued, because of the possible exacerbation of cardiac damage given that at higher concentrations an excessive inhibitory G-protein stimulation is obtained [98–101]. Severe cases of heart failure and shock may be treated with mechanical support devices or with levosimendan [102] when these are not available; given the efficacy of intra-aortic balloon counterpulsation in AMI is controversial [1, 63, 103–105], its efficiency in TTS patients should be studied prospectively along with that of other mechanical support devices.
Patients with significant apical akinesis or apical RWMA should be considered for prophylactic antithrombotic therapy, which will most likely have been initiated at admission and should be continued until RWMAs have resolved [1, 63].
Limited data on prophylactic therapy for recurrences and persistent symptoms exist, and therefore randomized prospective data are needed to verify the ideal therapeutic strategies for both short-term and long-term management.
Conclusions
Many theories have been proposed to explain the pathogenetic model underlying TTS but, while some of these hypotheses seem to be more plausible than others, the complete mechanism underlying the syndrome is not fully understood. It would seem that catecholamine overdrive may be an important component in the manifestation of TTS,but this theory does not explain the relative rarity of the syndrome. Could it be that some sort of preexisting condition is necessary to “predispose” people to the development of TTS? Could it be logical to hypothesize the presence of genetic determinants,such as a congenital channelopathy or adrenergic receptor polymorphisms? Or could TTS be favored by an environmental predisposing condition, such as chronic stress, manifested as an alteration in microRNA expression?
Considering that these and many other questions regarding TTS are yet to be answered, and taking into account the presence of various conditions associated with TTS, such as CMD, neuropsychiatric disorders, and other comorbidities, evidence suggests that the pathogenic mechanisms in TTS are multifactorial and representative of the delicate balance between various intimately tied components of the human organism. It is likely that future breakthroughs in the understanding of such mechanisms will come not only from the field of cardiology but that a significant contribution will emerge from interdisciplinary studies and observations.
Despite the growing attention that TTS has attracted in recent years and the increasing number of promising research studies regarding its clinical management, prospective randomized studies have been scarce, largely related to the rarity of this syndrome, and there is lack of universally acknowledged data on aspects such as diagnostic criteria,risk stratification, and therapeutic regimens. Future resources should be invested in the production and validation of effective, evidence-based guidelines that will help clinicians in the battle against this mysterious and insidious disease and its sometimes difficult differentiation from ACS.
Funding
None.
Conflict of Interest
The authors declare no conflict of interest [106–108].
REFERENCES
1. Lyon AR, Bossone E, Schneider B,Sechtem U, Citro R, Underwood SR, et al. Current state of knowledge on takotsubo syndrome: a position statement from the Taskforce on Takotsubo Syndrome of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 2016;18:8–27.
2. Lüscher TF, Templin C. Is takotsubo syndrome a microvascular acute coronary syndrome? Towards a new definition. Eur Heart J 2016.doi:10.1093/eurheartj/ehw057.
3. Sato HTH, Uchida T, Dote K,Ishihara M. Takotsubo-like left ventricular dysfunction due to multivessel coronary spasm. In:Kodama K, Haze K, Hori M, editors. Clinical aspect of myocardial injury: from ischemia to heart failure. Tokyo: Kagakuhyoronsha Publishing; 1990. pp. 56–64 (in Japanese).
4. Dote K, Sato H, Tateishi H, Uchida T, Ishihara M. Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases. J Cardiol 1991;21:203–14.
5. Bybee KA, Prasad A, Barsness GW, Lerman A, Jaffe AS, Murphy JG, et al. Clinical characteristics and thrombolysis in myocardial infarction frame counts in women with transient left ventricular apical ballooning syndrome. Am J Cardiol 2004;94:343–6.
6. Deshmukh A, Kumar G, Pant S,Rihal C, Murugiah K, Mehta JL.Prevalence of takotsubo cardiomyopathy in the United States. Am Heart J 2012;164:66–71.e1.
7. Minhas AS, Hughey AB, Kolias TJ. Nationwide trends in reported incidence of takotsubo cardiomyopathy from 2006 to 2012. Am J Cardiol 2015;116:1128–31.
