Potential impact of early physiotherapy in the emergency department for non-traumatic neck and back pain
Pothiawala Sohil, Pua Yong Hao, Leong Mark
1Department of Emergency Medicine, Singapore General Hospital, Singapore
2Department of Physiotherapy, Singapore General Hospital, Singapore
Potential impact of early physiotherapy in the emergency department for non-traumatic neck and back pain
Pothiawala Sohil1, Pua Yong Hao2, Leong Mark1
1Department of Emergency Medicine, Singapore General Hospital, Singapore
2Department of Physiotherapy, Singapore General Hospital, Singapore
BACKGROUND: Musculoskeletal complaints, especially non-traumatic neck and back pain, are routinely encountered in the emergency department (ED) and lead to ED overcrowding, a burgeoning wait time for physiotherapy and outpatient orthopedic reviews. The study aimed to evaluate the impact of early physiotherapy evaluation and treatment (EPET) vs. standard care (SC) on clinical outcomes for patients presenting to the ED with non-traumatic neck and back pain.
METHODS: A retrospective observational study of 125 patients who presented to the ED with non-traumatic neck and back pain with/without peripheral symptoms from July 2010 to February 2011. Neck Disability Index (NDI), Modif i ed Oswestry Low Back Pain Disability Questionnaire (MODI) and 11-point Numeric Pain Rating Scale were used as outcome measures and compared between groups at a mean of 34 days from their initial ED visit.
RESULTS: We identif i ed a total of 125 patients. EPET group comprised 62 patients (mean age, 45 years; men, 63%) and SC group comprised 63 patients (mean age, 45 years; men, 43%). The EPET and SC groups received physiotherapy at a median of 4 and 34 days respectively from their fi rst ED visit. EPET patients had signif i cantly lower levels of disability (9.0% vs. 33.4%, Welch t-test, P<0.001) and pain (median value, 1 vs. 4 points, Mann-Whitney U-test, P<0.001) compared with SC patients.
CONCLUSION: Early access to physiotherapy in ED was associated with reduced pain and disability levels. EPET protocol can potentially decrease the demand on outpatient orthopedic services, thereby freeing up available resources to treat patients who are more likely to benef i t from it.
Physiotherapy; Emergency department; Non-traumatic neck and back pain
INTRODUCTION
Singapore General Hospital (SGH) is a tertiary hospital and a national referral center in Singapore. The emergency department (ED) sees about 145 000 patients annually. The resources available in the ED are fi nite; and hence there is a need to prioritize patients on arrival to receive emergency medical care. Acuity of the presenting condition based on a combination of initial complaints and provisional diagnosis forms the basis for such prioritization.
Musculoskeletal complaints, especially nontraumatic neck and back pain, form an important part of the wide spectrum of conditions that EDs are required to screen and treat. The non-urgent patient population with such musculoskeletal complaints attending ED and orthopedic outpatients for care creates a burgeoning wait list; which stretches the available fi nite ED resources.
Traditionally, patients presenting with nontraumatic neck and back after being assessed by the ED staff, would be treated medically for their condition and discharged. Some may require admission to the emergency observation ward. Insufficient beds toaccommodate the increasing demand results in an access block causing a backlog of patients using ED resources. After treatment and observation, patients who are fi t for discharge may be referred to outpatient orthopedic clinics for continuation of care. Very often, the orthopedic service will refer patients who are still symptomatic despite rest and medications to the physiotherapist for physical therapy. This may take a few days to weeks for patients from their initial ED visit to reach for physiotherapy.
Early physiotherapy has been tried in many healthcare systems across the world. There has not been any study of this problem locally evaluating its benef i t. Understanding the problem in our local context and its impact on the patient and the ED will help in devising strategies for better managing this group of patients.
The objective of this study is to evaluate the impact of early physiotherapy evaluation and treatment on the clinical outcomes of pain and disability levels for patients presenting to the ED at SGH with non-traumatic neck and back pain as compared to the standard care (SC) group.
METHODS
Study design
Doctors at the ED were presented with the idea of early physiotherapy evaluation and treatment (EPET) in April 2010 and the potential impact it may have on patient care and service delivery. After a series of discussions amongst the ED and physiotherapy department staff on referral criteria, service availability guidelines were framed to determine the cases most likely to benef i t from EPET.
