Improving hospital-based trauma care for road traff i c injuries in Malawi
Linda Chokotho, Wakisa Mulwafu, Isaac Singini, Yasin Njalale, Kathryn H. Jacobsen
1Beit Cure Hospital, Blantyre, Malawi
2Department of Surgery, College of Medicine, University of Malawi, Blantyre, Malawi
3Johns Hopkins Project, Blantyre, Malawi
4Blantyre Adventist Hospital, Blantyre, Malawi
5Department of Global & Community Health, George Mason University, Fairfax, Virginia, USA
Improving hospital-based trauma care for road traff i c injuries in Malawi
Linda Chokotho1, Wakisa Mulwafu2, Isaac Singini3, Yasin Njalale4, Kathryn H. Jacobsen5
1Beit Cure Hospital, Blantyre, Malawi
2Department of Surgery, College of Medicine, University of Malawi, Blantyre, Malawi
3Johns Hopkins Project, Blantyre, Malawi
4Blantyre Adventist Hospital, Blantyre, Malawi
5Department of Global & Community Health, George Mason University, Fairfax, Virginia, USA
BACKGROUND: The mortality rate from road traffic injuries has increased in sub-Saharan Africa as the number of motor vehicles increase. This study examined the capacity of hospitals along Malawi's main north-south highway to provide emergency trauma care.
METHODS: Structured interviews and checklists were used to evaluate the infrastructure, personnel, supplies, and equipment at all four of Malawi's central hospitals, ten district hospitals, and one mission hospital in 2014. Most of these facilities are along the main north-south highway that spans the country.
RESULTS: Between July 2013 and March 2014, more than 9 200 road traffic injuries (RTIs) and 100 RTI deaths were recorded by the participating hospitals. All of the hospitals reported staff shortages, especially during nights and weekends. Few clinicians had completed formal training in emergency trauma management, and healthcare workers reported gaps in knowledge and skills, especially at district hospitals. Most central hospitals had access to the critical supplies and medications necessary for trauma care, but district hospitals lacked some of the supplies and equipment needed for diagnosis, treatment, and personal protection.
CONCLUSION: The mortality and disability burden from road traff i c injuries in Malawi (and other low-income countries in sub-Saharan Africa) can be reduced by ensuring that every central and district hospital has a dedicated trauma unit with qualified staff who have completed primary trauma care courses and have access to the equipment necessary to save lives.
Traffic accidents; Emergency medical services; Developing countries; Road traff i c injuries; Sub-Saharan Africa
INTRODUCTION
Malawi is a small, low-income country in southern Africa. Road traffic injuries (RTIs) are a common cause of hospital visits in Malawi,[1–3]and they are also the leading cause of adult injury-related deaths.[4]Malawi has one of the world's highest rates of traff i c-related fatalities.[5]The annual traff i c-related mortality rate of 35 per 100 000 residents is the highest in sub-Saharan Africa,[6]a world region with a higher than average burden from RTIs.[7,8]And that rate is not decreasing. Instead, the road traffic fatality rate has increased as the number of motor vehicles on the road has increased.[9,10]About 5 700 of Malawi's 17 million residents died from RTIs in 2015, even though there is only one motor vehicle on the road for every 40 residents.[10]As the burden from RTIs increases in Malawi and other countries in sub-Saharan Africa, thereis a need to improve the quality of trauma care offered by hospitals along major roads. The goal of this study was to assess the facilities' infrastructure, personnel, and supplies and equipment of hospitals along the North–South Corridor in Malawi to respond to emergency RTIs in order to identify critical areas for improvement in trauma care.
METHODS
Fifteen hospitals were included in this evaluation: all four central hospitals in the country, the ten district hospitals that are along the M1 highway, and one mission hospital that is along the M1 highway. All 15 health facilities receive patients with transport-related injuries. Four of the hospitals were in the Northern Region, four in the Central Region, and seven in the Southern Region (Figure 1).