8. Khera R, Light-McGroary K, Zahr F, Horwitz PA, Girotra S. Trends in hospitalisation for takotsubo cardiomyopathy in the United States.Am Heart J 2016;172:53–63.
9. Gianni M, Dentali F, Grandi AM, Sumner G, Hiralal R, Lonn E. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J 2006;27:1523–9.
10. Hurst RT1, Prasad A, Askew JW 3rd, Sengupta PP, Tajik AJ.Takotsubo cardiomyopathy: a unique cardiomyopathy with variable ventricular morphology. JACC Cardiovasc Imaging 2010;3:641–9.
11. Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR,Jaguszewski M, et al. Clinical features and outcomes of takotsubo(stress) cardiomyopathy. N Engl J Med 2015;373:929–38.
12. Brinjikji W, El-Sayed AM, Salka S. In-hospital mortality among patients with takotsubo cardiomyopathy: a study of the National Inpatient Sample 2008 to 2009. Am Heart J. 2012;164:215–21.
13. Chou AY, Saw J. Basis for sex specific expression of takotsubo cardiomyopathy, cardiac syndrome X, and spontaneous coronary artery dissection. Can J Cardiol 2014;30:738–46.
14. Sato A, Yagihara N, Kodama M,Mitsuma W, Tachikawa H, Ito M,et al. Takotsubo cardiomyopathy after delivery in an oestrogendeficient patient. Int J Cardiol 2011;149:e78–9.
15. Brenner R, Weilenmann D, Maeder MT, Jörg L, Bluzaite I, Rickli H, et al. Clinical characteristics,sex hormones, and long-term follow-up in Swiss postmenopausal women presenting with takotsubo cardiomyopathy. Clin Cardiol 2012;35:340–7.
16. Auzel O, Mustafic H, Pillière R, El Mahmoud R, Dubourg O,Mansencal N. Incidence, characteristics, risk factors, and outcomes of takotsubo cardiomyopathy with and without ventricular arrhythmia.Am J Cardiol 2016;117:1242–7.
17. Watanabe H, Kodama M, Okura Y, Aizawa Y, Tanabe N, Chinushi M, et al. Impact of earthquakes on takotsubo cardiomyopathy. J Am Med Assoc 2005;294:305.
18. Chan C, Elliott J, Troughton R,Frampton C, Smyth D, Crozier I,et al. Acute myocardial infarction and stress cardiomyopathy following the Christchurch earthquakes.PLoS One 2013;8:e68504.
19. Peters S. Association between chronic obstructive pulmonary disease and tako tsubo cardiomyopathy – a case report. Int J Cardiol 2014;176:e101.
20. Landefeld K, Saleh Q, Sander GE. Stress cardiomyopathy in the setting of COPD exacerbation. J Investig Med High Impact Case Rep 2015;3:2324709615612847.
21. Dimsdale JE. Psychological stress and cardiovascular disease. J Am Coll Cardiol 2008;51:1237–46.
22. Scantlebury DC, Rohe DE, Best PJ, Lennon RJ, Lerman A, Prasad A. Stress-coping skills and neuroticism in apical ballooning syndrome(takotsubo/stress cardiomyopathy).Open Heart 2016;3:e000312.
23. Wallström S, Ulin K, Määttä S,Omerovic E, Ekman I. Impact of long-term stress in takotsubo syndrome: experience of patients. Eur J Cardiovasc Nurs 2016;15:522–8.
24. Kastaun S, Gerriets T, Tschernatsch M, Yeniguen M, Juenemann M.Psychosocial and psychoneuroendocrinal aspects of takotsubo syndrome.Nat Rev Cardiol 2016;13:688–94.
25. Wittstein IS, Thiemann DR, Lima JA, Baughman KL, Schulman SP,Gerstenblith G, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med 2005;352:539–48.
26. De Souza F, Altenburg Odebrecht Curi Gismondi R, Henriques Cunha Neto S, de Mattos MA. Tako-tsubolike cardiomyopathy and extraadrenal pheochromocytoma: case report and literature review. Clin Res Cardiol 2008;97:397–401.