This pilot project was introduced in July 2010 for patients presenting with non-traumatic neck and back pain with/without peripheral symptoms to the ED of SGH. These patients were screened and treated by the ED doctors and on the basis of the guidelines set and at the discretion of the consulting ED doctor, referred to a physiotherapist within the ED for further management of their musculoskeletal problem. On discharge from the ED, the patients in both groups were given analgesia as well as appropriate advice. Also, the patients from the EPET group as well as the SC group received standard physiotherapy intervention at the outpatient physiotherapy department in the subsequent weeks. The frequency and number of sessions with a physiotherapist depended on patient's progress and response.
This study was a retrospective observational review of the data of the pilot project. The data collected as part of the clinical pathways was used. Patients' attendances were retrieved for an 8-month period from 1 July 2010 to 28 February 2011. The data was obtained from the ED electronic medical records and the patients' medical records in SGH orthopedic and physiotherapy outpatient clinics at Singapore General Hospital. A data mining approach using eHints was done in collaboration with SGH Management Information. Data collection during the patient's referral to the physiotherapy department in ED or as an outpatient after discharge from the ED was done by the physiotherapists (IV and PYH). The data analysis was performed by SP, IV, PYH and ML.
Study population
Patients who were referred for early physiotherapy as part of the clinical pathway during that period formed the EPET group. The patients who were not referred for early physiotherapy and were referred to orthopedic outpatient clinic from the ED as the current practice then formed the SC group (Figure 1).
Inclusion criteria
The inclusion criteria were: (1) age>21 years; (2) patients who presented to the ED with non-traumatic neck and back pain with/without peripheral referred symptoms within the study period from 1 July 2010 to 28 February 2011; (3) patients who were referred for early physiotherapy as part of the clinical pathway during that period will form the EPET group; (4) patients who were not referred for early physiotherapy and were referred to orthopedics as the current practice then will form the SC group.
Exclusion criteria
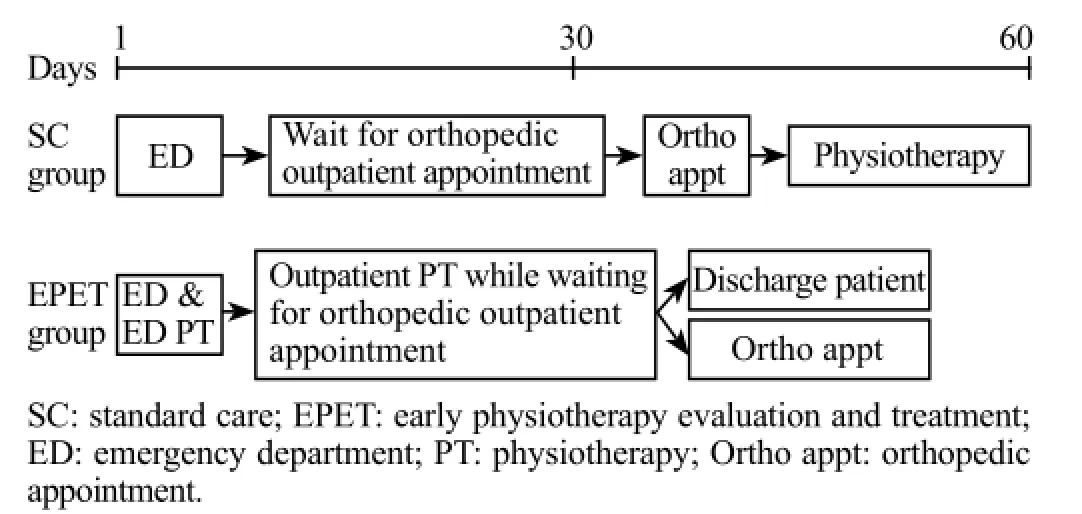
Figure 1. Timeline diagram showing patient fl ow pathway for patients with non-traumatic neck and back pain.
The exclusion criteria included: (1) age<21 years; (2) patients who were admitted during the study period; (3) patients with back and neck pain secondary to trauma;(4) patients who were not given or those who voluntarily refused physiotherapy or orthopedic outpatient appointments; (5) patients who absconded from the ED; (6) patients who defaulted follow-up.
Outcome measurements
The primary outcomes measured were pain intensity and disability level at the first visit in the ED for EPET group and subsequent outpatient physiotherapy in both EPET and SC groups.