Checklists for evaluating the facilities, personnel, and supplies and equipment of the accident and emergency (A&E) departments at each facility were derived from the World Health Organization (WHO) Guidelines for Essential Trauma Care.[11]A classification of adequate indicates something that is present and used appropriately. A classification of inadequate indicates something that usually is not present. A classif i cation of partially adequate indicates something that is present sometimes but not always or one that is present but not readily available.
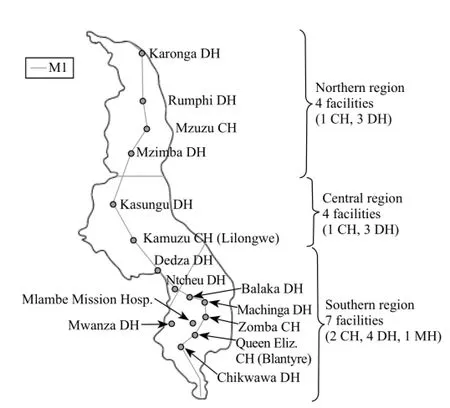
Figure 1. Locations of the participating hospitals in Malawi. Thirteen of the 15 hospitals are located along the M1 highway, which is the major north-to-south highway in Malwai. CH: central hospital; DH: district hospital.
Additionally, availability of trauma registries and cross-sectional data on the number of trauma patients treated at each facility were tabulated. These hospital-level data were acquired through structured interviews with hospital directors, heads of departments (physicians), and matrons (heads of nursing staff). All clinicians and other hospital staff who volunteered to provide responses to the knowledge and skills questions in the surveys consented to their participation; no individually-identifying information was collected. The study protocol was approved by the Malawi Ministry of Health prior to implementation.
All data were collected between April and June 2014. The responses to the questionnaire items were entered into Microsoft Access databases with built-in logic checks to ensure the quality of the data, then were cleaned and analysed using Stata software.
RESULTS
Burden of road trauma
In the nine months from July 2013 to March 2014, more than 9 200 RTI cases and more than 100 RTI deaths were recorded by the participating health facilities. This totally included more than 2 300 RTIs in the northern region, more than 3 800 in the central region, and nearly 3 100 in the southern region. However, only two of the facilities (Kamuzu Central Hospital in Lilongwe and Queen Elizabeth Central Hospital in Blantyre) had formal trauma registries. The other central and district hospitals maintain registers for all patients, but these registers rarely include complete information about the types and causes of various injuries. Thus, the count of RTIs treated at the participating facilities is likely incomplete. Also, the number of fatalities does not reflect the actual number of road traffic deaths in the areas served by participating hospitals. The only cases included in the counts are the minority of fatalities that were registered by hospitals. Deaths occurring at the site of a collision are not included in hospital records.
Infrastructure
Four of the 15 participating facilities had dedicated accident and emergency (A&E) units. These include three central hospitals (Mzuzu Central Hospital in the northern region, Kamuzu Central Hospital in Lilongwe, and Queen Elizabeth Central Hospital in Blantyre, which has separate A&E units for adults and children) and one district hospital (Rumphi District Hospital, in the northern region). Zomba Central Hospital has nodedicated accidents and emergency (A&E) unit; trauma patients are treated at the surgical outpatient clinic. The other district hospitals either use one room as a makeshift A&E unit or have a theatre for minor operations that is used for treatment of trauma and emergency surgical patients. As of 2014, none of the fifteen hospitals had a formal disaster management plan.
Personnel
Trauma care units in Malawi are supposed to be staffed by five types of clinicians: medical assistants (MAs), nurses, clinical officers (COs), medical officers, and specialist doctors. MAs complete a 2-year postsecondary certificate in clinical medicine. Nurses typically have 3 to 4 years of postsecondary training. COs earn a 3-year postsecondary diploma in clinical medicine. Medical off i cers earn an MBBS in clinical medicine after 6 years of study, and are qualified (licensed) physicians with no specialist training. To become a surgical specialist, an additional 5 years of training must be completed after becoming qualif i ed as a general physician.