27. Marcovitz PA, Czako P, Rosenblatt S, Billecke SS. Pheochromocytoma presenting with takotsubo syndrome.J Interv Cardiol 2010;23:437–42.
28. Talahma M, Alkhachroum AM,Alyahya M, Manjila S, Xiong W. Takotsubo cardiomyopathy in aneurysmal subarachnoid hemorrhage: institutional experience and literature review. Clin Neurol Neurosurg 2016;141:65–70.
29. Harris ZM, Alonso A, Kennedy TP.Adrenergic inhibition with dexmedetomidine to treat stress cardiomyopathy during alcohol withdrawal: a case report and literature review. Case Rep Crit Care 2016;2016:9693653.doi: 10.1155/2016/9693653.
30. Ono R, Falcão LM. Takotsubo cardiomyopathy systematic review:pathophysiologic process, clinical presentation and diagnostic approach to takotsubo cardiomyopathy. Int J Cardiol 2016;209:196–205.
31. Y-Hassan S, Henareh L. Plasma catecholamine levels in patients with takotsubo syndrome: implications for the pathogenesis of the disease.Int J Cardiol 2015;181:35–8.
32. Manfrini O, Cenko E, Verna E,Salerno Uriarte JA, Bugiardini R. Endothelial dysfunction versus early atherosclerosis: a study with high resolution imaging. Int J Cardiol 2013;168:1714–6.
33. Bugiardini R, Borghi A, Pozzati A,Ottani F, Morgagni GL, Puddu P.The paradox of nitrates in patients with angina pectoris and angiographically normal coronary arteries. Am J Cardiol 1993;72:343–7.
34. Bugiardini R, Manfrini O, Pizzi C,Fontana F, Morgagni G. Endothelial function predicts future development of coronary artery disease:a study of women with chest pain and normal coronary angiograms.Circulation 2004;109:2518–23.
35. Bugiardini R, Bairey Merz CN.Angina with “normal” coronary arteries: a changing philosophy. J Am Med Assoc 2005;293:477–84.
36. Vaccarino V, Badimon L, Corti R,de Wit C, Dorobantu M, Manfrini O, et al. Presentation, management,and outcomes of ischaemic heart disease in women. Nat Rev Cardiol 2013;10:508–18.
37. Bugiardini R, Badimon L, Collins P, Erbel R, Fox K, Hamm C, et al.Angina, “normal” coronary angiography, and vascular dysfunction:risk assessment strategies. PLoS Med 2007;4:e12.
38. Bugiardini R. Women, ‘nonspecific’ chest pain, and normal or near-normal coronary angiograms are not synonymous with favourable outcome. Eur Heart J 2006;27:1387–9.
39. Cenko E, Bugiardini R. Vasotonic angina as a cause of myocardial ischemia in women. Cardiovasc Drugs Ther 2015;29:339–45.
40. Bugiardini R. Normal coronary arteries: clinical implications and further classification. Herz 2005;30:3.
41. Warisawa T, Naganuma T,Nakamura S. Reversible microvascular dysfunction in takotsubo syndrome shown using index of microcirculatory resistance. Circ J 2016;80:750–2.
42. Pepine CJ, Anderson RD, Sharaf BL, Reis SE, Smith KM, Handberg EM, et al. Coronary microvascular reactivity to adenosine predicts adverse outcome in women evaluated for suspected ischemia results from the National Heart,Lung and Blood Institute WISE(Women’s Ischemia Syndrome Evaluation) study. J Am Coll Cardiol 2010;55:2825–32.
43. Kothawade K, Bairey Merz CN.Microvascular coronary dysfunction in women: pathophysiology,diagnosis, and management. Curr Probl Cardiol 2011;36:291–318.
44. Pizzuto F, Voci P, Mariano E,Puddu P, Spedicato P, Romeo F. Coronary flow reserve of the angiographically normal left anterior descending coronary artery in patients with remote coronary artery disease. Am J Cardiol 2004;94:577–82.
45. Pizzuto F, Voci P, Puddu PE,Chiricolo G, Borzi M, Romeo F.Functional assessment of the collateral-dependent circulation in chronic total coronary occlusion using transthoracic Doppler ultrasound and venous adenosine infusion. Am J Cardiol 2006;98:197–203.