Neck Disability Index (NDI), Modified Oswestry Low Back Pain Disability Questionnaire (MODI) and an 11-point Numeric Pain Rating Scale were used by the physiotherapists to collect data on pain and disability levels of the patients as a part of the clinical pathway.
The Neck Disability Index and the Modif i ed Oswestry Low Back Pain Questionnaire were used as measure of disability for neck and back pain respectively. These questionnaires are self-assessment tools which give the therapist information on how much has the neck or back pains affected the patient's ability to manage everyday life and are shown to have good reliability and validity. The numeric pain rating scale was used to monitor pain intensity. It is an 11-point scale ranging from 0 (no pain) to 10 (severe pain) and has been shown to have good reliability.
Data collection
The following variables were collected for the data analysis and interpretation from the electronic medical records (EMR): patient's demographic information, including age, gender, race; day of the visit, weekday vs. weekend; mode of arrival to ED; chief complaint on the day of the visit (acute/chronic); medical history, including past and psychiatric history; social history including family situation; primary and secondary diagnosis in DEM; emergency or non-emergency visit e.g. triage category; outpatient visit details either at the orthopedic or the physiotherapy outpatient clinics during subsequent visits; disability level (Neck Disability Index & Modified Oswestry Low Back Pain Disability Questionnaire) and an 11-point Numeric Pain Rating Scale of the patients at the first visit in ED and subsequent outpatient visits; primary provider in ED.
Statistical analysis
Data entry was carried out using Microsoft Excel 2003 (Microsoft Corporation). All data analyses were performed using SPSS version 14.0 (SPSS Inc., Chicago, IL, USA). Statistically significant differences were assessed using the Welch t-test for measuring the disability level and Mann-Whitney U-test for measuring the pain level. A P-value of ≤ 0.05 was considered as statistically signif i cant. A separate biomedical statistician who was not involved in the clinical practice performed all the statistical analyses.
Ethical considerations
The study was approved by the Singhealth Centralized Institutional Review Board (CIRB Ref: 2013/292/C). This study did not require the informed consent of individual patients for the analysis as it is a retrospective observational study. Hence, waiver of informed consent was obtained. The collection of data posed no risk to study participants. All patients' identif i ers were removed from the dataset to safeguard the patients' privacy and conf i dentiality.
RESULTS
We identif i ed a total of 125 patients during the study period who were treated under the EPET or SC pathways for neck and back pain. There were 62 patients in the EPET group, with the mean patient age of 45 years, and 63% of the patients in this group were males. There were 63 patients in the SC group, with the mean patient age being 45 years, and 43% of these patients were males.
EPET group had their physiotherapy sessions commence as early as the same day as their initial ED visit (mean 4 days±4). The SC group on discharge from ED had to await an orthopedic review following which they were referred for outpatient physiotherapy. This traditional pathway resulted in a mean delay of 34±22 days before they could see the physiotherapist for their first session. In this mean delay of 34 days, patients in the EPET group had at least 4 sessions of physiotherapy. All patients completed self-assessment questionnaires for disability and graded their pain on every session.
The two primary outcome measures, one the pain scale and the other, the disability level were collected for patients from both the EPET and SC groups. Outcome measures were compared between the two groups at a mean of 34 days from their initial ED visit. EPET patients had significantly lower levels of disability (9.0%) as compared to patients in the SC group (33.4%). This demonstrates a statistically significant difference in disability levels between the two groups (P<0.001) (Figure 2). Moreover, the median value of pain in EPET was 1 as compared to 4 points in the SC group, which isstatistically signif i cant (P<0.001) (Figure 3).