All 15 hospitals in this study reported having too few staff to adequately care for trauma patients (Table 1). At the four central hospitals, all five types of clinicians were on staff, but there were not sufficient numbers of personnel to have the appropriate level of staff i ng at all times. Shortages were much more pronounced at district hospitals. At district hospitals, nearly all daytime trauma cases are managed by one or two general or orthopedic COs with the support of nurses and MAs when available. During nights and weekends, the casualty units at district hospitals are usually staffed by an MA who is on call for all cases not just trauma, and nurses are not always available because they are assigned to other units. Some hospitals reported that because of nurse staffing shortages there are times when minimally-trained patient attendants rather than nurses are called on to assist with the care of trauma patients. Only two of the ten district hospitals in this study reported having a medical off i cer assigned to the casualty unit, and none of the district hospitals reported having a specialist doctor on staff.
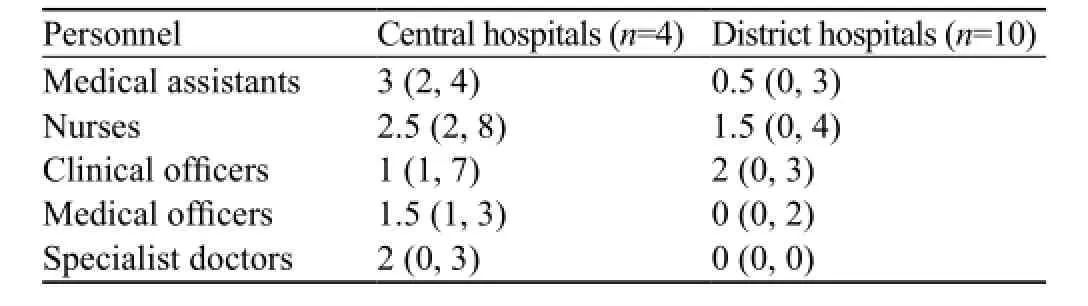
Table 1. Mean (minimum, maximum) number of clinical staff serving in the trauma care unit at central hospitals and district hospitals in Malawi
Almost none of the trauma care personnel at any district hospital had completed coursework focused on emergency trauma management. A primary trauma care course had been offered in Malawi for the first time just before the site visits for this study; only about 35 participants from across all of Malawi had completed it, and almost none of those clinicians worked at one of the 15 hospitals participating in this study. Most of the lead trauma care providers at central hospitals were conf i dent with resuscitation skills and with airway and breathing support, such as insertion of endotracheal tubes and chest drains. Most district hospital staff—generally orthopedic clinical officers with no formal training on emergency care procedures—were not confident in their ability to perform these skills. Most trauma care personnel at both central and district hospitals were confident about inserting peripheral intravenous lines, but almost all lacked knowledge about fl uid resuscitation protocols and circulation monitoring. Knowledge and skills related to abdominal injuries and the management of extremity, spine, head, and neck injuries also varied by facility type. While orthopedic clinical officers were confident in their ability to perform fasciotomies and closed limb immobilization, other clinicians were not.
Supplies and equipment
We conducted inventories at the participating hospitals with a focus on the tools necessary for acute resuscitation of trauma victims. The central hospitals had adequate or partially adequate supplies of oral and nasal airway devices, bags/valves/masks, suction devices, Yankauer or other stiff suction tips, laryngoscopes, endotracheal tubes, stethoscopes, oxygen, needles and syringes, chest tubes, pulse oximeters, intravenous (IV) solution, blood for transfusion, and urinary catheters (Table 2). Only one central hospital had an arterial blood gas machine (located in the paediatric A&E department) and a mechanical ventilator (located in the adult A&E department), and the ventilator was reported as never being used. The central hospitals had inadequate ability to conduct electronic cardiac monitoring.
The district hospitals had adequate access to basic clinical tools such as stethoscopes, blood pressure cuffs, IV solution, and urinary catheters, but they consistently reported inadequate supplies of airway and breathing equipment such as oral and nasal airway devices, bags/ valves/masks, equipment for suctioning, laryngoscopes, endotracheal tubes, chest tubes, and pulse oximeters. Even when these types of equipment were available in operating theatres, they were usually not accessible tothe staff working in casualty departments. Also, in some district hospitals equipment donations were being stored because there was no room for them in the treatment areas. Thus, sometimes on-site equipment was not available for use.