46. Pizzuto F, Voci P, Bartolomucci F,Puddu PE, Strippoli G, Broglia L,et al. Usefulness of coronary flow reserve measured by echocardiography to improve the identification of significant left anterior descending coronary artery stenosis assessed by multi detector computed tomography. Am J Cardiol 2009;104;657–64.
47. Meimoun P, Clerc J, Vincent C,Flahaut F, Germain AL, Elmkies F, et al. Non-invasive detection of tako-tsubo cardiomyopathy vs.acute anterior myocardial infarction by transthoracic Doppler echocardiography. Eur Heart J Cardiovasc Imaging 2012;14:464–70.
48. Collste O, Tornvall P, Alam M,Frick M. Coronary flow reserve during dobutamine stress in takotsubo stress cardiomyopathy. BMJ Open 2015;5:e007671.
49. Elesber A, Lerman A, Bybee KA,Murphy JG, Barsness G, Singh M,et al. Myocardial perfusion in apical ballooning syndrome correlate of myocardial injury. Am Heart J 2006;152:469.e9–13.
50. Greco CA, De Rito V, Petracca M,Garzya M, Donateo M, Magliari F. Takotsubo syndrome in a newborn. J Am Soc Echocardiogr 2011;24:471.e5–7.
51. Dessardo S, TomuliV, Dessardo NS. Tako-tsubo syndrome in a 12-year-old girl: exhausted heart,not broken heart. Pediatr Cardiol 2011;32:1008–11.
52. Krpata DM, Barksdale EM Jr.Trauma induced left ventricular apical ballooning syndrome in a 15 year old: a rare case of tako-tsubo cardiomyopathy J Pediatr Surg 2013;48:876–9.
53. Ohwada R, Hotta M, Kimura H,Takagi S, Matsuda N, Nomura K,et al. Ampulla cardiomyopathy after hypoglycemia in three young female patients with anorexia nervosa. Intern Med 2005;44:228–33.
54. Biteker M, Duran NE, Civan HA,Gündüz S, Gökdeniz T, Kaya H,et al. Broken heart syndrome in a 17-year-old girl. Eur J Pediatr 2009;168:1273–5.
55. Ikutomi M, Yamasaki M, Matsusita M, Watari Y, Arashi H, Endo G, et al. Takotsubo cardiomyopathy in siblings. Heart Vessels 2014;29:119–22.
56. Musumeci B, Saponaro A, Pagannone E, Proietti G, Mastromarino V, Conti E, et al. Simultaneous takotsubo syndrome in two sisters. Int J Cardiol 2013;165:e49–50.
57. Kumar G, Holmes DR Jr, Prasad A.“Familial” apical ballooning syndrome (takotsubo cardiomyopathy).Int J Cardiol 2010;144: 444–5.
58. Brugada R, Brugada J, Antzelevitch C, Kirsch GE, Potenza D, Towbin JA, et al. Sodium channel blockers identify risk for sudden death in patients with ST-segment elevation and right bundle branch block but structurally normal hearts.Circulation 2000;101:510–5.
59. Bybee K, Kara T, Prasad A, Lerman A, Barsness GW, Wright RS, et al.Systematic review: transient left ventricular apical ballooning: a syndrome that mimics ST-Segment elevation myocardial infarction.Ann Intern Med 2004;141:858–65.
60. Prasad A, Lerman A, Rihal C.Apical ballooning syndrome (takotsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J 2008;155:408–17.
61. Demirelli S, Ermis E, Hatem E,Uslu A, Askin L. Focal mid-ventricular anterior ballooning: an unusual pattern of takotsubo cardiomyopathy. Intractable Rare Dis Res 2015;4:108–10.
62. Kato K, Kitahara H, Fujimoto Y,Sakai Y, Ishibashi I, Himi T, et al.Prevalence and clinical features of focal takotsubo cardiomyopathy.Circ J 2016;80:1824–9.