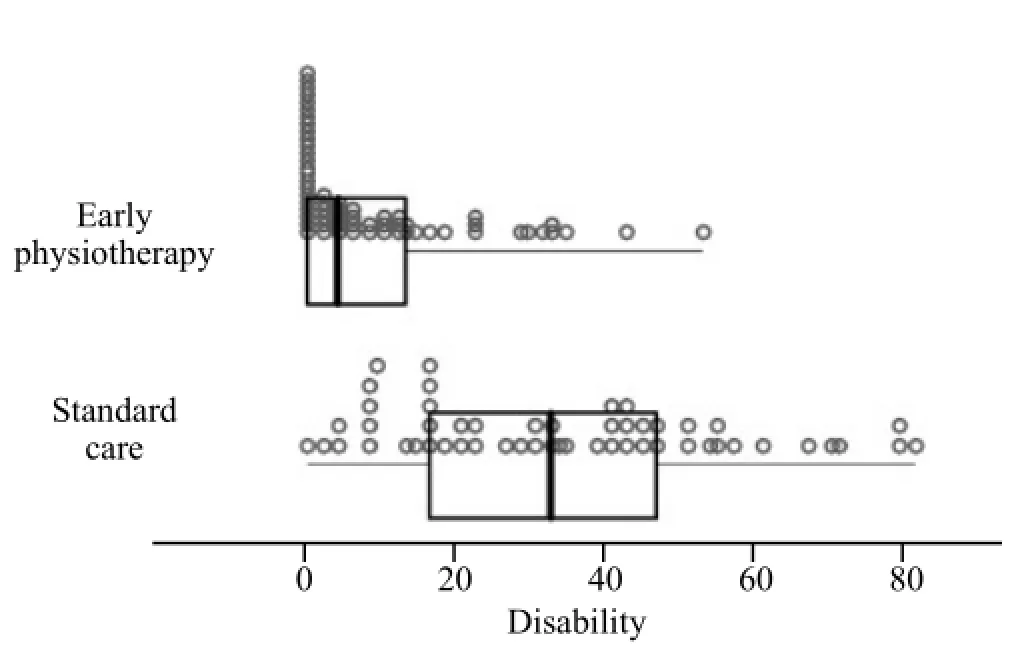
Figure 2. Box plot diagram showing comparison of disability level in the EPET (9%) vs. SC (33.4%) groups.
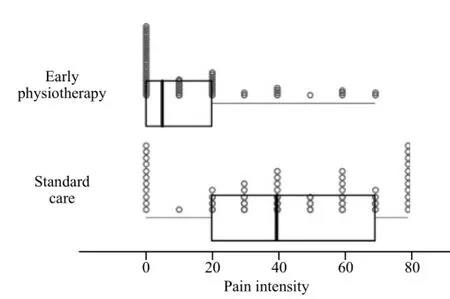
Figure 3. Box plot diagram showing comparison of pain intensity in the EPET (1 point) vs. SC (4 points) groups.
DISCUSSIONS
Research has indicated that there is an increasing ED attendance worldwide, due to the convenience of receiving immediate medical care for the less urgent medical conditions. Moreover, a shortage of elderly-care facilities and changes in family demographics have resulted in more elderly people living alone with limited social support.[1]The various factors leading to access block has resulted in ED overcrowding, increased waiting times and decreased quality of care. This has been suggested to increase the likelihood of adverse events.[2]
Musculoskeletal complaints, especially non-traumatic neck and back pain, form an important part of the wide spectrum of conditions that emergency physicians are required to screen and treat. Physiotherapists have a specialized knowledge and appropriate skill-set to treat patients with these musculoskeletal complaints.[3]Therefore, the addition of the physiotherapists as a part of the ED team has the potential for freeing up emergency physicians to attend to other cases and hence potentially reduce the waiting times for patients.[4]Moreover, the additional reasons for the development of an ED physiotherapy service include the need for mobility and exercise experts in the ED; and some evidence suggesting early physiotherapy intervention facilitates healing and prevents secondary complications.[3]
A general understanding of this service was to have a physiotherapist attend to the appropriate patients in the ED for physiotherapy-specific management with a view of alleviating patient's pain and disability; and the potential impact it may have on patient care and service delivery. EPET empowers the ED staff to screen and directly refer patients for physiotherapy services. Patients in the EPET pathway get access to physiotherapy services as early as on the same day of their ED visit for their musculoskeletal ailments (Figure 1).
Anaf and Sheppard[5]reported that physiotherapy based within the ED would be valuable in targeting interventions to assist with pain, decreased mobility as well help to reduce the number of hospital admissions through appropriate inter-disciplinary liaison. The perceived quality of care is likely to be improved with the utilization of a specif i cally trained physiotherapist in the ED.[6]It also has the potential of saving medical time for both ED doctors as well as the trauma clinic, as well as reduces referrals to the other review clinics.[6,7]
Physiotherapist assessment in the ED was associated with a statistically significant improvement in patient satisfaction.[8,9]Rapid access to physiotherapy in the ED has also shown to have a signif i cant impact on recovery time after acute knee injuries.[10]Also, patients with such direct access had fewer prescriptions for analgesia as compared to those without direct access.[11]
Having a physiotherapist in the ED resulted in an increased number of patients treated with physiotherapy, and decreased waiting times. It also resulted in more patients attending their initial appointments.[12]A study by Taylor et al[13]also suggests that it can result in decreased waiting times and length of stay for patients without any adverse effects.[14]They enhance the ability of EDs to meet the waiting time targets and are popular with patients in view of improved satisfaction levels.