For diagnosis, nearly all the hospitals had plain X-ray films and functional X-ray machines. Only one central hospital had a CT scanner and only one had an MRI. All district and central hospitals had adequate ability to conduct haemoglobin and blood glucose tests. Central hospitals had functional analytic chemistry machines, but they were often unable to conduct electrolyte and serum lactate testing because the necessary reagents were out of stock. District hospitals generally had inadequate ability to conduct electrolyte tests.
All the hospitals reported adequate stocks of anaesthetics, anticonvulsants, analgesics, antiseptic solutions, intravenous fluids such as normal saline and dextrose, and prophylactic medications. The opioid antidote naloxone and the osmotic diuretic mannitol were only available in one central hospital. Although most hospitals had antibiotics such as ceftriaxone, gentamicin, metronidazole, and benzyl penicillin in stock, supplies were reported to be unreliable and to run low at the end of the time periods prior to monthly restocking.
Access to personal protection equipment was only partially adequate. Most facilities had sufficient stocks of surgical gloves, but utility gloves for use by cleaning staff were not available. Goggles and gowns were typically available only in surgical theatres and not in the other units treating trauma patients. District and central hospitals reported similar supply limitations, but district hospitals reported more access to gowns, even though the gown supply was still inadequate. Staff from all facilities reported inadequate training in universal precautions. Only one central hospital offered routine training in prevention of bloodborne diseases to all staff. All hospitals offered HIV post-exposure prophylaxis (PEP) to staff if they suffered a needlestick or other exposure.
The inventories of safety equipment found that sharps disposal containers (typically improvised from repurposed cardboard boxes) and incinerators were present and being used appropriately at all district hospitals. However, two of the central hospitals did not have functioning incinerators at the time of the survey. At all district hospitals, biological waste was disposed of in "placenta pits". Medical waste bins were in short supply, and biohazard materials were not always placed in dedicated and appropriately labelled waste bins separate from other rubbish.

Table 2. Availability of supplies and equipment at central hospitals and district hospitals in Malawi
DISCUSSION
Our analysis of hospital-based trauma care in hospitals across Malawi showed a substantial burden from road traffic injuries; the need to address staffing and equipment shortages, especially at district hospitals; and the need for expanded access to trauma care training for all clinical staff at central and district hospitals. Few hospitals have dedicated trauma units, and few maintain good-quality trauma registers.
Restructuring the hospital system in Malawi to ensure that every central and district hospital has a dedicated trauma unit with qualif i ed staff would improve the survival and outcomes of injured patients. While it may be impossible given resource limitations for all hospitals to offer specialist care, all district hospitals should be prepared to manage mild and moderate injuries and to provide resuscitation and stabilization of the more severe trauma cases that require referral to a central hospital. At central hospitals, the goal should be to grow the existing emergency units into higher-level trauma centres that are prepared to provide quality specialist care for all referral cases. In Malawi, accreditation ofthese emergency departments and trauma centres could be overseen by the Malawi Medical Council, which would use internationally-validated assessment tools to ensure that best practices for staffing, equipment, and other aspects of trauma care in low- and middleincome countries (LMICs) are being implemented. The accreditation process could also ensure adequate training in advanced trauma care for clinicians in the units, and it would mandate improved data collection and evaluation procedures that would enable better monitoring of hospital-based trauma care.
In terms of training, Malawi is somewhat unique in its reliance on mid-level clinical officers and medical assistants to provide the majority of trauma care. These clinicians are required to provide initial stabilisation of all trauma patients, including severely injured patients, and they sometimes also provide definitive treatment without the support of specialists. There is a need to strengthen the trauma training clinical officers receive during their studies at the Malawi College of Health Sciences. Advanced Trauma Life Support (ATLS) training may improve knowledge of clinicians in lowand middle-income countries; however, the courses can be costly, and without improved access to equipment they may yield limited improvements in patient outcomes.[12,13]A Primary Trauma Care (PTC) course emphasizing the systematic approaches such as airway management, care of chest injuries, control of major haemorrhage, and care of paediatric trauma patients that are proven to reduce morbidity and mortality in resource-limited settings may be the most appropriate option in low-income countries like Malawi.[14–16]Such courses should be mandatory for all clinical staff assigned to emergency departments and trauma centres, and recertif i cation every three years would help ensure that all practitioners remain up-to-date on knowledge and skills. The Ministry of Health (MOH) employs the majority of healthcare workers in Malawi, and is empowered to mandate requirements for licensure and continuing education.