63. Kurisu S, Kihara Y. Clinical management of takotsubo cardiomyopathy. Circ J 2014;78:1559–66.
64. Kawai S, Kitabatake A, Tomoike H, Takotsubo Cardiomyopathy Group. Guidelines for diagnosis of takotsubo (ampulla) cardiomyopathy. Circ J 2007;71:990–2.
65. Wittstein I. Stress cardiomyopathy:a syndrome of catecholamine-mediated myocardial stunning? Cell Mol Neurobiol 2012;32:847–57.
66. Omerovic E, Redfors B, Shao Y.Stress-induced cardiomyopathy(takotsubo) – broken heart and mind? Vasc Health Risk Manag 2013;9:149–54.
67. Parodi G, Citro R, Bellandi B,Provenza G, Marrani M, Bossone E.Revised clinical diagnostic criteria for tako-tsubo syndrome: the Takotsubo Italian Network proposal. Int J Cardiol 2014;172:282–3.
68. Dias A, Franco E, Janzer S,Koshkelashvili N, Bhalla V,Pressman GS, et al. Performance of a novel clinic score in differentiating takotsubo cardiomyopathy from ST elevation myocardial infarction within the first 24h. Int J Cardiol 2016;203:12–4.
69. Ogura R, Hiasa Y, Takahashi T,Yamaguchi K, Fujiwara K, Ohara Y, et al. Specific findings of the standard 12-lead ECG in patients with ‘takotsubo’ cardiomyopathy:comparison with the findings of acute anterior myocardial infarction. Circ J 2003;67:687–90.
70. Ansari MJ, Prasad A, Pellikka PA,Klarich KW. Takotsubo cardiomyopathy caused by hypoglycemia: a unique association with coronary arterial calcification. Int J Cardiol 2011;147:e21–3.
71. Nordin C. The case for hypoglycaemia as a proarrhythmic event: basic and clinical evidence. Diabetologia 2010;53:1552–61.
72. Madias C, Fitzgibbons TP,Alsheikh-Ali AA, Bouchard JL,Kalsmith B, Garlitski AC, et al.Acquired long QT syndrome from stress cardiomyopathy is associated with ventricular arrhythmias and torsades de pointes. Heart Rhythm 2011;8:555–61.
73. Citro R, Rigo F, Ciampi Q, D’andrea A, Provenza G, Mirra M, et al.Echocardiographic assessment of regional left ventricular wall motion abnormalities in patientis with takotsubo cardiomyopathy: a comparison with anterior left infarction. Eur J Echocardiogr 2011;12:542–9.
74. Bossone E, Lyon A, Citro R,Athanasiadis A, Meimoun P, Parodi G, et al. Takotsubo cardiomyopathy: an integrated multi-imaging approach. Eur J Echocardiogr 2001;12:542–9.
75. Mansencal N, Abbou N, Pillière R,El Mahmoud R, Farcot J, Dubourg O. Usefulness of two-dimensional speckle tracking echocardiography for assessment of tako-tsubo cardiomyopathy. Am J Cardiol 2009;103:1020–4.
76. Mangieri E, Alessandri N, Tanzilli G, Barillà F, Puddu PE, Monti F,et al. Enoximone coupled to very low dose dobutamine echocardiography detects myocardial viability in akinetic and dyskinetic postmyocardial infarcted areas. Am J Cardiol 1999;84:264–69.
77. Eitel I, Von Knobelsdorff-Brenkenhoff F, Bernhardt P, Carbone I, Muellerleile K, Aldrovandi A,et al. Clinical characteristics and cardiovascular magnetic resonance findings in stress (takotsubo) cardiomyopathy. J Am Med Assoc 2011;306:277–86.
78. Weinsaft JW, Kim HW, Crowley AL, Klem I, Shenoy C, Van Assche L, et al. LV Thrombus detection by routine echocardiography: insights into performance characteristics using delayed enhancement CMR. JACC Cardiovasc Imaging 2011;4:702–12.
79. Joshi SB, Chao T, Herzka DA,Zeman PR, Cooper HA, Lindsay J, et al. Cardiovascular magnetic resonance T2 signal abnormalities in left ventricular ballooning syndrome. Int J Cardiovasc Imaging 2010;26:227–32.