A systematic review suggested that there was insufficient evidence yet to support the benefits of ED physiotherapy at system and provider levels, but there was high-level evidence of its benefits in terms of improved pain management and disability levels.[15]Also, introducing this service could potentially lead to increased health delivery costs.[8]
However, despite all this research till date, the evidence for the effectiveness and benefits of using physiotherapy services at EDs is debated. The variability in the role of physiotherapists, timing of service provision and also the different models of healthcare delivery systems across the studies makes generalization diff i cult.[16]
This paved the way for us to perform a retrospective observational review of the pilot project to determine the impact of EPET vs. SC on patient outcomes and the ability to increase resource availability. We aimed to compare the outcome measures of the SC group on their first physiotherapy visit which was at a mean of 34 days from their initial ED visit; to the 34th day mean value of the disability and pain intensity in the EPET group. By doing this we aimed to look at the impact early physiotherapy management and progression of care would have on patient's disability and pain.
EPET patients had significantly lower levels of disability as compared to patients in the SC group (9.0% vs. 33.4%). Also, the median value of pain was lower in the EPET group as compared to the SC group (1 vs. 4 points). Thus, early physiotherapy in the ED for patients presenting with non-traumatic neck and back pain with/ without peripheral symptoms was associated with reduced pain and disability, which in turn resulted in overall improved patient satisfaction.
The results of our study supports the conclusions of previous studies by Lau et al[16]and Zigenfus et al[17]that demonstrated a strong indication for early physiotherapy management of patients with acute low back pain resulting in reduced pain and improved patient satisfaction.
Thus, EPET involves a new way of ED staff working in multidisciplinary cohorts to manage patients, rather than replacing traditional existing ED services. It would aim at providing quality care to every patient through comprehensive integrated clinical practice, with the knowledge of experienced musculoskeletal physiotherapist providing positive clinical benefits to patients. It would also potentially facilitate appropriate care to a group of patients who would otherwise default their outpatient appointments.
As this is a new development in the role of the physiotherapist and its extended scope of ED practice, the benef i ts of this pilot study would provide a basis for interventional trials to further assess its effectiveness not only at the patient level, but also at a systems level.
Limitations
The limitations of this pilot study are its limit to a single emergency department. As this is a retrospective study, we did not stipulate at which exact days post-ED visit, the outcomes were measured in both groups. Also, the nature of the study allowed the fi rst contact of patients in the SC group with the physiotherapists only at a median of the 34th day from their initial ED visit. Hence, no baseline data on the pain and disability levels could be collected for this group of patients till then.
Further research in this direction would aim to develop a randomized control trial evaluating this effectiveness, as well as to design a study to evaluate its cost-effectiveness and to measure the reduction of workload on the ED and orthopedic services.
CONCLUSIONS
Early physiotherapy for patients presenting to the ED for non-traumatic neck and back pain with/without peripheral symptoms was associated with reduced pain and disability, as compared to patients with outpatient physiotherapy referral. This would result in overall improved patient satisfaction. EPET protocol can potentially decrease demand on outpatient orthopedic services, thereby freeing up available resources to treat patients who are most likely to benefit from it. Understanding the impact of early physiotherapy management on the patient and the ED will help in devising strategies for better managing this group of patients, the appropriate allocation of resources and reducing the access blocks to the ED and outpatient orthopedic teams.
ACKNOWLEDGEMENT
Thanks to Imran Virani who was a Physiotherapist at Singapore General Hospital for his contribution to the study.
Funding: None.
Ethical approval: The Centralized Institutional Review Board (CIRB) of Singhealth has provided ethical approval and ethics protocol reference number is 2013/292/C.
Conflicts of interest: The authors declare there is no competing interest related to the study, authors, other individuals or organizations.
Contributors: Sohil P proposed the study and wrote the fi rst draft. All authors read and approved the fi nal version of the paper.