Although this evaluation focused on Malawi, similar challenges associated with limited personnel and equipment have been reported across the sub-Saharan African region.[17–21]The need to improve trauma care for RTIs in LMICs is widely recognized, but limited progress has been made thus far.[22,23]
One limitation of this cross-sectional analysis is that it focused on hospitals located near the main north-south highway in Malawi. Almost all the surveyed hospitals were within 5 km of the highway, and their experience may not reflect the situation at hospitals located 30 km or farther away from the main transportation corridor. As national emergency medicine plans are developed and implemented, it will be important to incorporate the perspectives of healthcare providers in more remote and rural areas. A survey instrument such as the International Assessment of Capacity for Trauma (INTACT) or the PIPES (personnel, infrastructure, equipment, and supplies) Index may be useful for comparing strengths and needs in various areas.[24]
CONCLUSION
This study has identif i ed the strengths and limitations of the trauma care offered by hospitals along the major highway in Malawi. Addressing the key gaps in capacity identified in this analysis is necessary for reducing the burden from road traffic injuries and other types of trauma in the country. To more completely reduce the burden from preventable injury mortality and disability, these hospital-based improvements must be accompanied by similar progress in injury prevention, prehospital care, and rehabilitation. However, since a comprehensive trauma care system relies on consistently high-quality inhospital emergency care, the emergency department is an appropriate fi rst place to implement quality improvement plans.
Funding: The study was funded by a grant from the World Bank. Ethical approval: The study was approved by Ministry of Health, Malawi.
Conflicts of interest: The authors declare that no competing interest and no personal relationships with other people or organizations that could inappropriately inf l uence their work.
Contributors: LC led the design of the study and data collection. LC, KHJ, and WM drafted the manuscript. All authors contributed to the interpretation of the results and the critical revision of the manuscript.
REFERENCES
1 Chokotho L, Mulwafu W, Jacobsen KH, Pandit H, Lavy C. The burden of trauma in four rural district hospitals in Malawi: a retrospective review of medical records. Injury. 2014;45(12):2065–70.
2 Samuel JC, Akinkuotu A, Villaveces A, Charles AG, Lee CN, Hoffman IF, et al. Epidemiology of injuries at a tertiary care center in Malawi. World J Surg. 2009;33(9):1836–41.
3 Yu KL, Bong CN, Huang MC, Chen CC, Ko YC, Chang PY, et al. The use of hospital medical records for child injury surveillance in northern Malawi. Trop Doct. 2009;39(3):170–2.
4 Chasimpha S, McLean E, Chihana M, Kachiwanda L, Koole O, Tafatatha T, et al. Patterns and risk factors for deaths fromexternal causes in rural Malawi over 10 years: a prospective population-based study. BMC Public Health. 2015;15:1036.
5 Sivak M, Schoettle B. Mortality from road crashes in 193 countries: a comparison with other leading causes of death. Ann Arbor: University of Michigan Transportation Research Institute; 2014.
6 World Health Organization. World health statistics 2016: monitoring health for the SDGs. Geneva: WHO; 2016.
7 Chen G. Road traffic safety in African countries: status, trend, contributing factors, countermeasures and challenges. Int J Inj Contr Saf Promot. 2010;17(4):247–55.
8 World Health Organization. Global status on road traff i c safety: time for action. Geneva: WHO; 2013.
9 Olukoga A. Trends in road traff i c crashes, casualties and fatalities in Malawi. Trop Doct. 2007;37(1):24–8.
10 World Health Organization. Global status report on road safety 2015. Geneva: WHO; 2015.
11 Mock C, Lormand JD, Goosen J, Joshipura M, Peden M. Guidelines for essential trauma care. Geneva: World Health Organization; 2004.