80. Yoshida T, Hibino T, Kako N,Murai S, Oguri M, Kato K, et al.A pathophysiologic study of takotsubo cardiomyopathy with F-18 fluorodeoxyglucose positron emission tomography. Eur Heart J 2007;28:2598–604.
81. Testa M, Feola M. Usefulness of myocardial positron emission tomography/nuclear imaging in takotsubo cardiomyopathy. World J Radiol 2014;6:502–6.
82. Ito K, Sugihara H, Kinoshita N, Azuma A, Matsubara H.Assessment of takotsubo cardiomyopathy (transient left ventricular apical ballooning) using99mTctetrofosmin,123I-BMIPP,123I-MIBG and99mTc-PYP myocardial SPECT.Ann Nucl Med 2005;19:435–45.
83. Eisner RL, Schmarkey LS, Martin SE, Carey D, Worthy MA, Chu TH, et al. Defects on SPECT “perfusion” images can occur due to abnormal segmental contraction. J Nucl Med 1994;35:638–43.
84. Mahrholdt H, Zhydkov A, Hager S, Meinhardt G, Vogelsberg H,Wagner A, et al. Left ventricular wall motion abnormalities as well as reduced wall thickness can cause false positive results of routine SPECT perfusion imaging for detection of myocardial infarction.Eur Heart J 2005;26:2127–35.
85. Mukoyama M, Nakao K, Saito Y,Ogawa Y, Hosoda K, Suga S, et al.Increased human brain natriuretic peptide in congestive heart failure.N Engl J Med 1990;323:757–8.
86. Randhawa MS, Dhillon AS, Taylor HC, Sun Z, Desai MY. Diagnostic utility of cardiac biomarkers in discriminating takotsubo cardiomyopathy from acute myocardial infarction. J Card Fail 2014;20:2–8.
87. Gupta SK, Bang C, Thum T.Circulating microRNAs as biomarkers and potential paracrine mediators of cardiovascular disease. Circ Cardiovasc Genet 2010;3:484–8.
88. Jaguszewski M, Osipova J, Ghadri J, Napp L, Widera C, Franke J,et al. A signature of circulating microRNAs differentiates takotsubo cardiomyopathy from acute myocardial infarction. Eur Heart J 2013;35:999–1006.
89. Liang JJ, Cha YM, Oh JK, Prasad A. Sudden cardiac death: an increasingly recognized presentation of apical ballooning syndrome(takotsubo cardiomyopathy). Heart Lung 2013;42:270–2.
90. Freitas HF, Renault R, Ribeiro ES,Andrade FM, Brito FS Jr, Velloso LG. Sudden cardiac arrest due to puerperal transient left ventricular apical ballooning syndrome. Int J Cardiol 2011;149:e12–13.
91. Singh K, Carson K, Usmani Z,Sawhney G, Shah R, Horowitz J. Systematic review and metaanalisis of incidence and correlates of recurrence of takotsubo cardiomyopathy. Int J Cardiol 2014;174:696–701.
92. Schneider B, Athanasiadis A, Schwab J, Pistner W, Von Scheidt W, Gottwald U, et al. Clinical spectrum of takotsubo cardiomyopathy in Germany:results of the tako-tsubo registry of the Arbeitsgemeinschaft Leitende Kardiologische Krankenhausärzte(ALKK) Dtsch Med Wochenschr 2010;135:1908–13.
93. Akashi YJ, Musha H, Kida K, Itoh K, Inoue K, Kawasaki K, et al.Reversible ventricular dysfunction takotsubo cardiomyopathy. Eur J Heart Fail 2005;7:1171–6.
94. Kurisu S, Sato H, Kawagoe T,Ishihara M, Shimatani Y, Nishioka K, et al. Tako-tsubo-like left ventricular dysfunction with ST-segment elevation: a novel cardiac syndrome mimicking acute myocardial infarction. Am Heart J 2002;143:448–55.
95. Murugiah K, Wang Y, Desai NR,Spatz ES, Nuti SV, Dreyer RP,et al. Trends in short- and longterm outcomes for takotsubo cardiomyopathy among Medicare fee-for-service bene ficiaries, 2007 to 2012. JACC Heart Fail 2016;4:197–205.