REFERENCES
1 Cameron PA, Campbell DA. Access block: problems and progress. Med J Aust. 2003;178(3):99–100.
2 Forero R, Hillman K. Access block and overcrowding: a literature review. Prepared for the Australasian College for Emergency Medicine. Sydney: University of New South Wales, 2008.
3 Lebec MT, Jogodka CE. The physical therapist as a musculoskeletal specialist in the emergency department. J Orthop Sports Phys Ther. 2009;39(3):221–9.
4 Nall C. Primary care physiotherapy in the emergency department. Aust J Physiother. 2009;55(1):70.
5 Anaf S, Sheppard LA. Describing physiotherapy interventions in an emergency department setting: an observational pilot study. Accid Emerg Nurs. 2007;15(1):34–9.
6 Jibuike O, Paul-Taylor G, Maulvi S, Richmond P, Fairclough J. Management of soft tissue knee injuries in an accident and emergency department: the effect of the introduction of a physiotherapy practitioner. Emerg Med J. 2003;20(1):37–9.
7 Daker-White G, Carr AJ, Harvey I, Woolhead G, Bannister G, Nelson I, et al. A randomised controlled trial. Shifting boundaries of doctors and physiotherapists in orthopaedic outpatient departments. J Epidemiol Community Health. 1999;53(10):643–50.
8 Richardson B, Shepstone L, Poland F, Mugford M, Finlayson B, Clemence N. Randomized controlled trial and cost consequences study comparing initial physiotherapy assessment and management with routine medical practice for selectede patients in an accident and emergency department of an acute hospital. Emerg Med J. 2005;22(2):87–92.
9 McCleann C, Greenwood R, Benger J. Effect of an extended scope physiotherapy service on patient satisfaction and the outcome of soft tissue injuries in an adult emergency department. Emerg Med J. 2006;23(5):384–7.
10 Darwent M, Gamon A, McLoughlin F. Early physiotherapy within the accident and emergency department. Physiotherapy 1998; 83:281
11 Hackett GI, Bundred P, Hutton JL, O'Brien J, Stanley IM. Management of joint and soft tissue injuries in three general practices: value of on-site physiotherapy. Br J Gen Pract. 1993; 43(367):61–4.
12 Morris CD, Hawes SJ. The value of accident and emergency based physiotherapy services. J Accid Emerg Med. 1996;13(2):111–3.
13 Taylor NF, Norman E, Roddy L, Tang C, Pagram A, Hearn K. Primary contact physiotherapy in emergency departments can reduce length of stay for patients with peripheral musculoskeletal injuries compared with secondary contact physiotherapy: a prospective non-randomised controlled trial. Physiotherapy. 2011;97(2):107–14.
14 Bethel J. The role of the physiotherapist practitioner in emergency departments: a critical appraisal. Emerg Nurse. 2005;13(2):26–31.
15 Kilner E. What evidence is there that a physiotherapy service in the emergency department improves health outcomes? A systematic review. J Health Serv Res Policy. 2011;16(1):51–8.
16 Lau PMY, Chow DHK, Pope MH. Early physiotherapy intervention in an accident and emergency department reduces pain and improves satisfaction for patients with acute low back pain: a randomized trial. Aust J Physiother. 2008;54(4):243–9.
17 Zigenfus GC, Yin J, Giang GM, Fogarty WT. Effectiveness of early physical therapy in the treatment of acute low back musculoskeletal disorders. J Occup Environ Med. 2000;42(1):35–9.
Received August 28, 2016
Accepted after revision January 20, 2017
World J Emerg Med 2017;8(2):110–115
10.5847/wjem.j.1920–8642.2017.02.005
Pothiawala Sohil, Email: drsohilpothiawala@yahoo.com
 World journal of emergency medicine2017年2期
World journal of emergency medicine2017年2期
- World journal of emergency medicine的其它文章
- Improving hospital-based trauma care for road traff i c injuries in Malawi
- Patient tracking in earthquake emergency response in Iran: A qualitative study
- Prediction of motor recovery after ischemic stroke using diffusion tensor imaging: A meta-analysis
- Fibrinogen degradation product levels on arrival for trauma patients requiring a transfusion even without head injury
- Trend of blood lactate level in acute aluminum phosphide poisoning
- The RAMA Ped Card: Does it work for actual weight estimation in child patients at the emergency department