12 Jayaraman S, Sethi D, Chinnock P, Wong R. Advanced trauma life support training for hospital staff. Cochrane Database Syst Rev. 2014;(8):CD004173.
13 Mohammad A, Branicki F, Abu-Zidan FM. Educational and clinical impact of Advanced Trauma Life Support (ATLS) courses: a systematic review. World J Surg. 2014;38(2):322–9.
14 Nogaro MC, Pandit H, Peter N, Le G, Oloruntoba D, Muguti G, et al. How useful are primary trauma care courses in sub-Saharan Africa? Injury. 2015;46(7):1293–8.
15 Peter NA, Pandit H, Le G, Muguti G, Lavy C. Delivering trauma training to multiple health-worker cadres in nine sub-Saharan African countries: lessons learnt from the COOL programme. Lancet. 2015;385 Suppl 2:S45.
16 Quansah R, Abantanga F, Donkor P. Trauma training for nonorthopaedic doctors in low- and middle-income countries. Clin Orthop Relat Res. 2008;466(10):2403–12.
17 Chokotho L, Jacobsen KH, Burgess D, Labib M, Le G, Lavy CBD, et al. Trauma and orthopaedic capacity of 267 hospitals in east, central, and southern Africa. Lancet. 2015;385 Suppl 2:S17.
18 Chokotho L, Jacobsen KH, Burgess D, Labib M, Le G, Peter N, et al. A review of existing trauma and musculoskeletal impairment (TMSI) care capacity in east, central, and southern Africa. Injury. 2016;47(9):1990–5.
19 Hanche-Olsen TP, Alemu L, Viste A, Wisborg T, Hansen KS. Trauma care in Africa: a status report from Botswana, guided by the World Health Organization's "Guidelines for Essential Trauma Care." World J Surg. 2012;36(10):2371–83.
20 Kouo-Ngamby M, Dissak-Delon FN, Feldhaus I, Julliard C, Stevens KA, Ekeke-Monono M. A cross-sectional survey of emergency and essential surgical care capacity among hospitals with high trauma burden in a Central African country. BMC Health Serv Res. 2015;15:478.
21 Wesson HKH, Bachani AM, Wekesa JM, Mburu J, Hyder AA, Stevens KA. Assessing trauma care at the district and provincial hospital levels: a case study of hospitals in Kenya. Injury. 2013; 44(Suppl 4):S75–80.
22 Moroz PJ, Spiegel DA. The World Health Organization's action plan on the road traff i c injury pandemic: is there any action for orthopaedic trauma surgeons? J Orthop Trauma. 2014;28(Suppl 1):S11–4.
23 Stewart BT, Gyedu A, Quansah R, Addo WL, Afoko A, Agbenorku P, et al. District-level hospital trauma care audit filters: Delphi technique for defining context-appropriate indicators for quality improvement initiative evaluation in developing countries. Injury. 2016;47(1):211–9.
24 Wong EG, Gupta S, Deckelbaum DL, Razek T, Kamara TB, Nwomeh BC, et al. The International Assessment of Capacity for Trauma (INTACT): an index for trauma capacity in low-income countries. J Surg Res. 2014;190(2):522–7.
Received July 9, 2016
Accepted after revision January 26, 2017
World J Emerg Med 2017;8(2):85–90
10.5847/wjem.j.1920–8642.2017.02.001
Linda Chokotho, Email: linda.chokotho@cureinternational.org
 World journal of emergency medicine2017年2期
World journal of emergency medicine2017年2期
- World journal of emergency medicine的其它文章
- Patient tracking in earthquake emergency response in Iran: A qualitative study
- Prediction of motor recovery after ischemic stroke using diffusion tensor imaging: A meta-analysis
- Potential impact of early physiotherapy in the emergency department for non-traumatic neck and back pain
- Fibrinogen degradation product levels on arrival for trauma patients requiring a transfusion even without head injury
- Trend of blood lactate level in acute aluminum phosphide poisoning
- The RAMA Ped Card: Does it work for actual weight estimation in child patients at the emergency department