96. Redfors B, Vedad R, Angerås O, Råmunddal T, Petursson P,Haraldsson I, et al. Mortality in takotsubo syndrome is similar to mortality in myocardial infarction – a report from the SWEDEHEART registry.Int J Cardiol 2015;185:282–9.
97. Elesber AA, Prasad A, Lennon RJ, Wright RS, Lerman A, Rihal CS. Four-year recurrence rate and prognosis of the apical ballooning syndrome. J Am Coll Cardiol 2007;50:448–52.
98. Redmond M, Knapp C, Salim M,Shanbhag S, Jaumdally R. Use of vasopressors in takotsubo cardiomyopathy: a cautionary tale. Br J Anaesth 2013;110:487–8.
99. Rathakrishnan R, Lee YP. The use of vasopressors in takotsubo cardiomyopathy: impact on neurological practice. Int J Cardiol 2010;145:131.
100. Abe Y, Tamura A, Kadota J.Prolonged cardiogenic shock caused by a high-dose intravenous administration of dopamine in a patient with takotsubo cardiomyopathy. Int J Cardiol 2010;141:e1–3.
101. Paur H, Wright PT, Sikkel MB,Tranter MH, Mans field C, O’Gara P, et al. High levels of circulating epinephrine trigger apical cardiodepression in a β2-adrenergic receptor/Gi-dependent manner: a new model of takotsubo cardiomyopathy. Circulation 2012;126:697–706.
102. Usta C, Puddu PE, Papalia U, De Santis V, Vitale D, Tritapepe L,et al. Comparison of the inotropic effects of levosimendan, rolipram,and dobutamine on human atrial trabeculae. J Cardiovasc Pharmacol 2004;44:622–25.
103. Thiele H, Zeymer U, Neumann FJ,Ferenc M, Olbrich HG, Hausleiter J, et al. Intraaortic balloon support for myocardial infarction with cardiogenic shock. N Engl J Med 2012;367:1287–96.
104. Thiele H, Zeymer U, Neumann FJ,Ferenc M, Olbrich HG, Hausleiter J, et al. Intra-aortic balloon counterpulsation in acute myocardial infarction complicated by cardiogenic shock (IABP-SHOCK II):final 12 month results of a randomised, open-label trial. Lancet 2013;382:1638–45.
105. Schiariti M, Saladini P, Cuturello D, Iannetta L, Torromeo C, Puddu PE. Decline in platelet count and long-term post-PCI ischemic events: implication of the intraaortic balloon pump. Vasc Pharm 2014;60:25–31.
106. Shewan LG, Coats AJ. Adherence to ethical standards in publishing scientific articles: a statement from the International Journal of Cardiology. Int J Cardiol 2012;161:124–5.
107. Alfonso F, Timmis A, Pinto FJ,Ambrosio G, Ector H, Kulakowski P, et al. Conflict of interest policies and disclosure requirements among European Society of Cardiology national cardiovascular journals.Eur Heart J 2012;33:587–94.
108. ESC Board. Relations between professional medical associations and the health-care industry, concerning scientific communication and continuing medical education: a policy statement from the European Society of Cardiology.Eur Heart J 2012;33:666–74.
 Cardiovascular Innovations and Applications2017年2期
Cardiovascular Innovations and Applications2017年2期
- Cardiovascular Innovations and Applications的其它文章
- Telemedicine: Its Importance in Cardiology Practice. Experience in Chile
- Digoxin and Heart Failure: Are We Clear Yet?
- Role of Cholesterol Crystals During Acute Myocardial Infarction and Cerebrovascular Accident
- Evaluation of Multidisciplinary Collaborative Care in Patients with Acute Coronary Syndrome and Depression and/or Anxiety Disorders
- Chronic Kidney Disease is a New Target of Cardiac Rehabilitation
- Occlusive Spasm of the Left Anterior Descending Artery and First Diagonal Branch After Implantation of Everolimus Eluting Stents Without Re-stenosis in a Female Patient with Resting Angina
